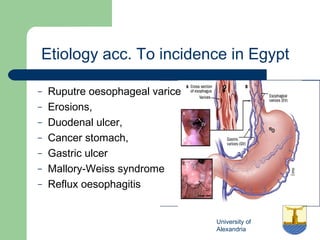
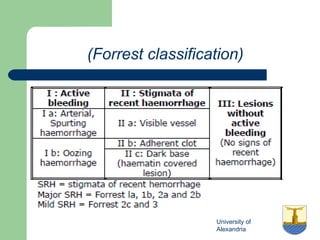
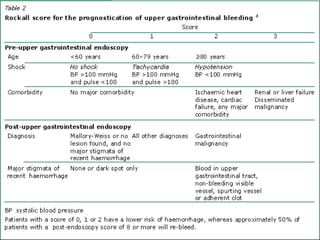
This document discusses upper gastrointestinal bleeding, including its definition, etiologies, presentations, and management. The main causes of upper GI bleeding are esophageal and gastric varices, peptic ulcers, erosive gastritis, and Dieulafoy's lesions. Clinical manifestations include melena, hematemesis, and hematochezia. Management involves resuscitation, endoscopy to determine the source of bleeding, and treatments specific to the cause such as band ligation for varices, sclerotherapy for ulcers, and antisecretory drugs for erosions. Refractory bleeding may require transjugular intrahepatic portosystemic shunt placement or surgery.