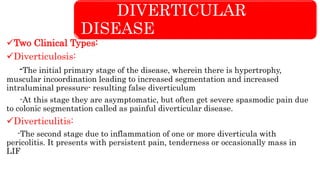
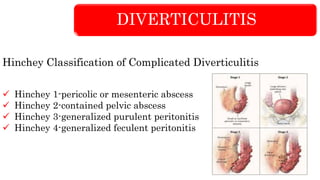
The document discusses diverticular disease as a cause of lower gastrointestinal hemorrhage, detailing its types, clinical features, investigations, and management options. It highlights the etiology and complications associated with diverticulosis and diverticulitis, including symptoms, diagnostic procedures, and treatment approaches. Key clinical vignettes illustrate typical patient presentations and the necessary diagnostic and therapeutic strategies.