This document provides an overview of optimizing critical care ventilation based on ventilator waveforms. It discusses:
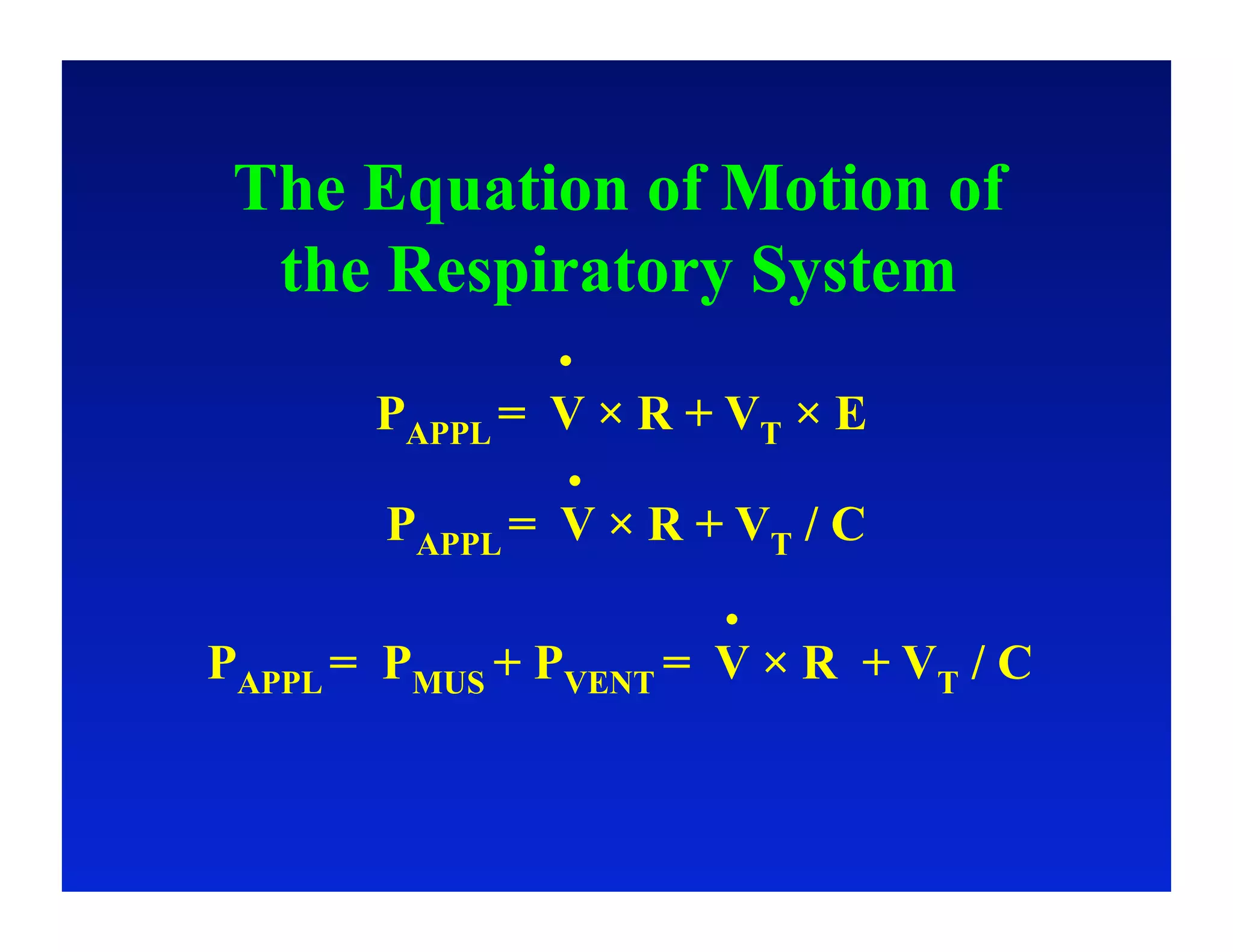
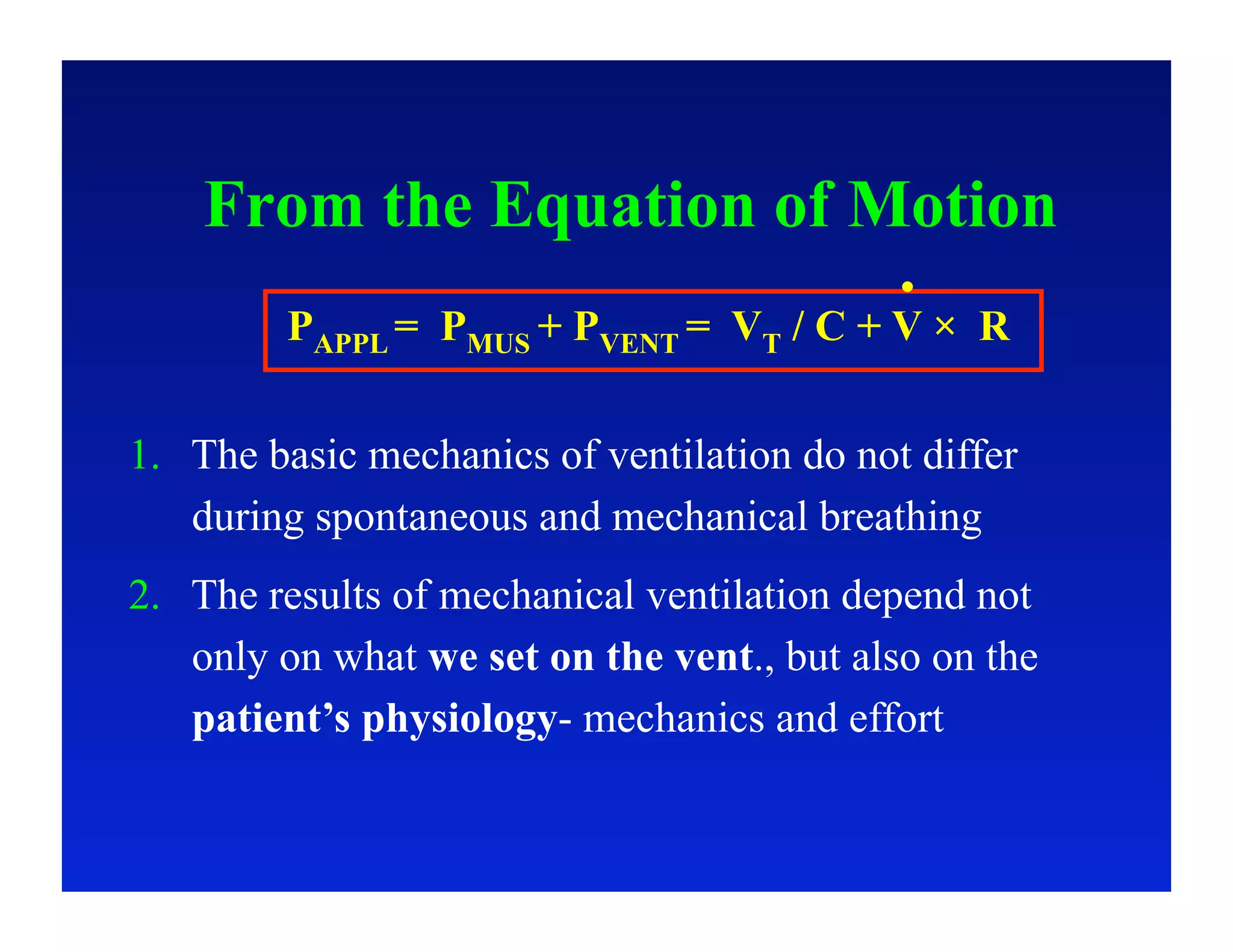
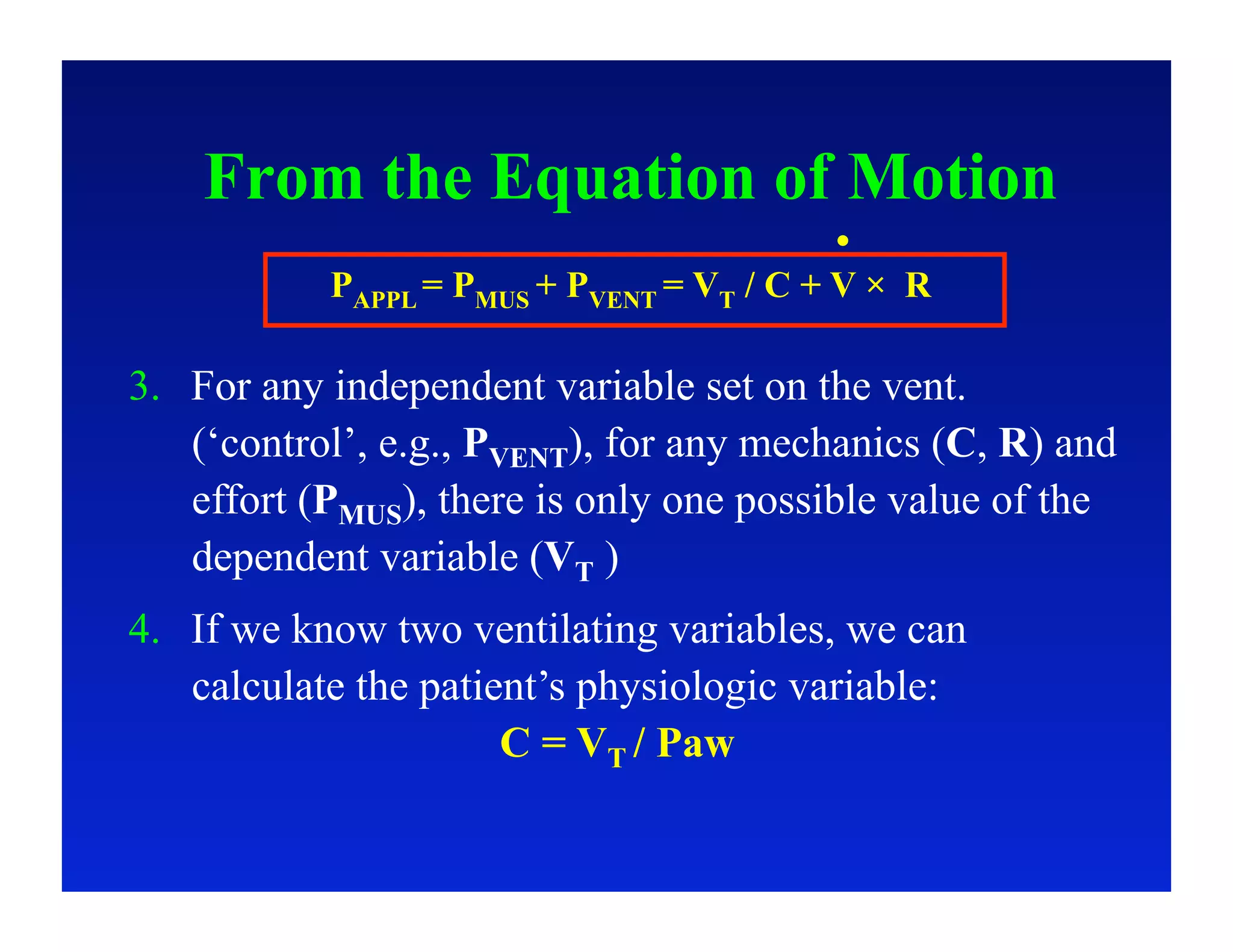
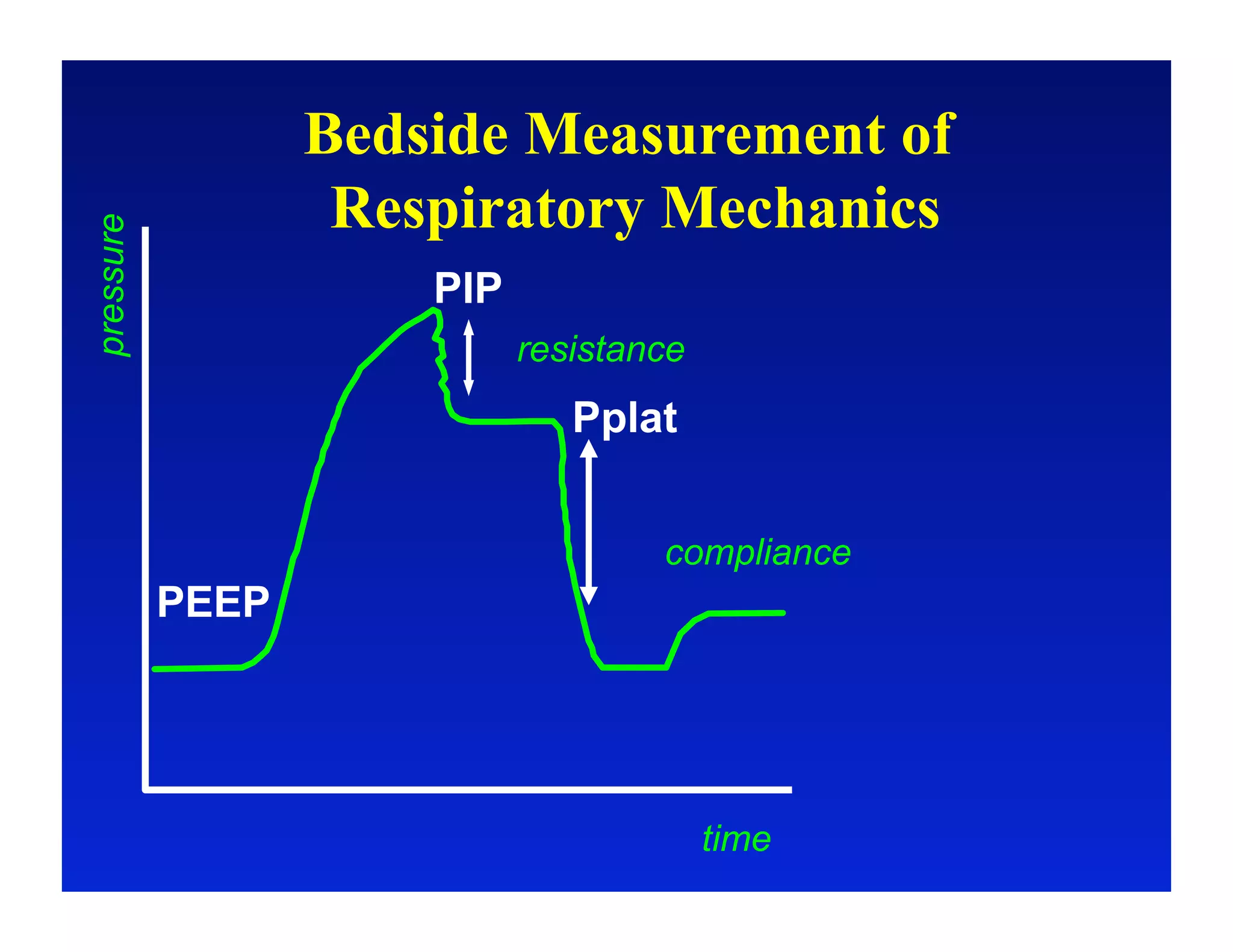
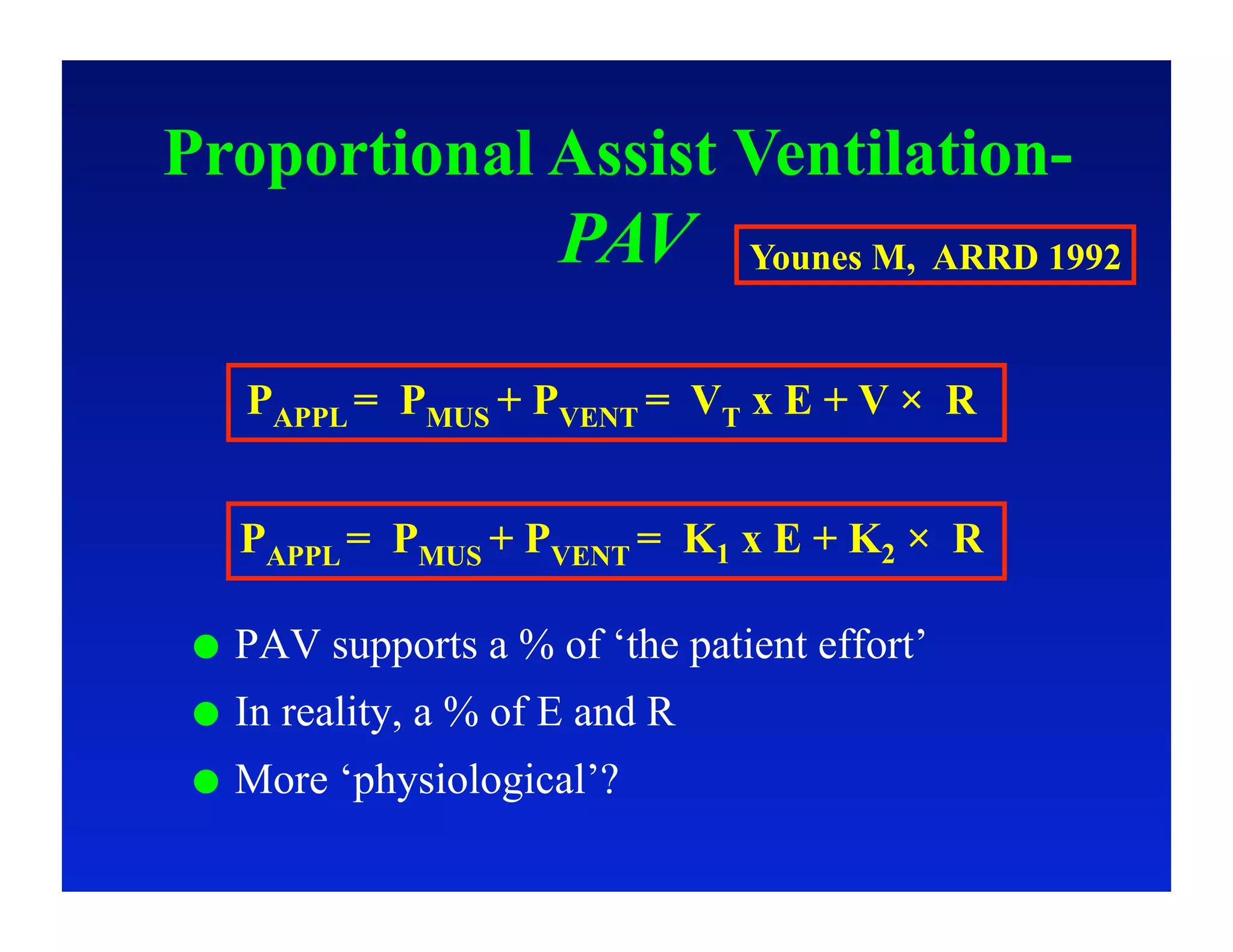
1. The basic physiology of ventilation and the equation of motion of the respiratory system.
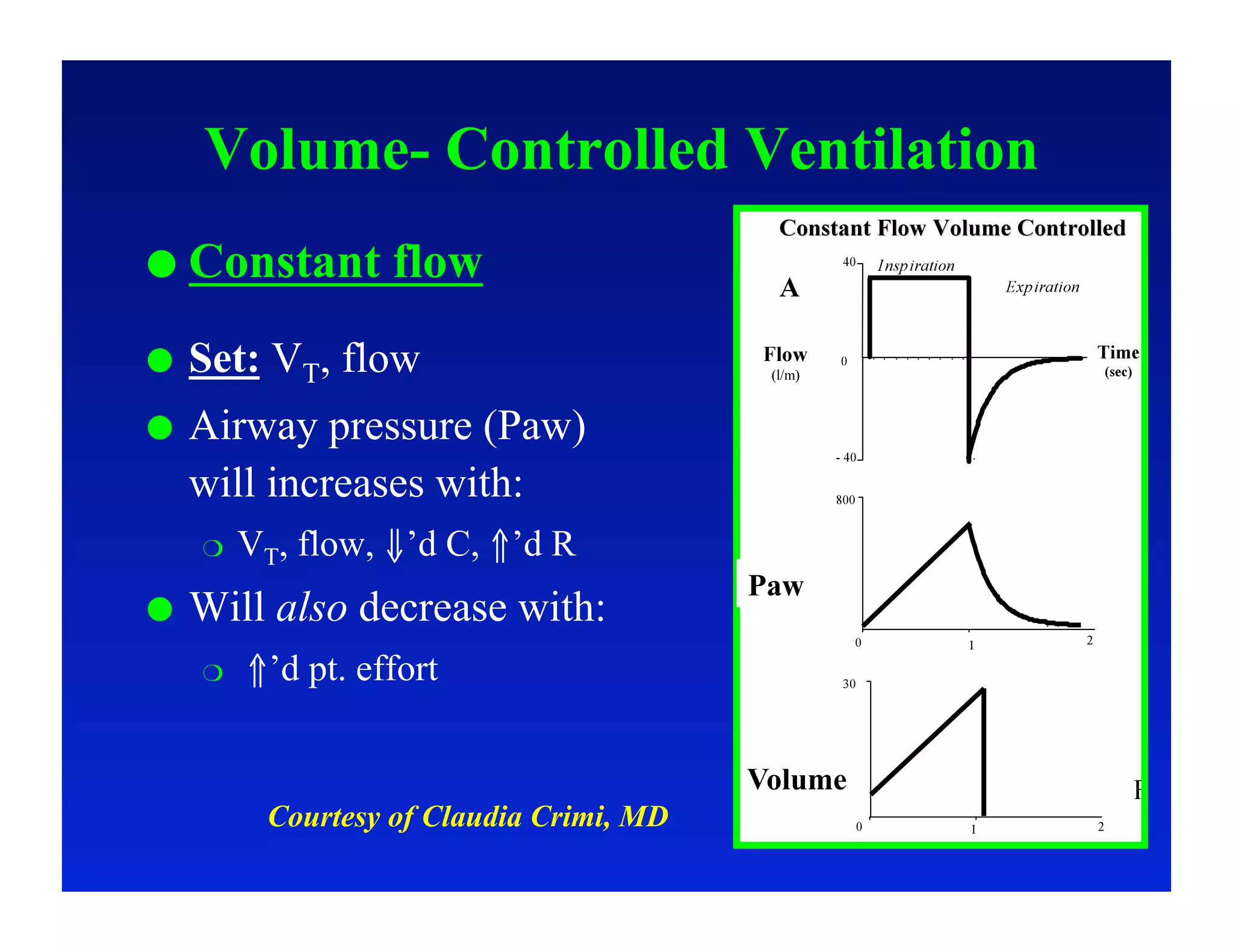
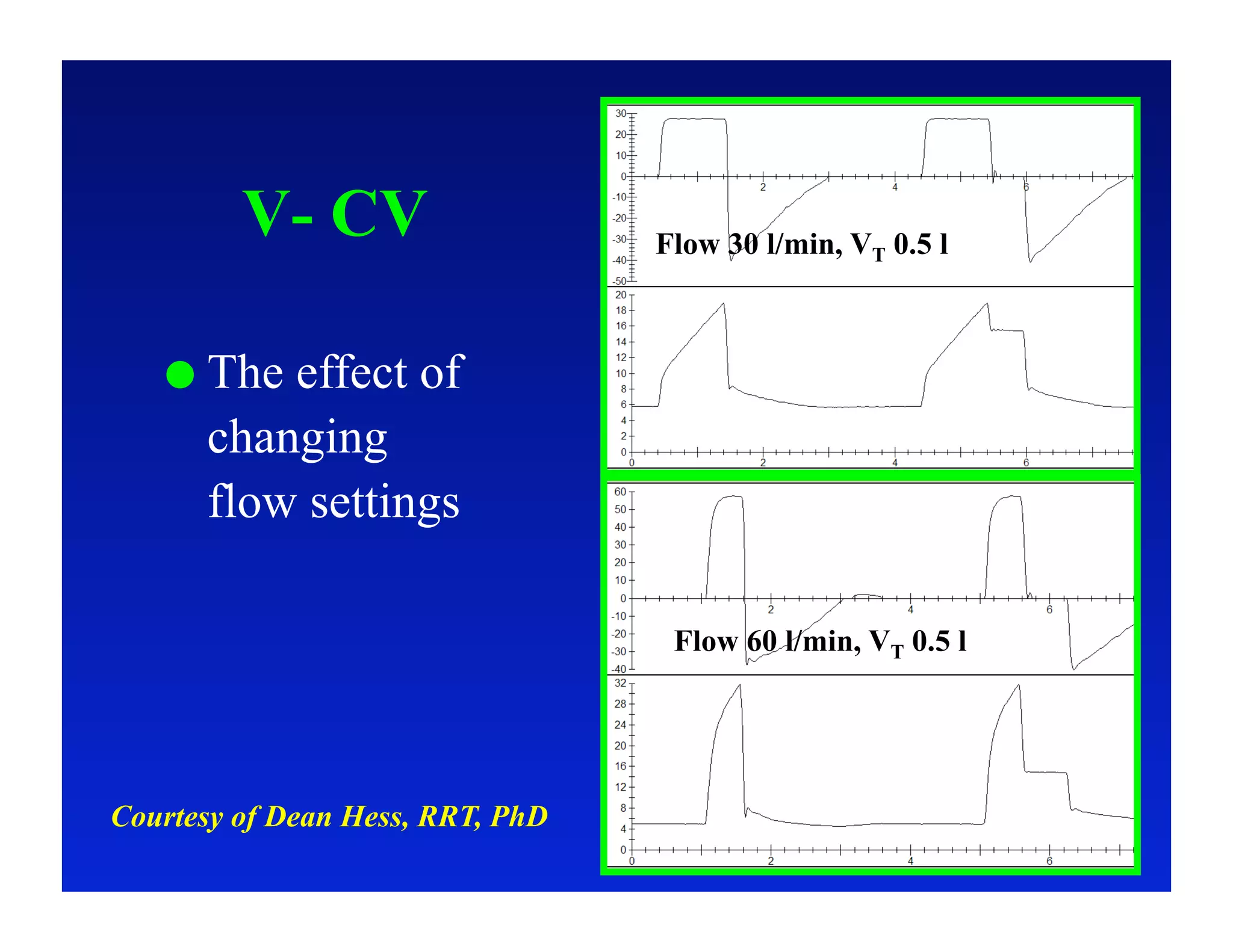
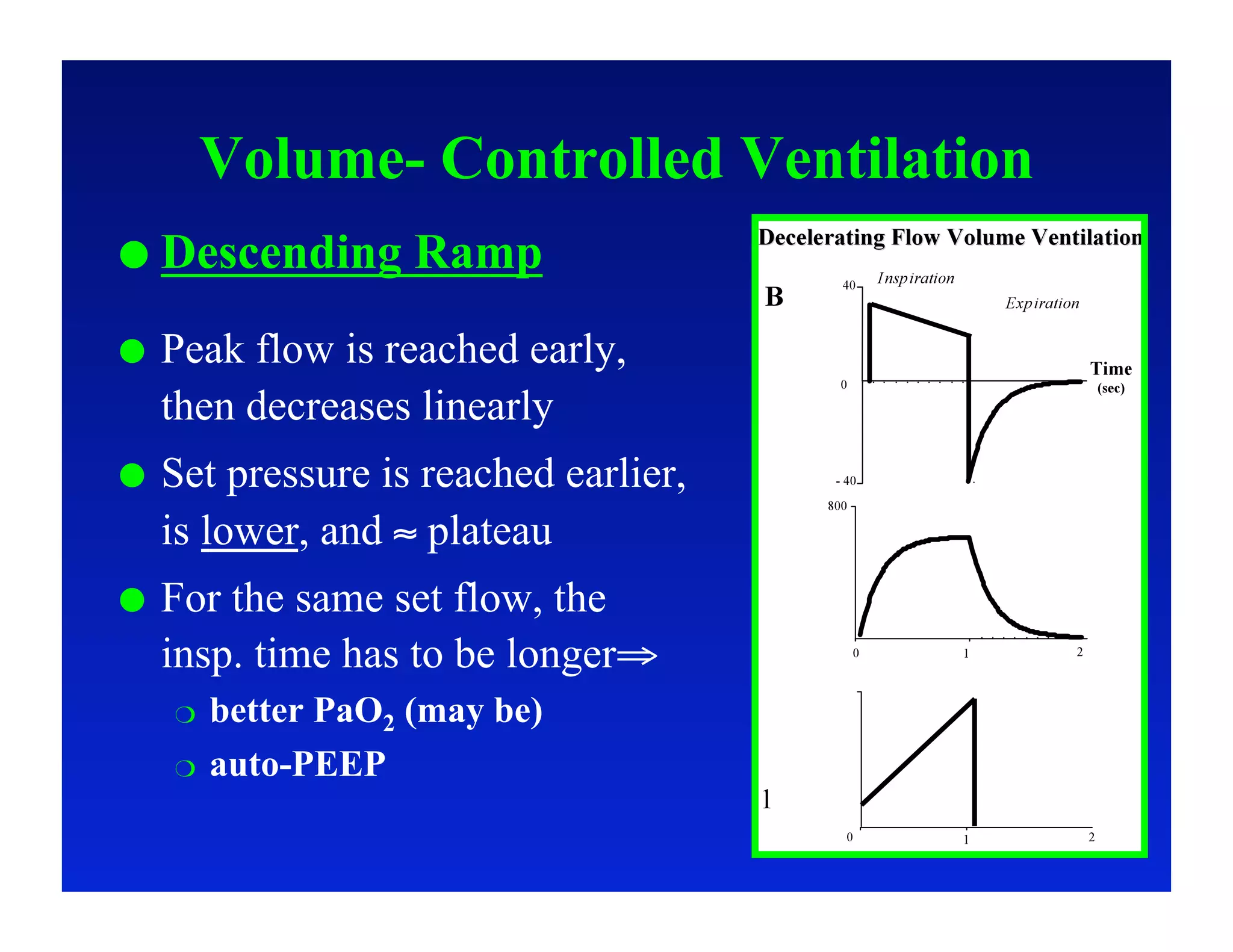
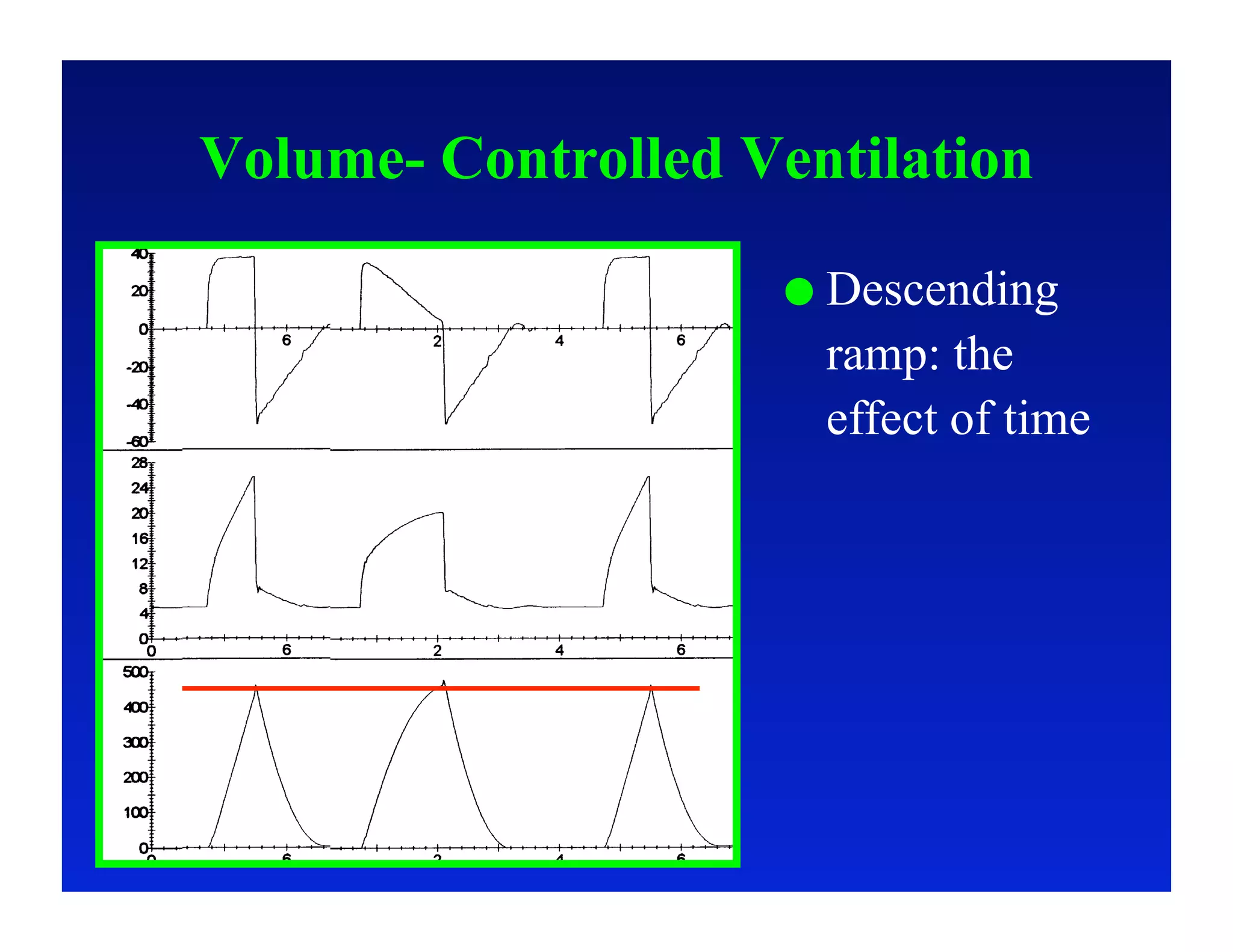
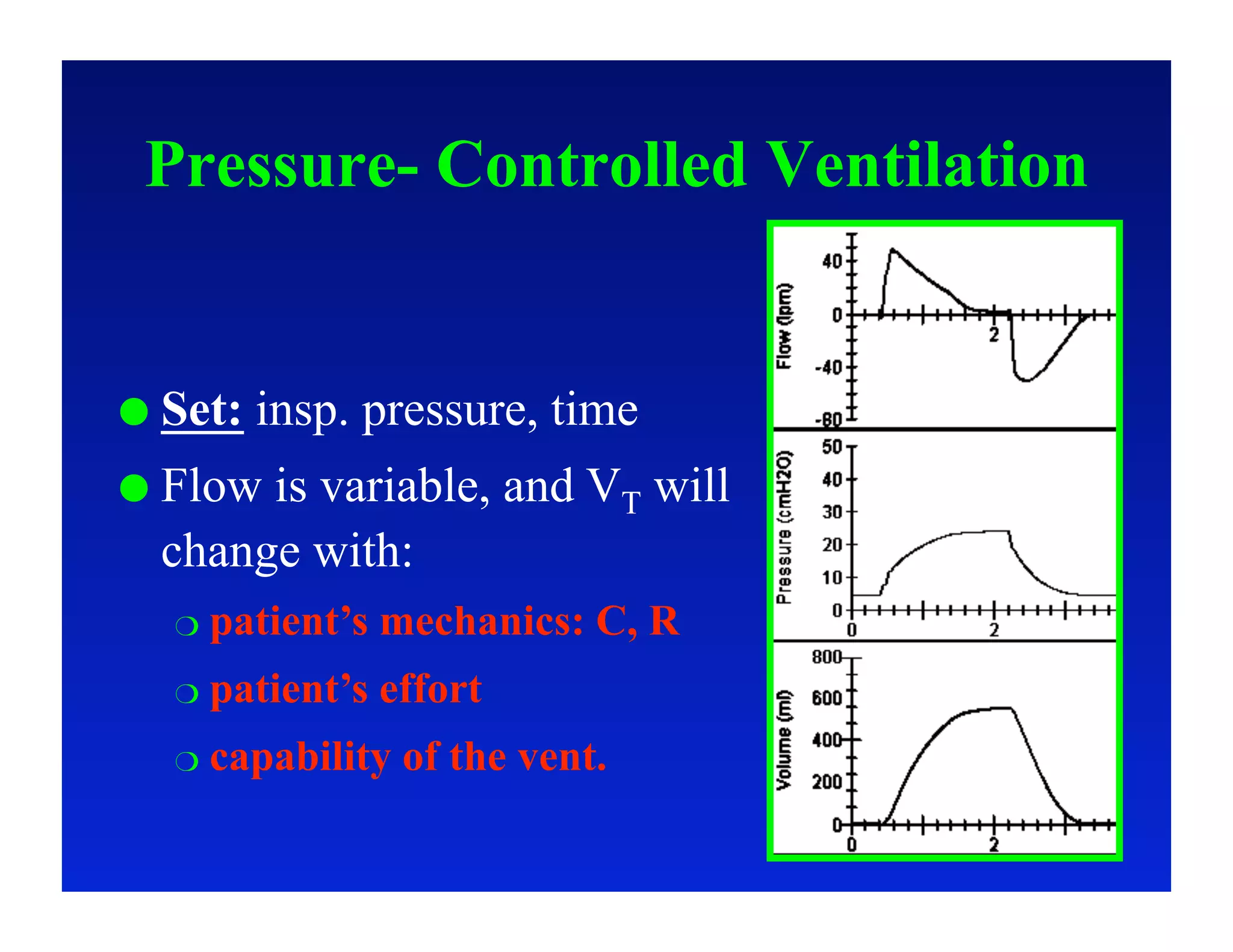
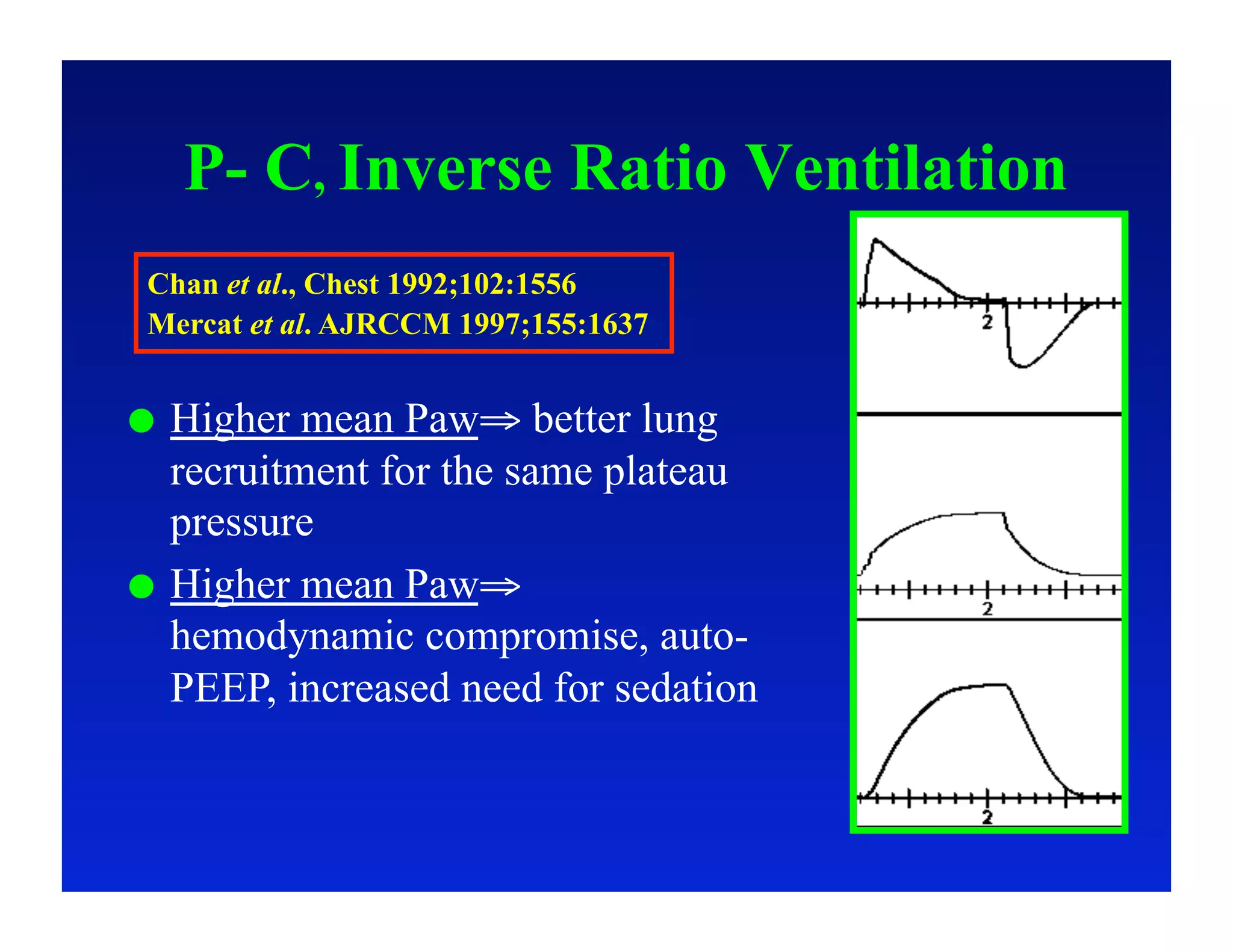
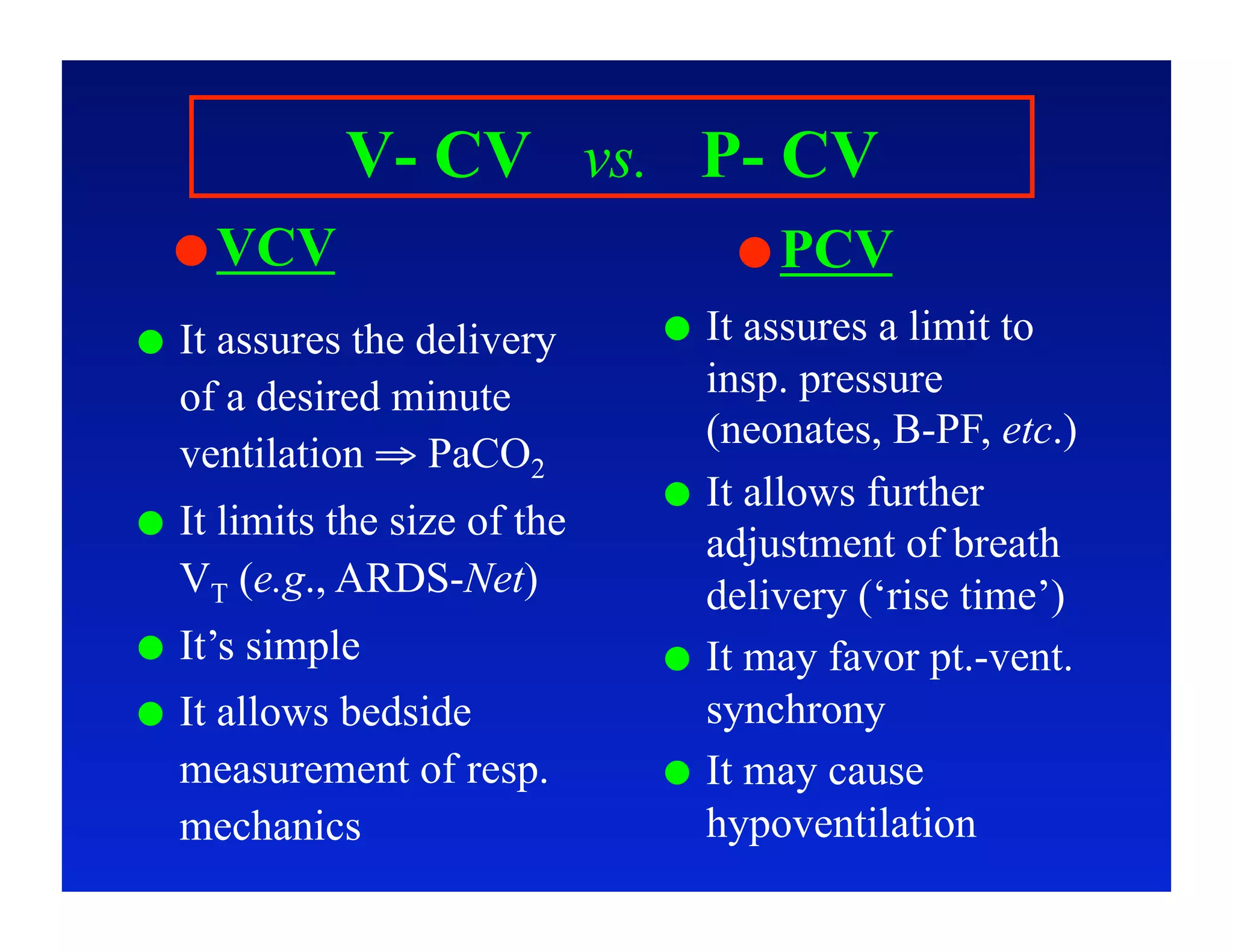
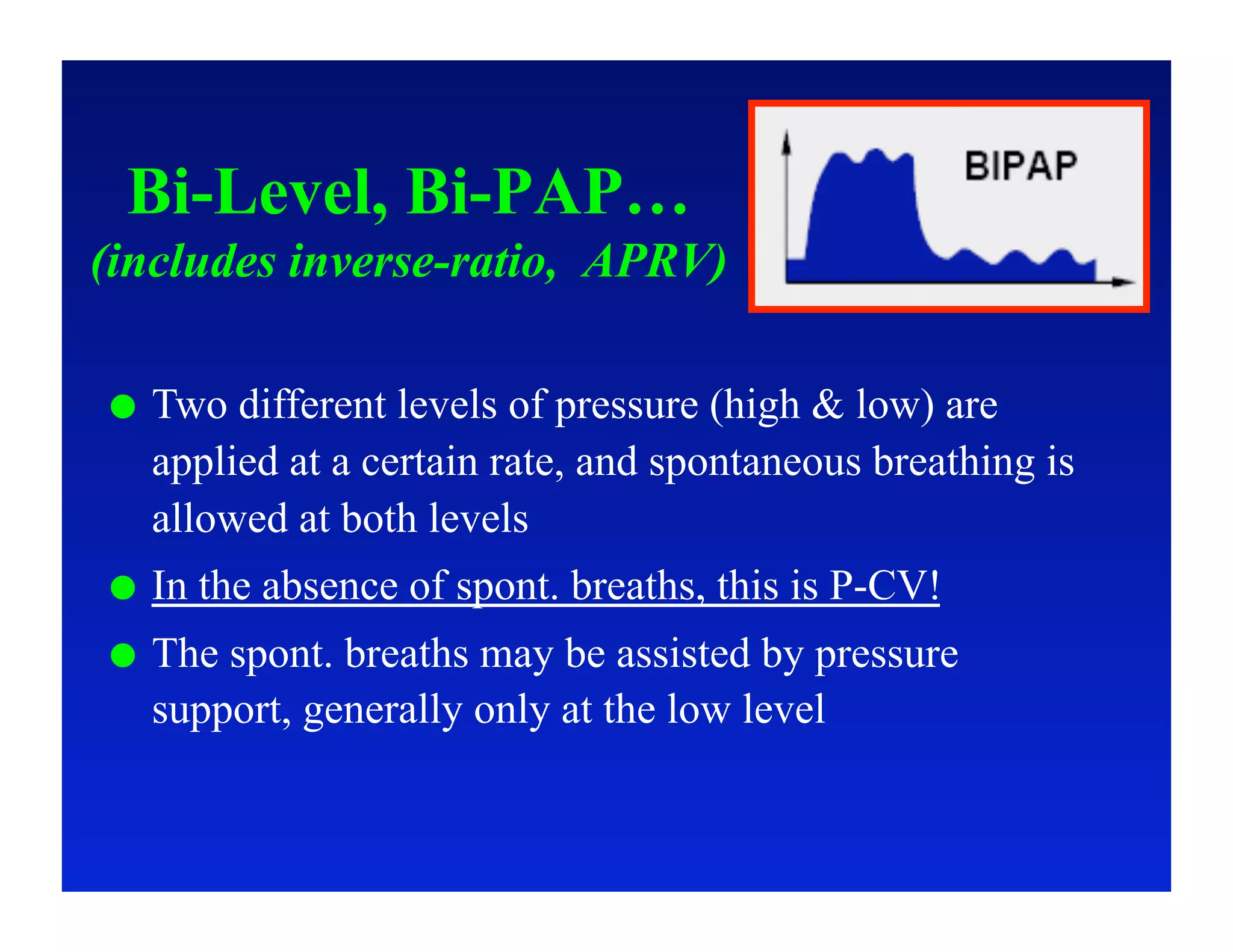
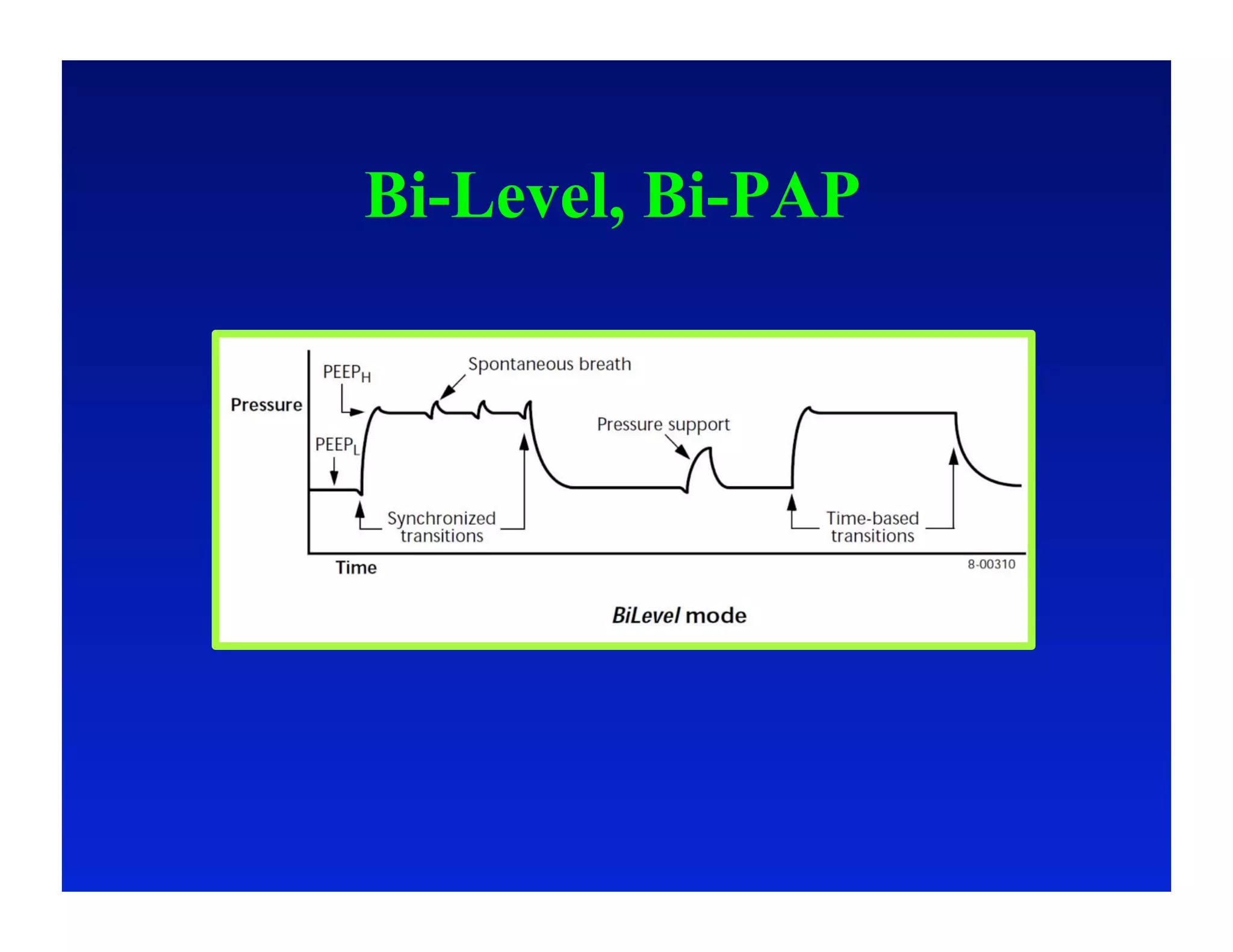
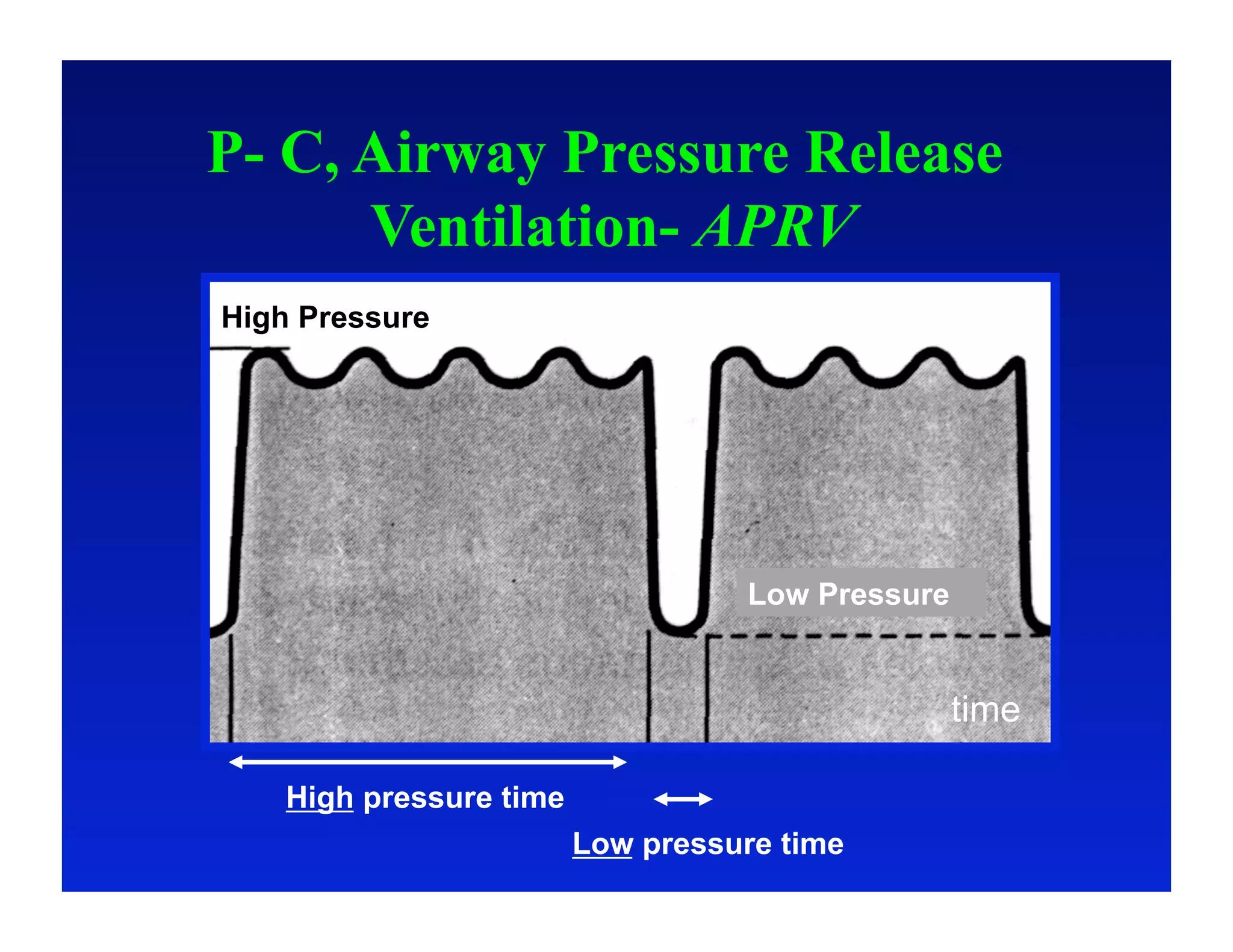
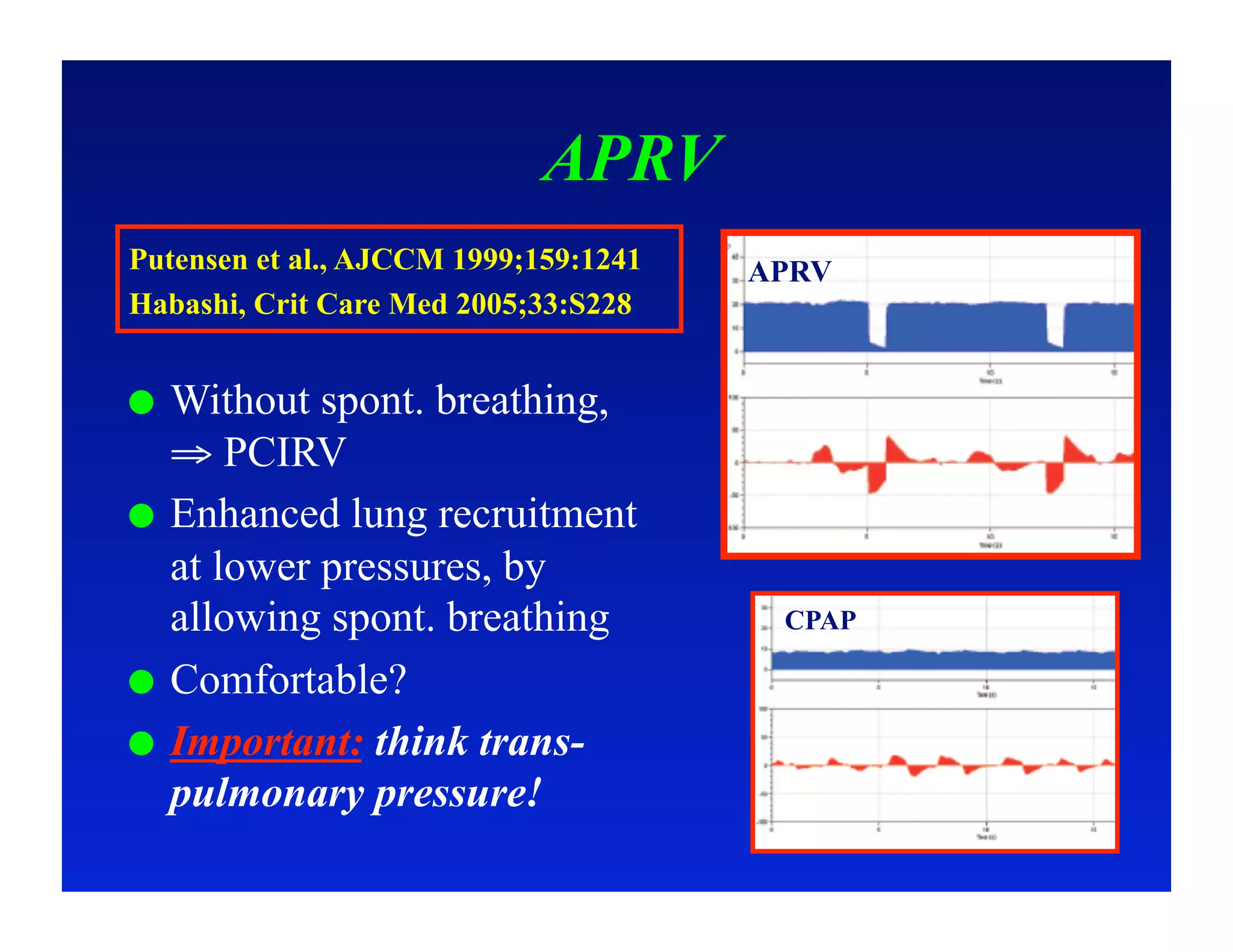
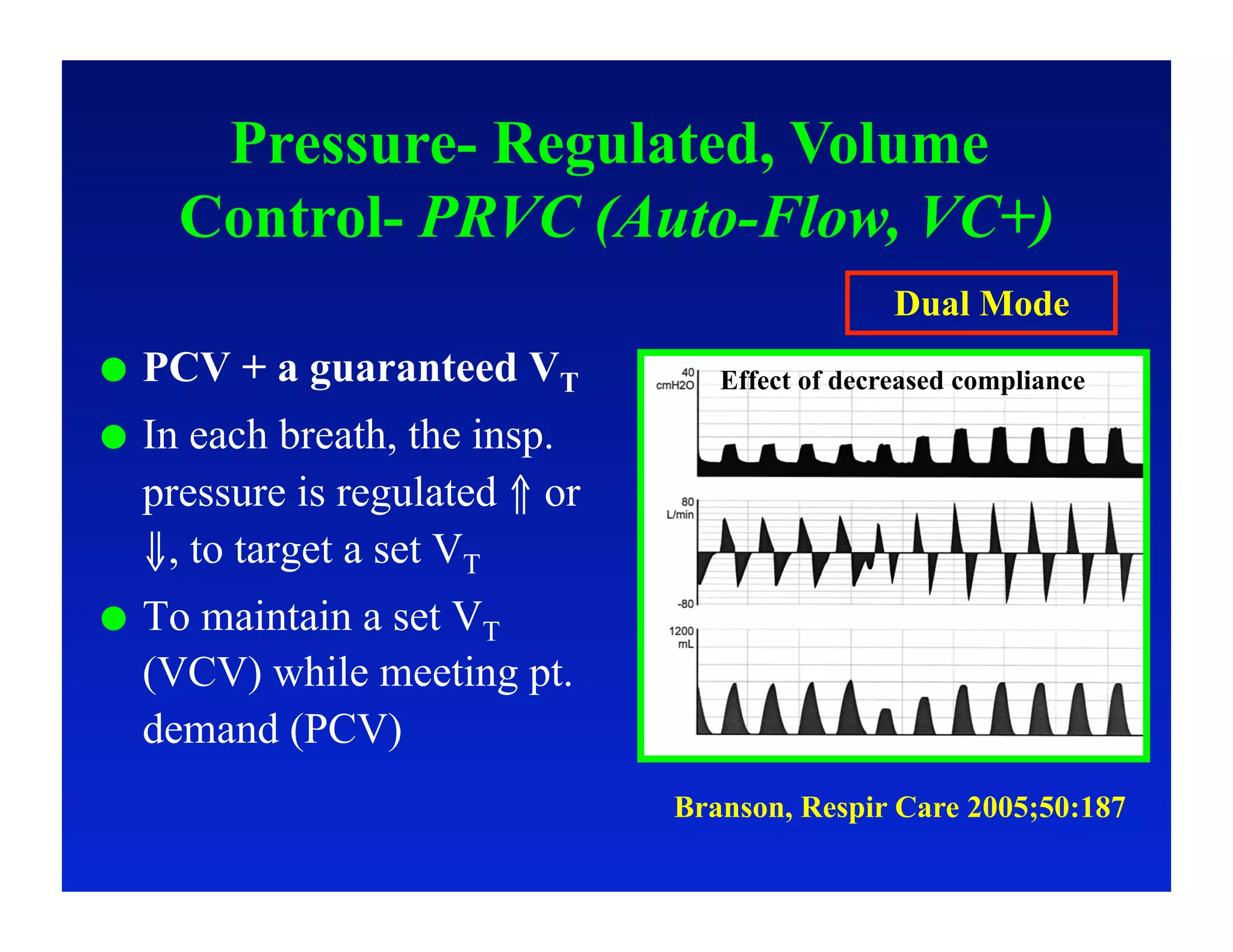
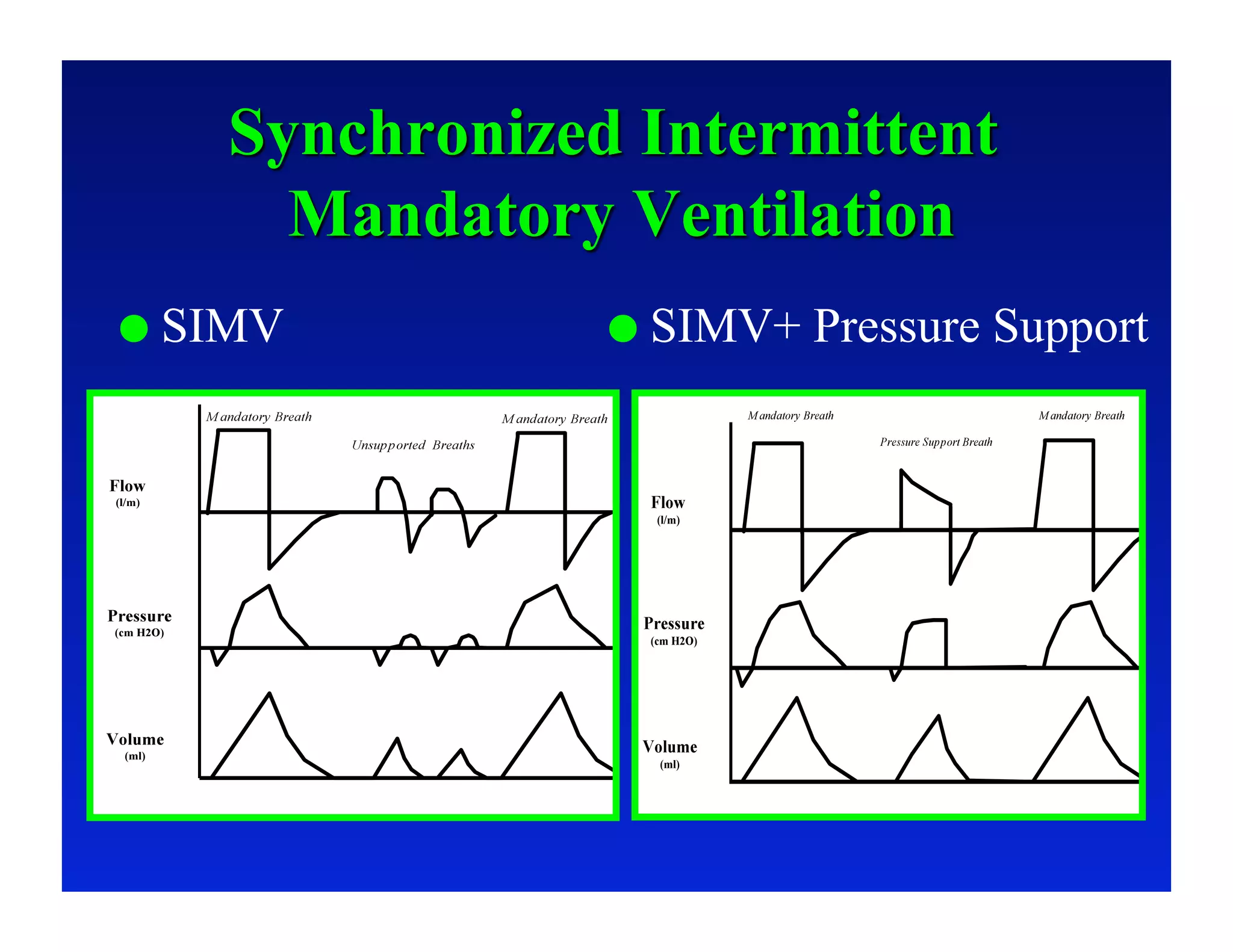
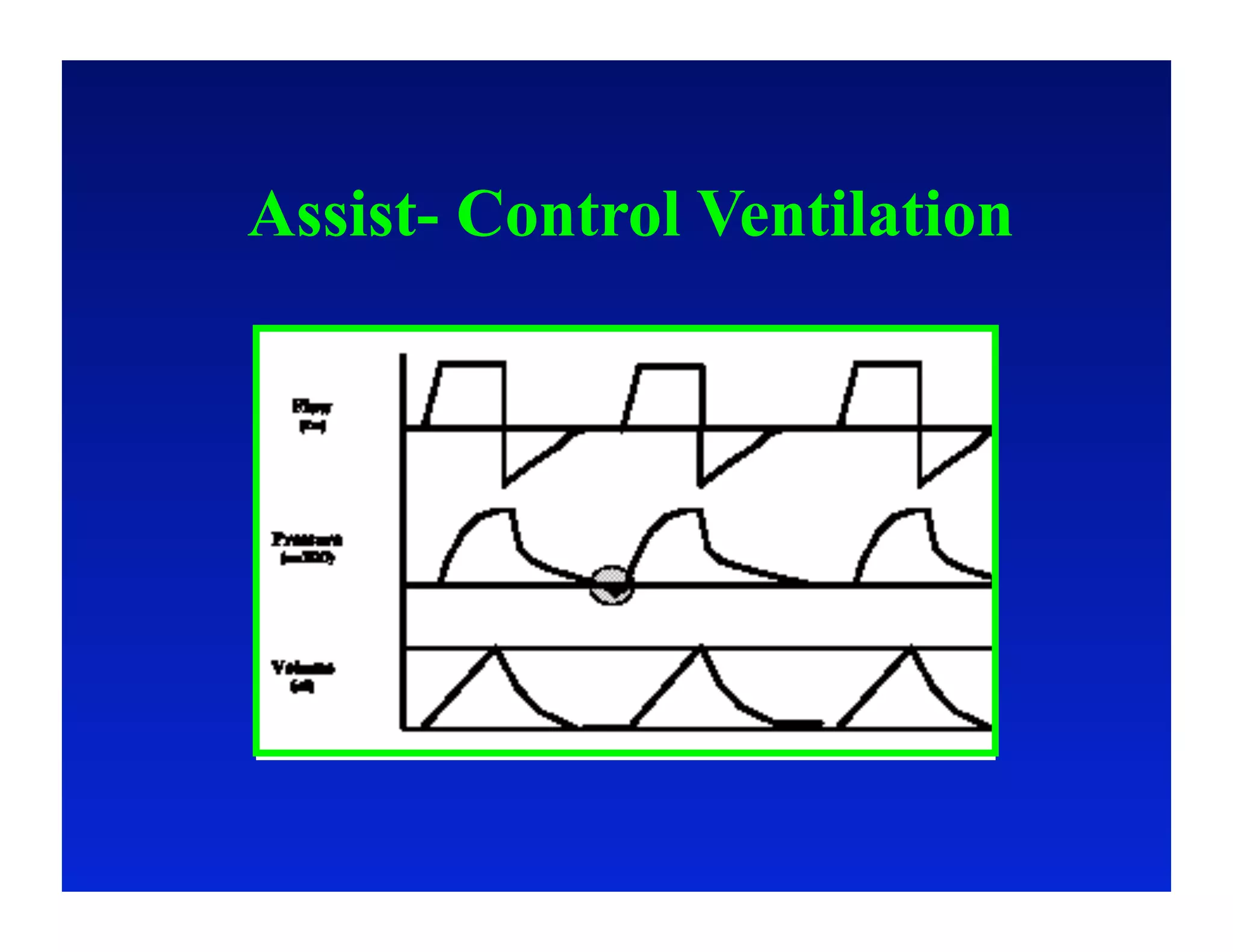
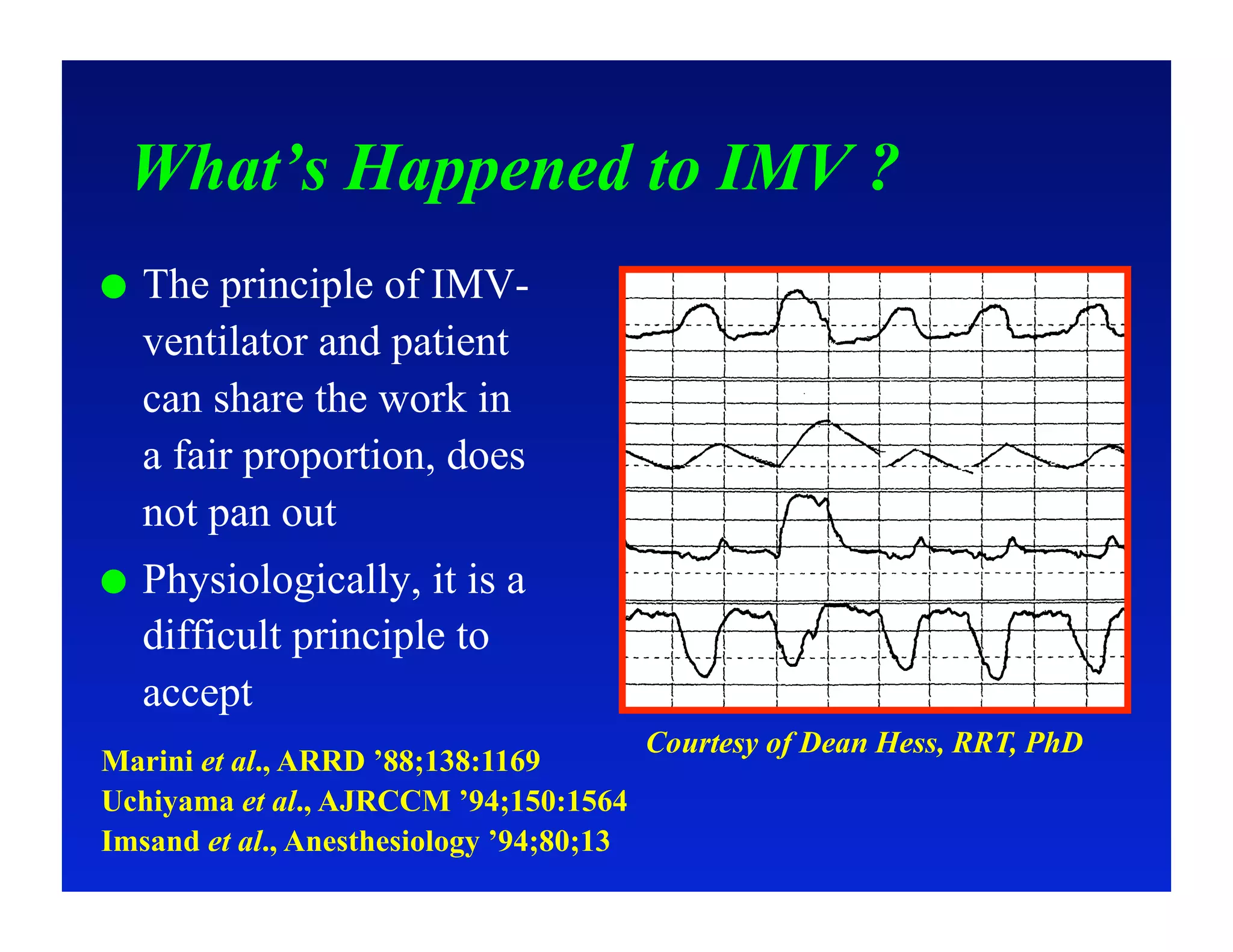
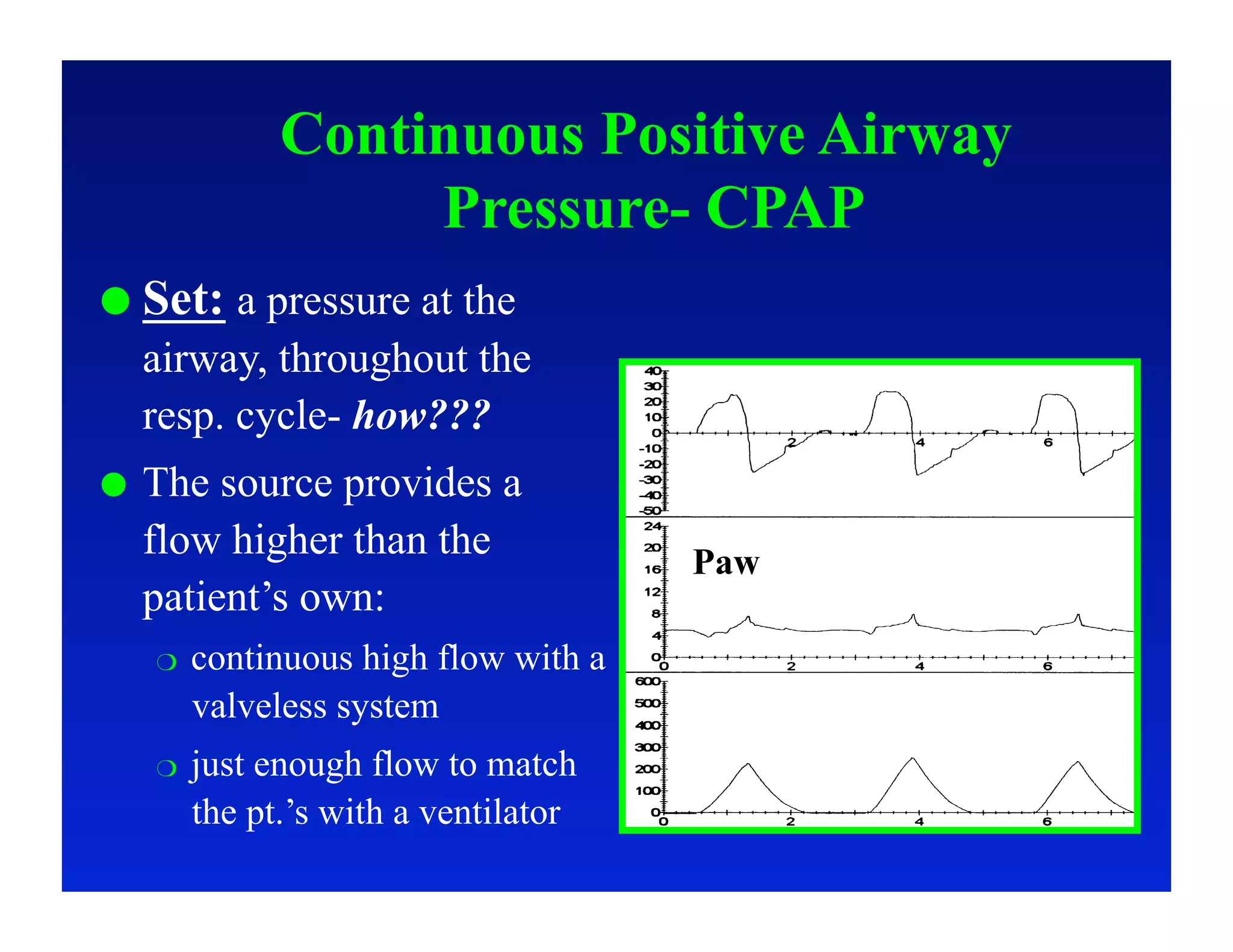
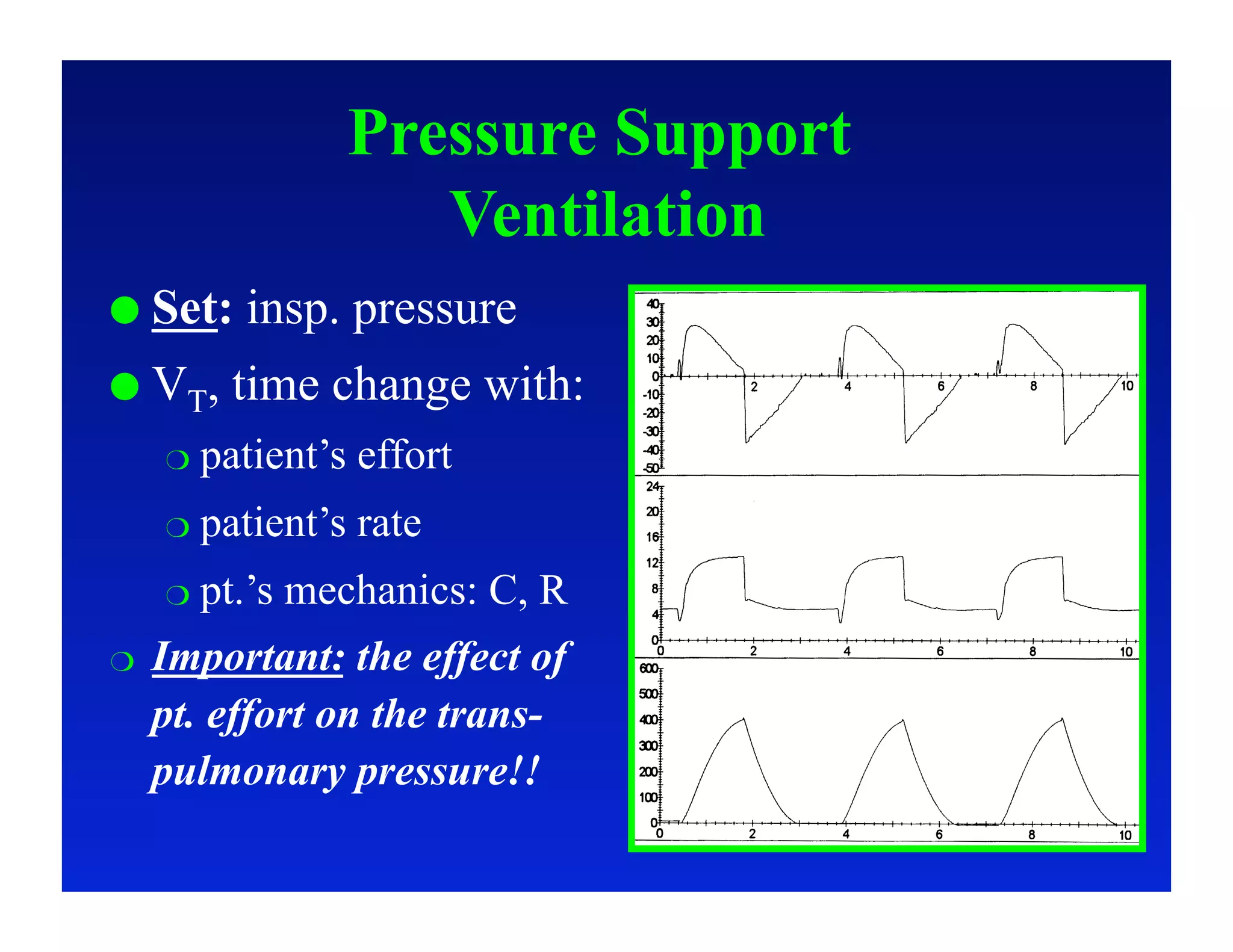
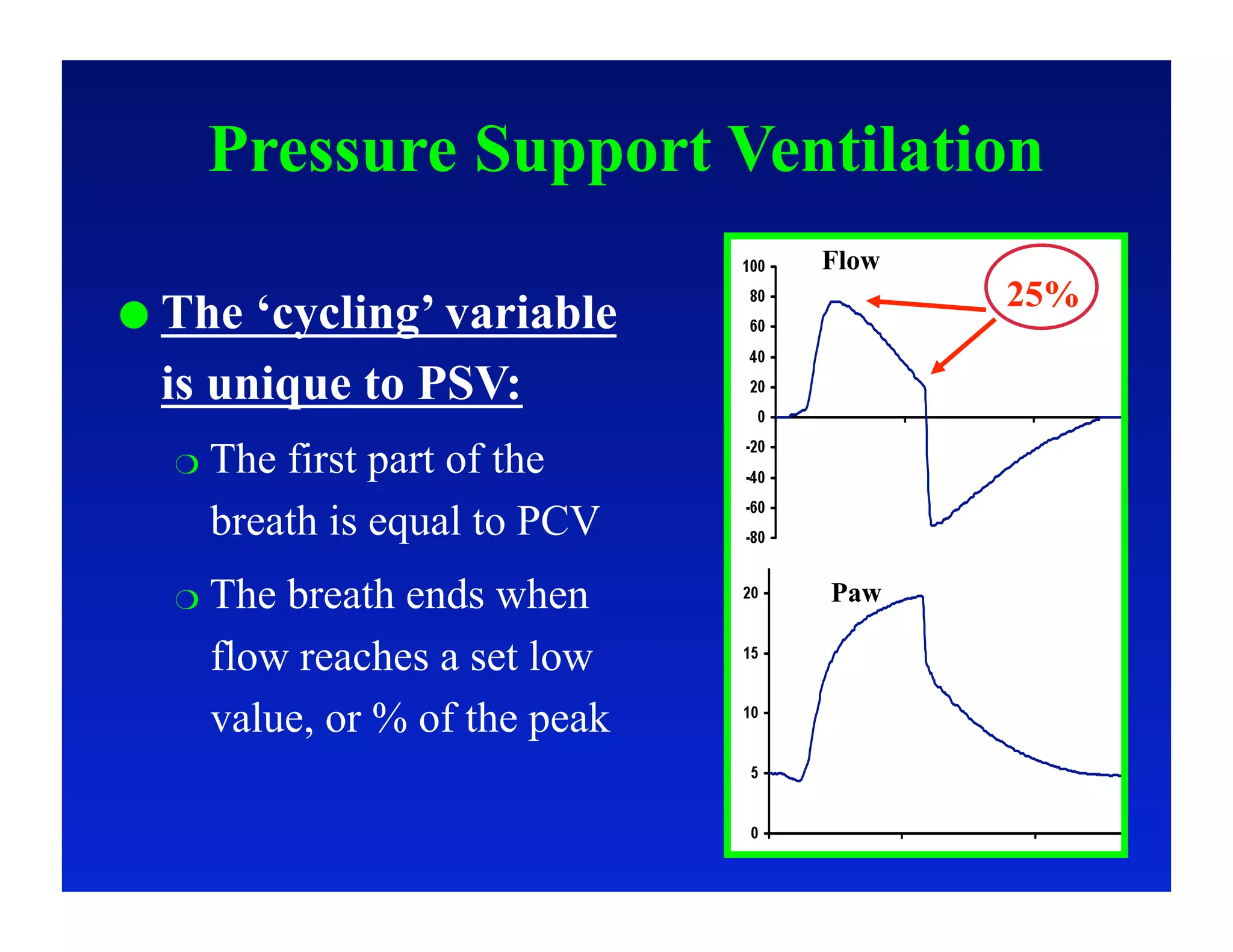
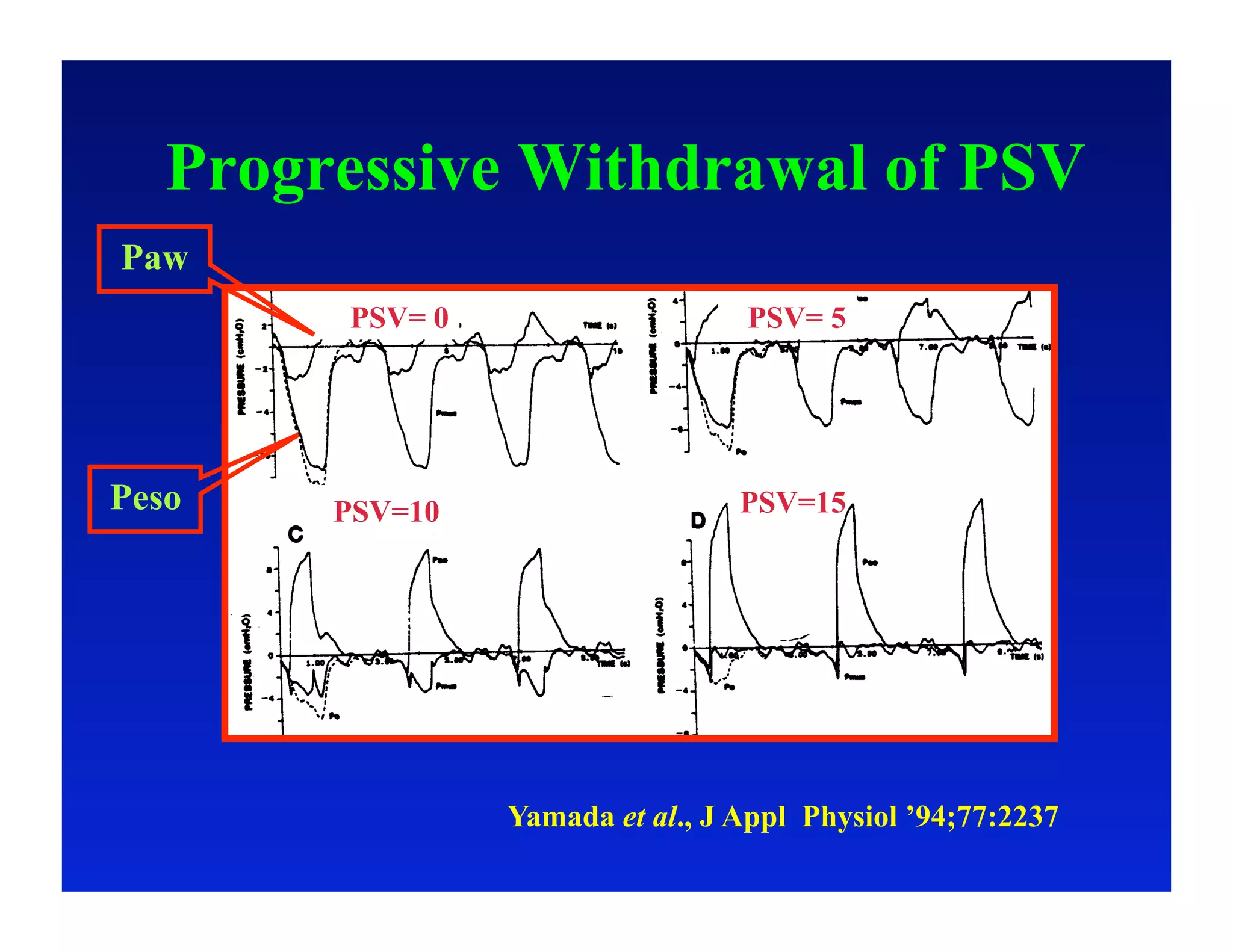
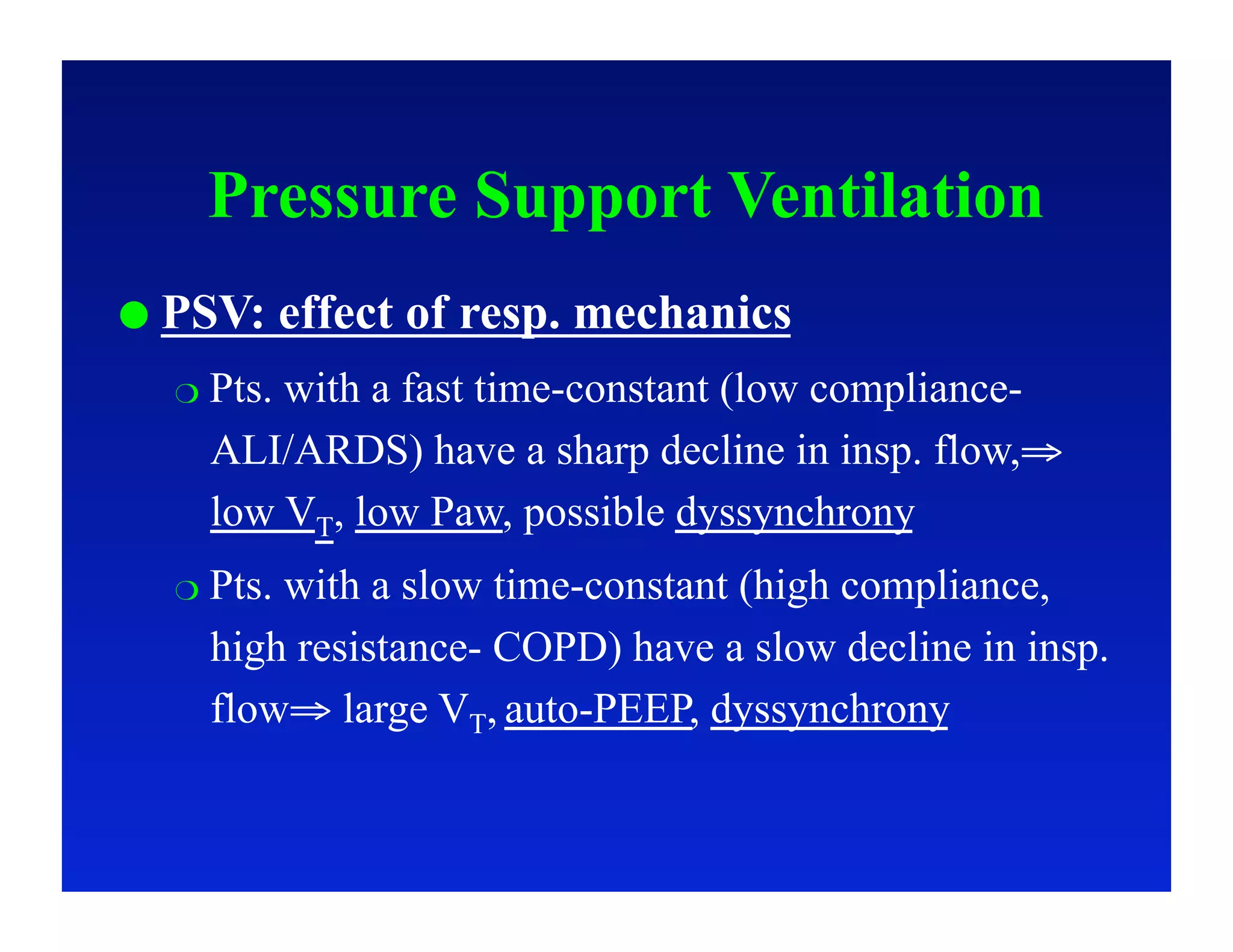
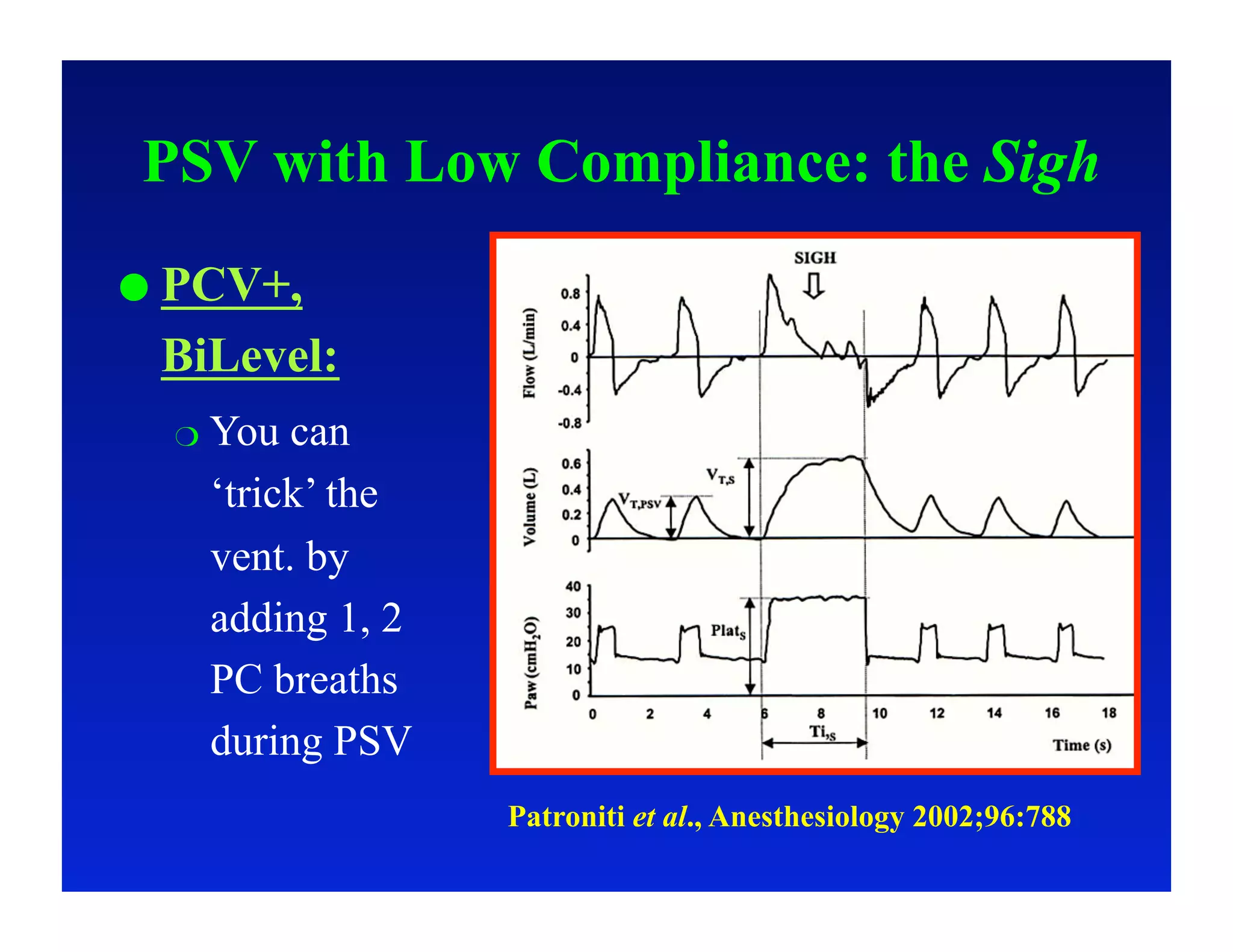
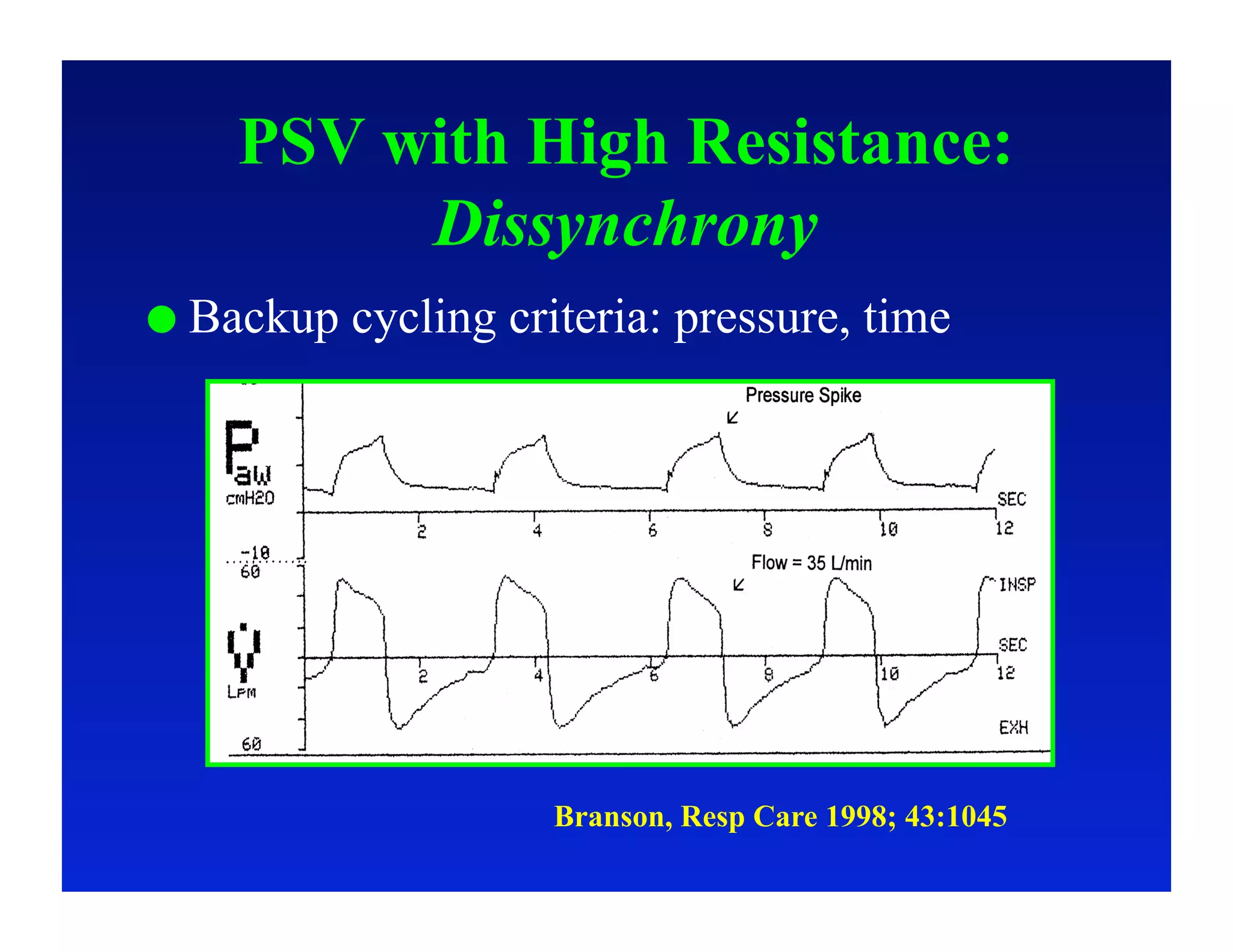
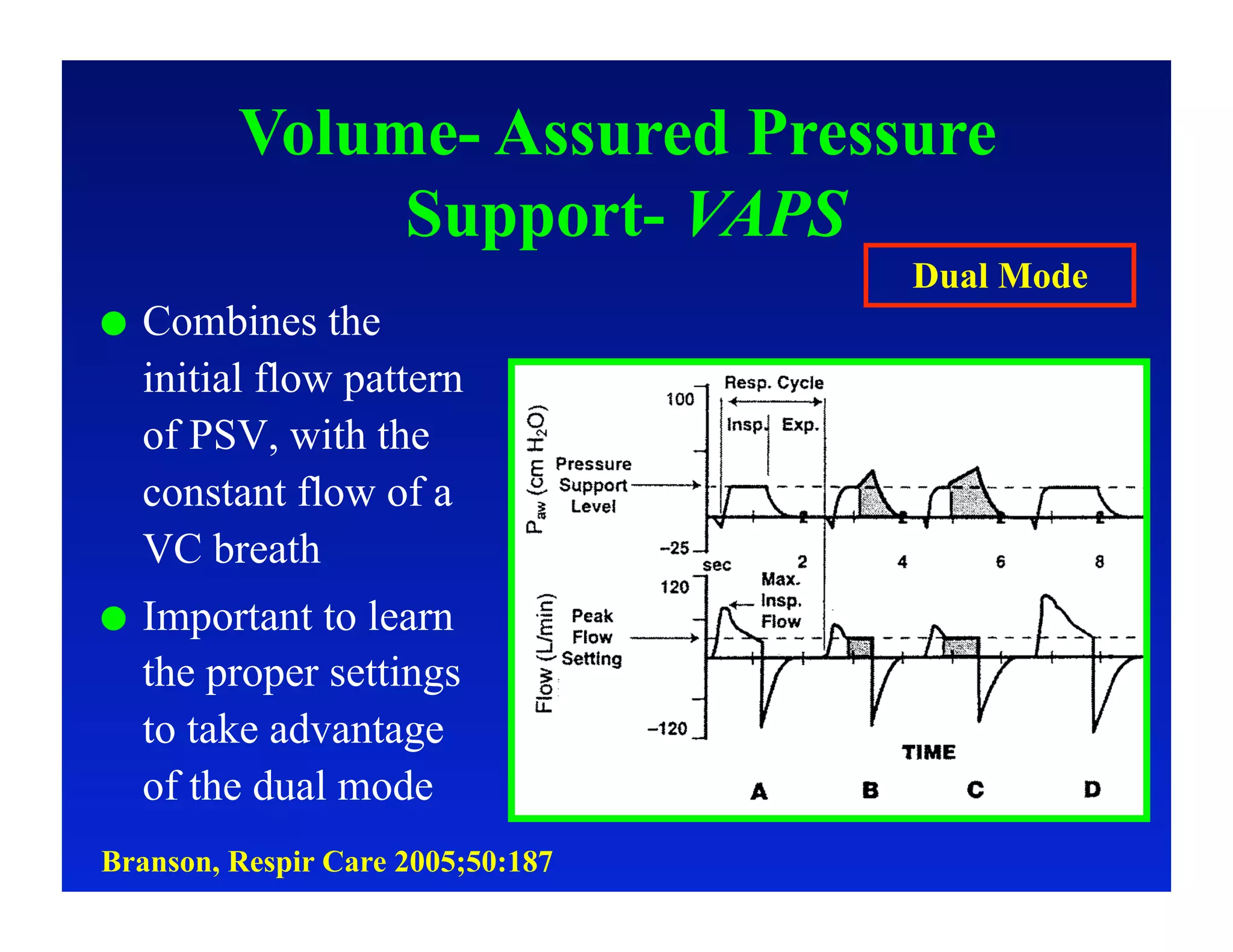
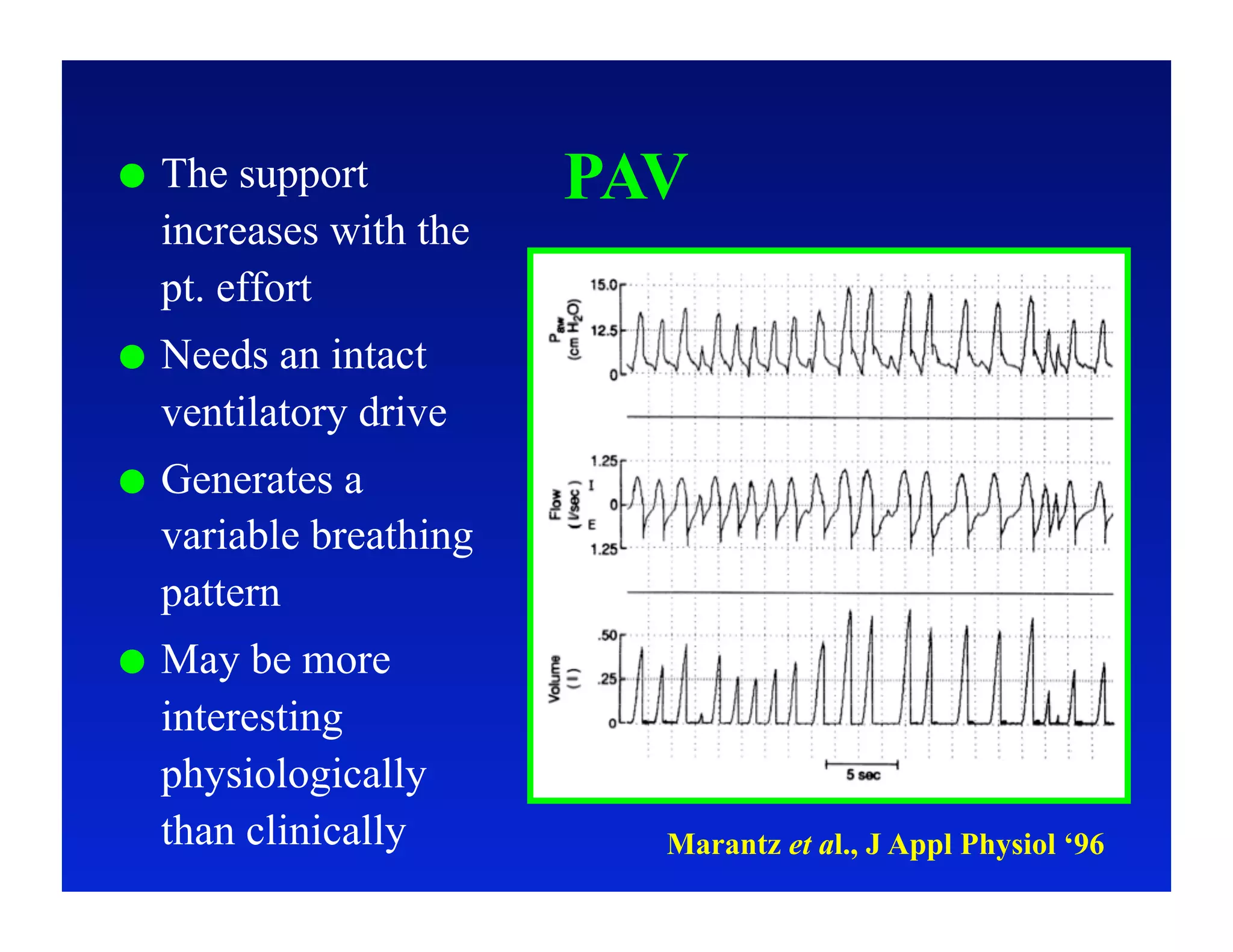
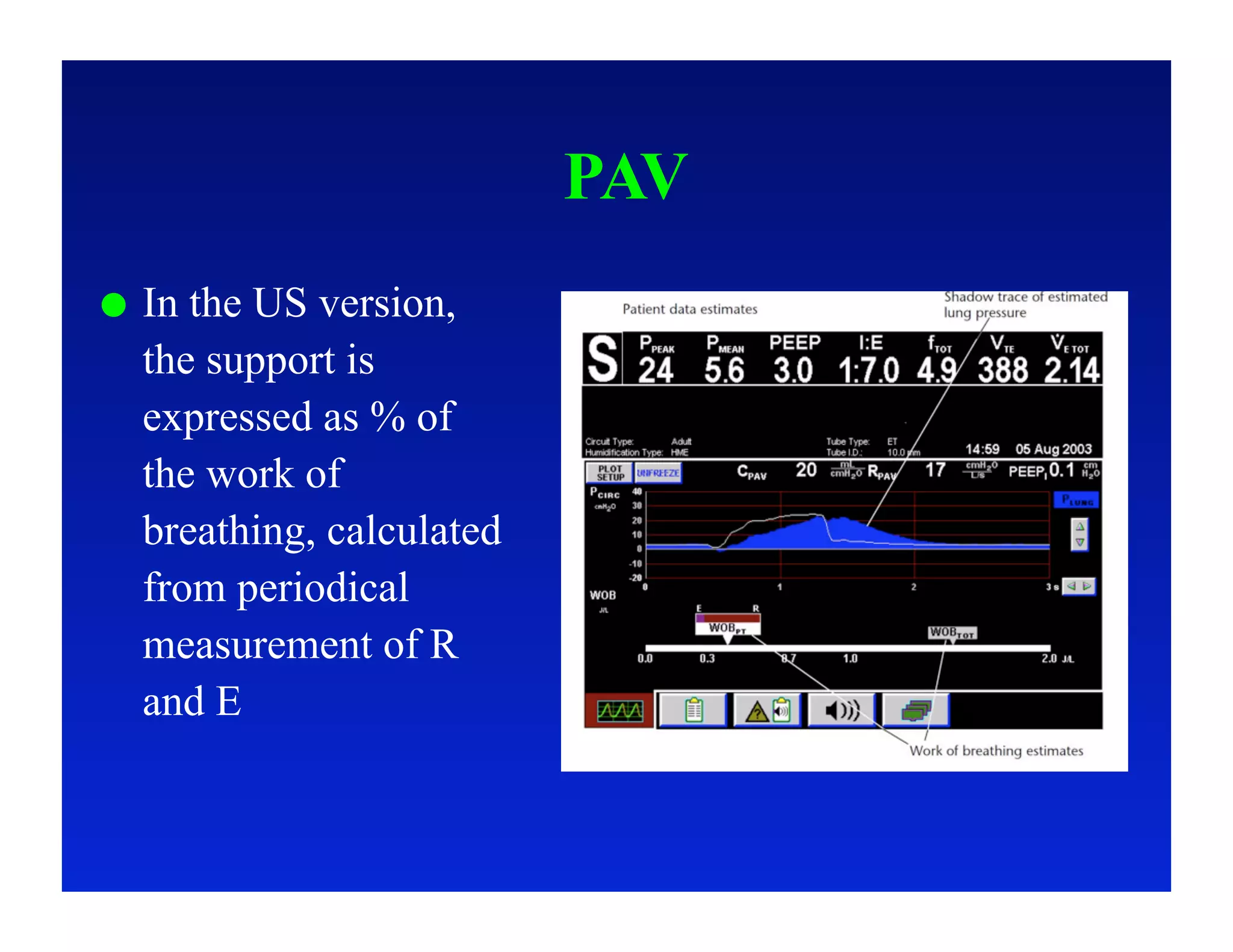
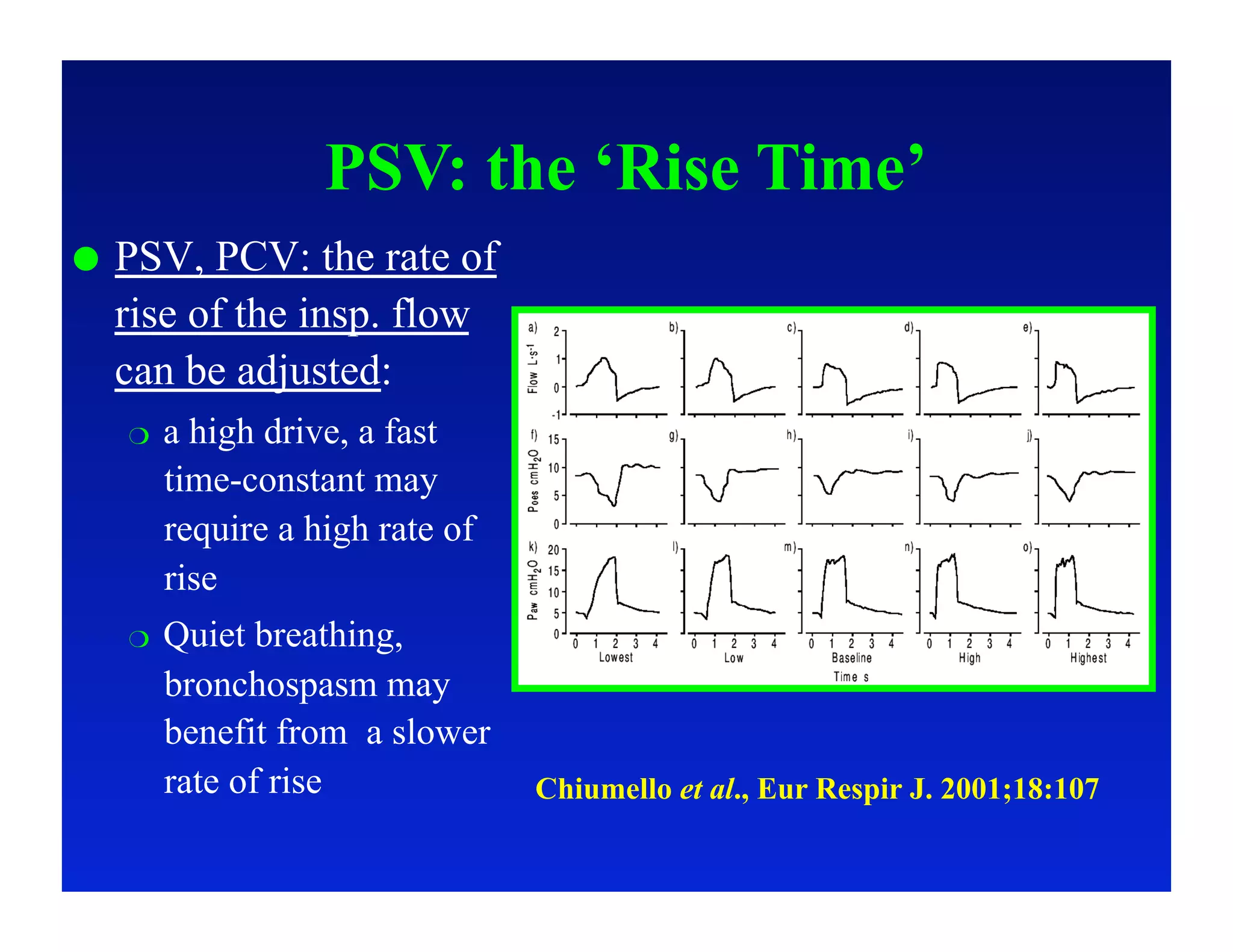
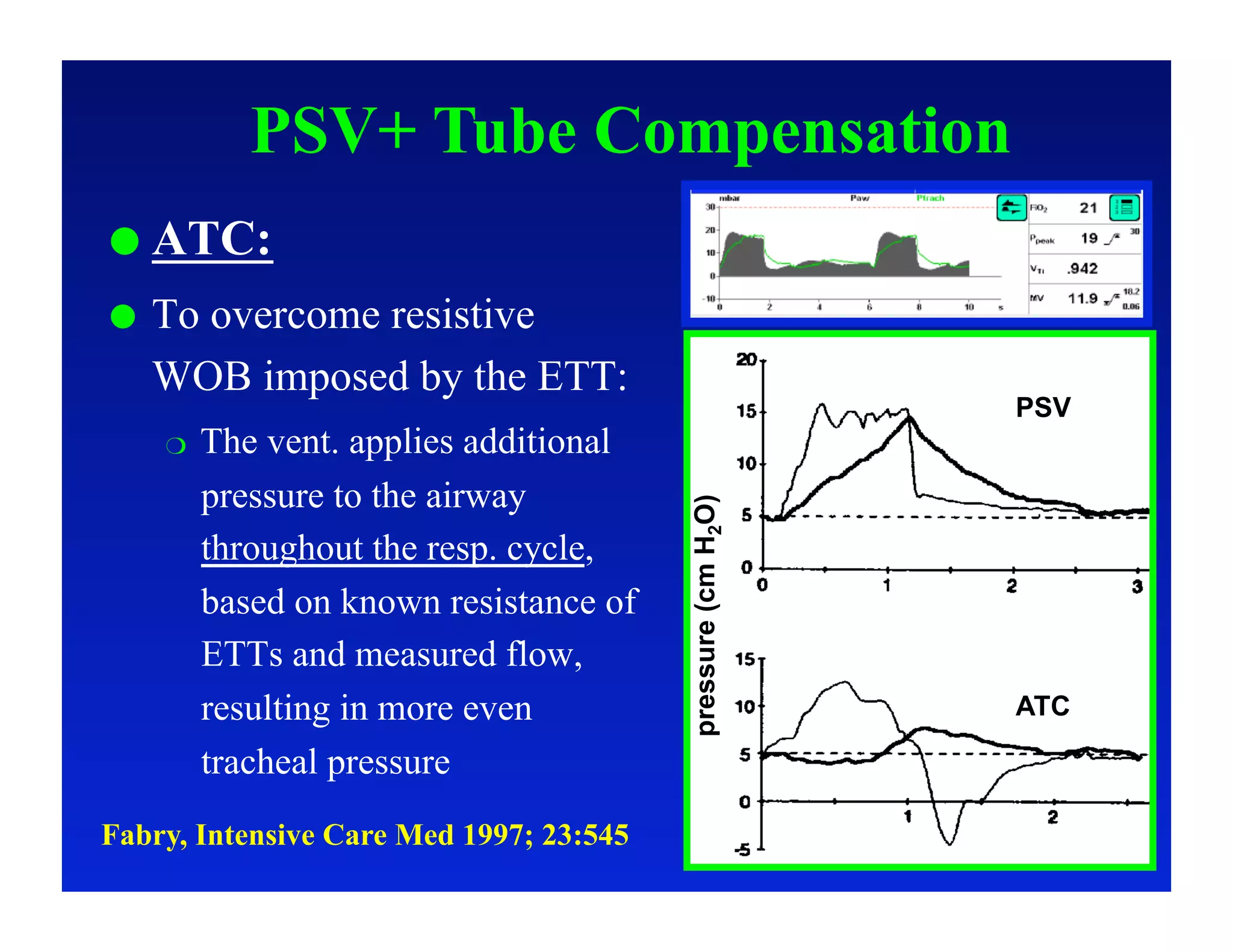
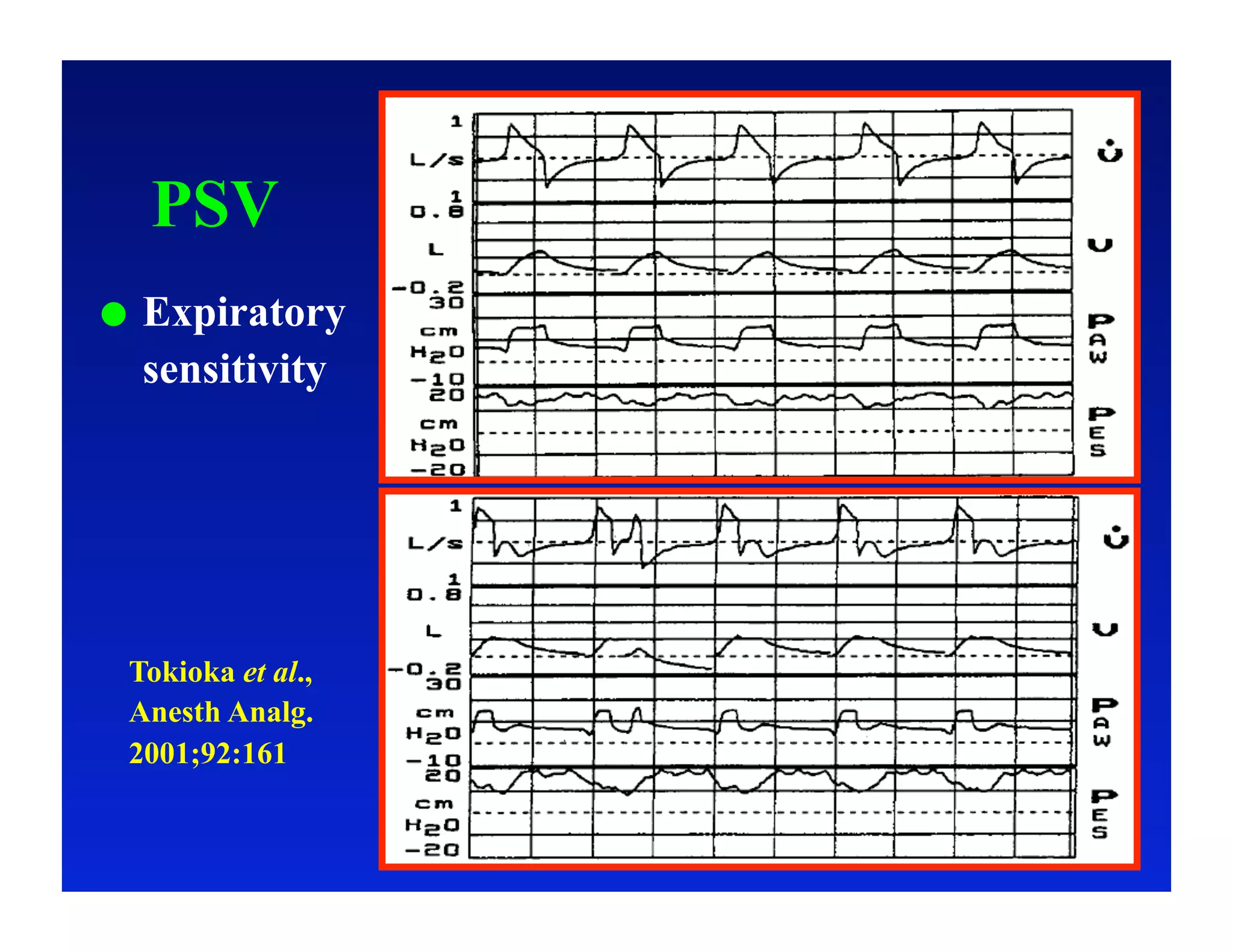
2. Different modes of mechanical ventilation including volume-controlled, pressure-controlled, bi-level, and pressure support ventilation.
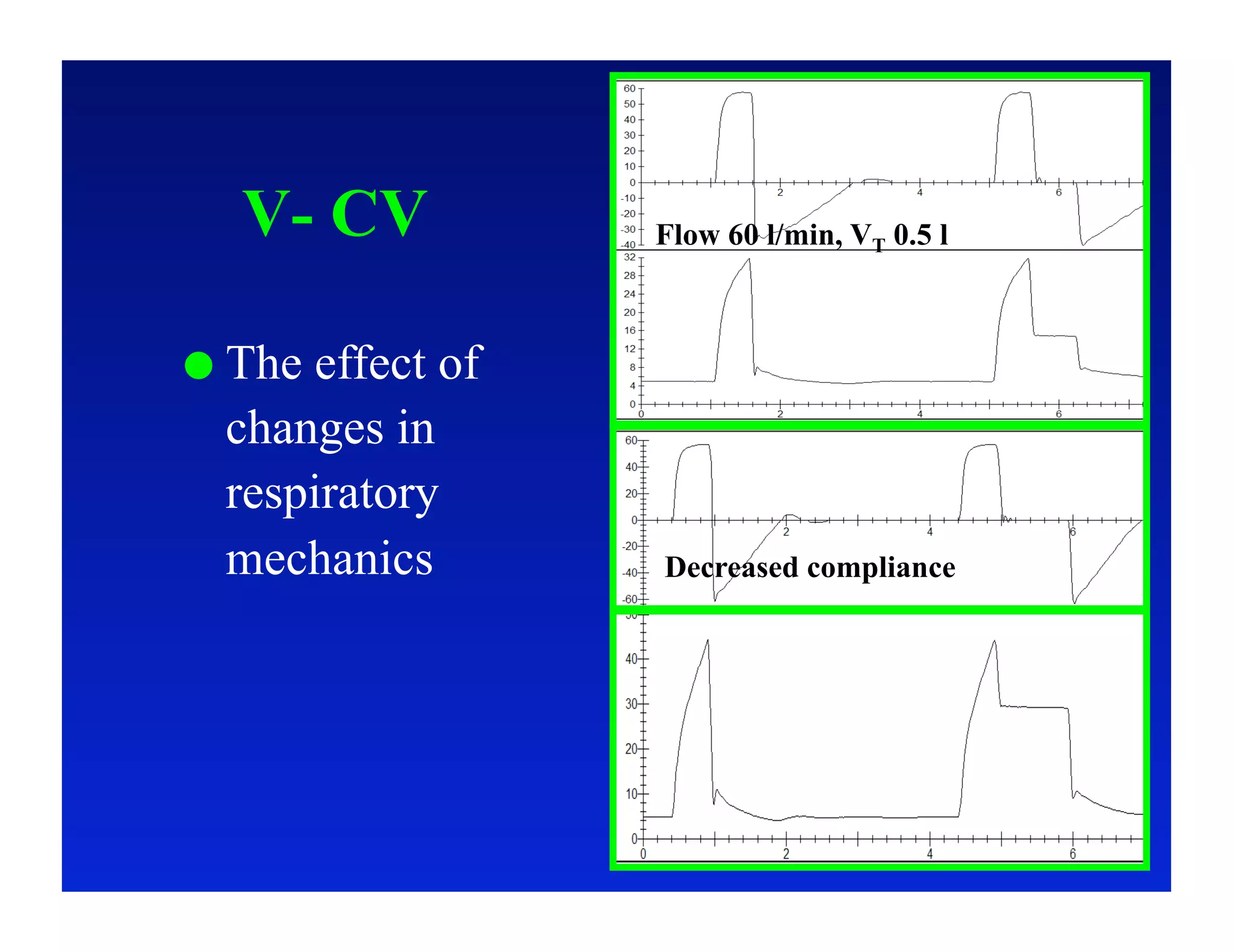
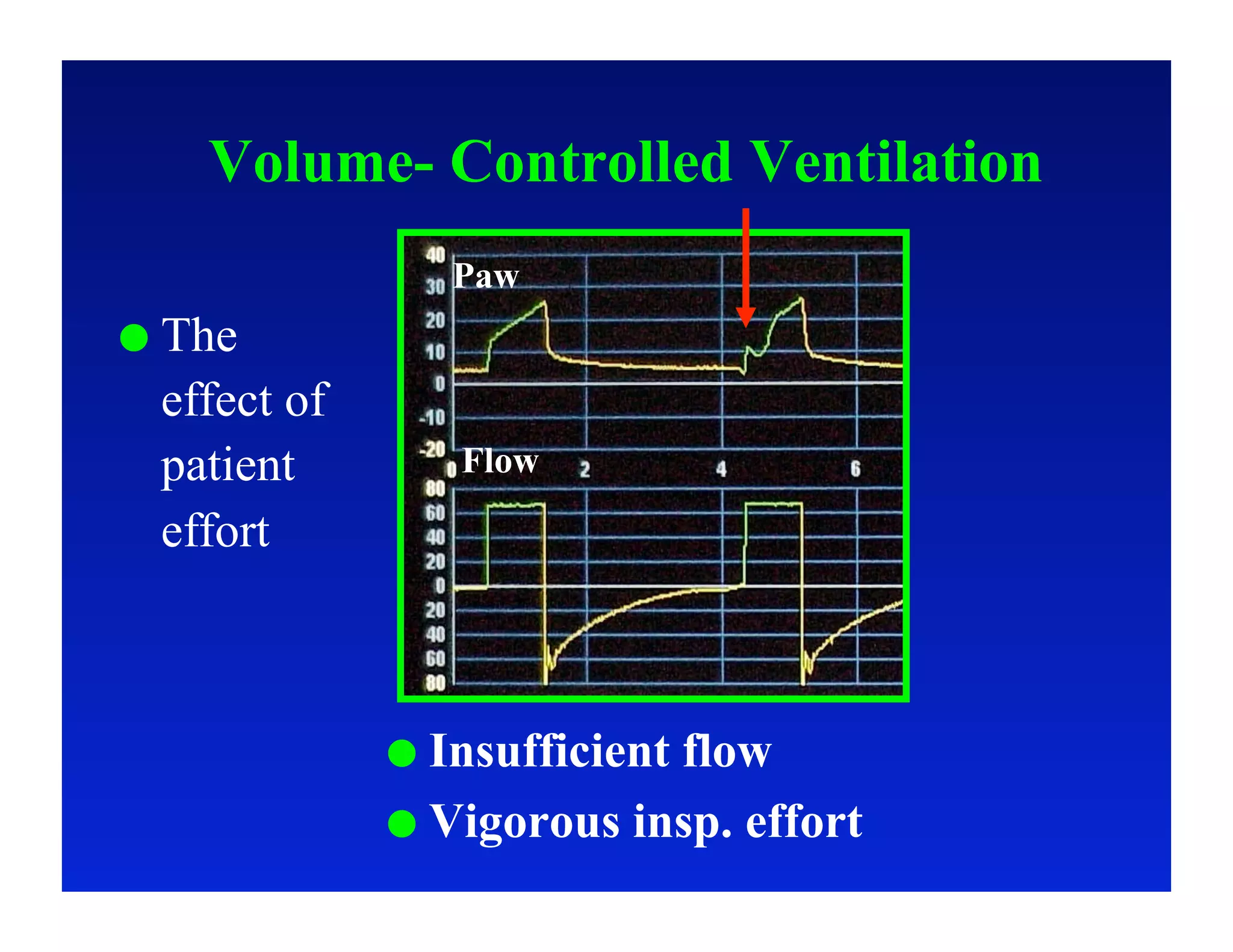
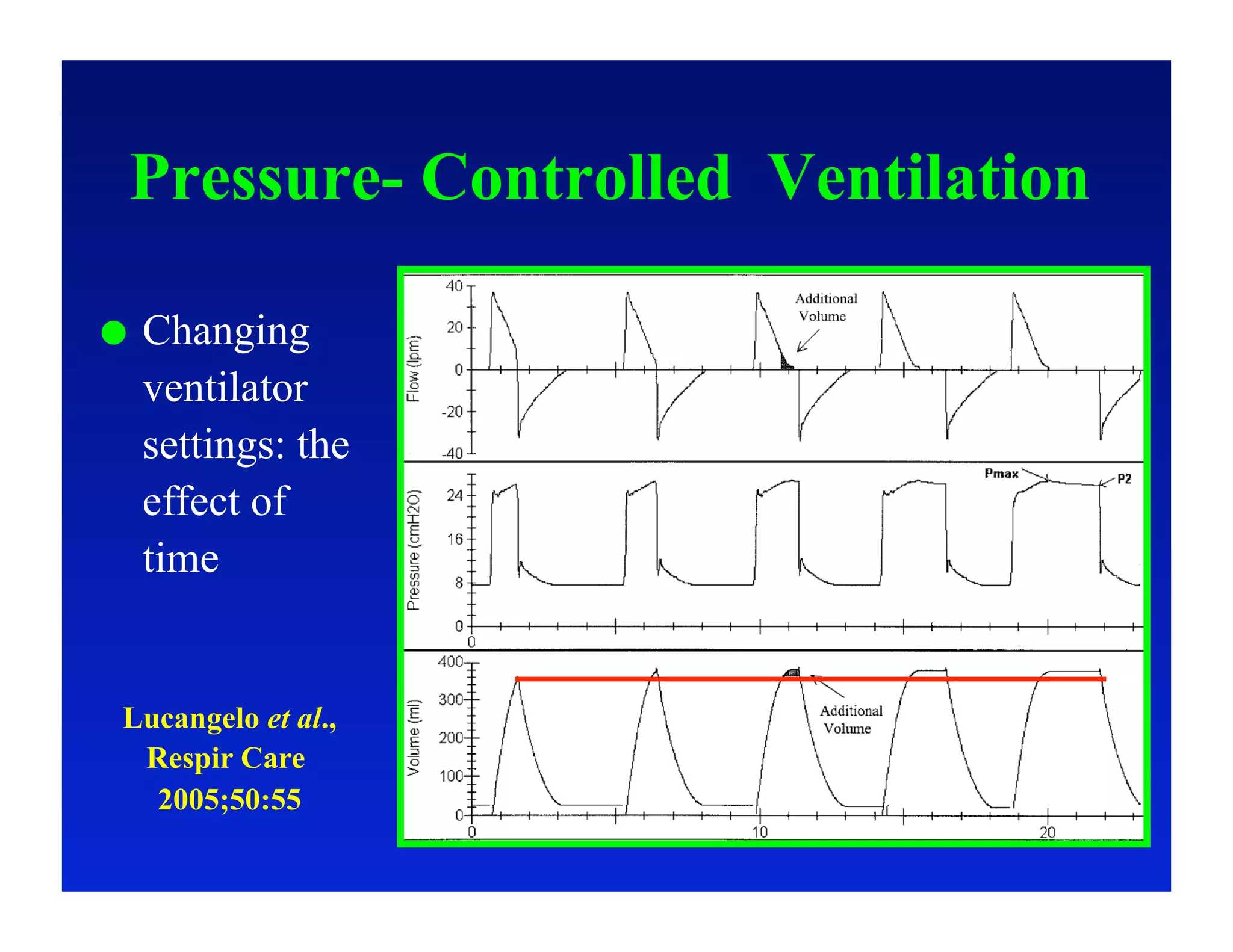
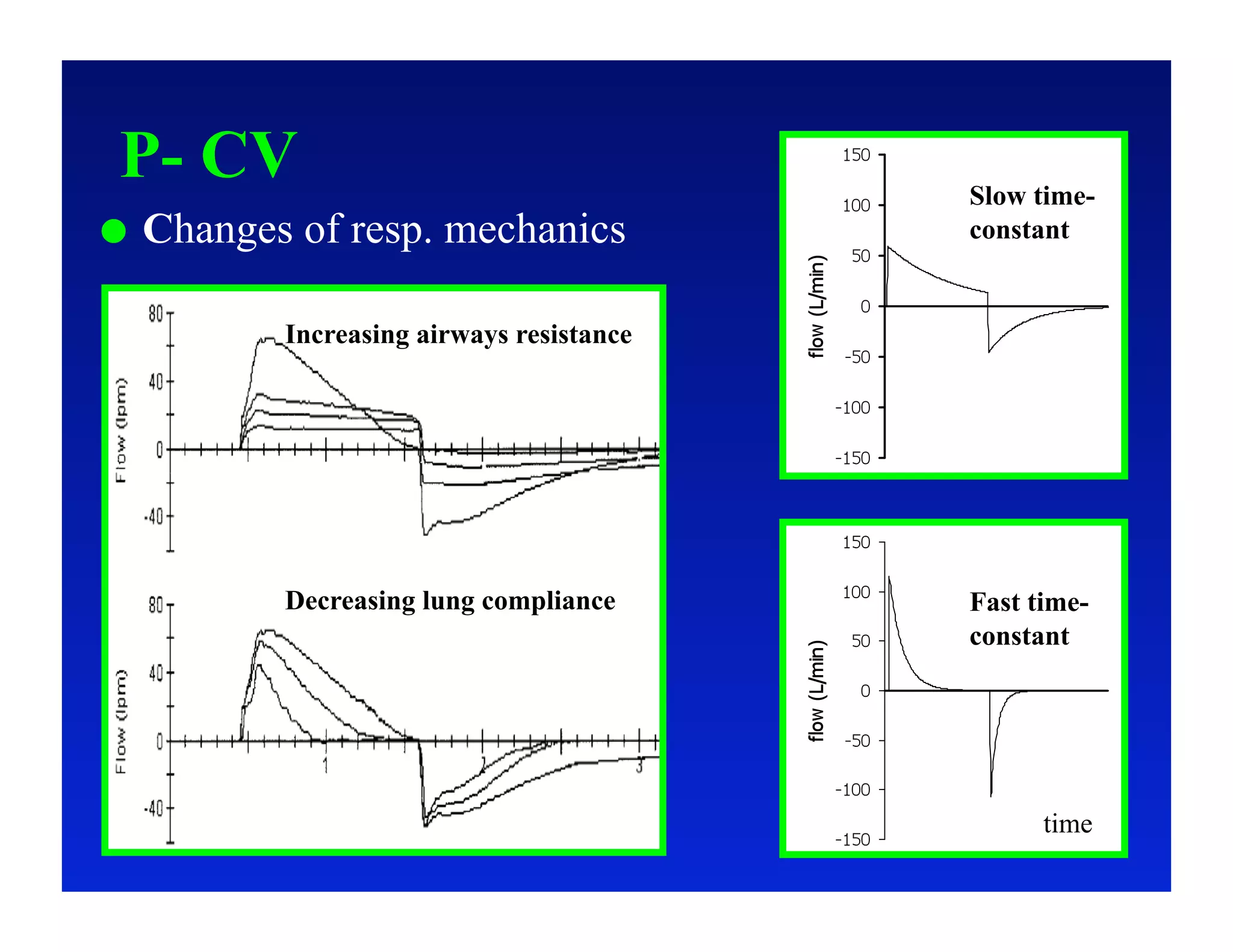
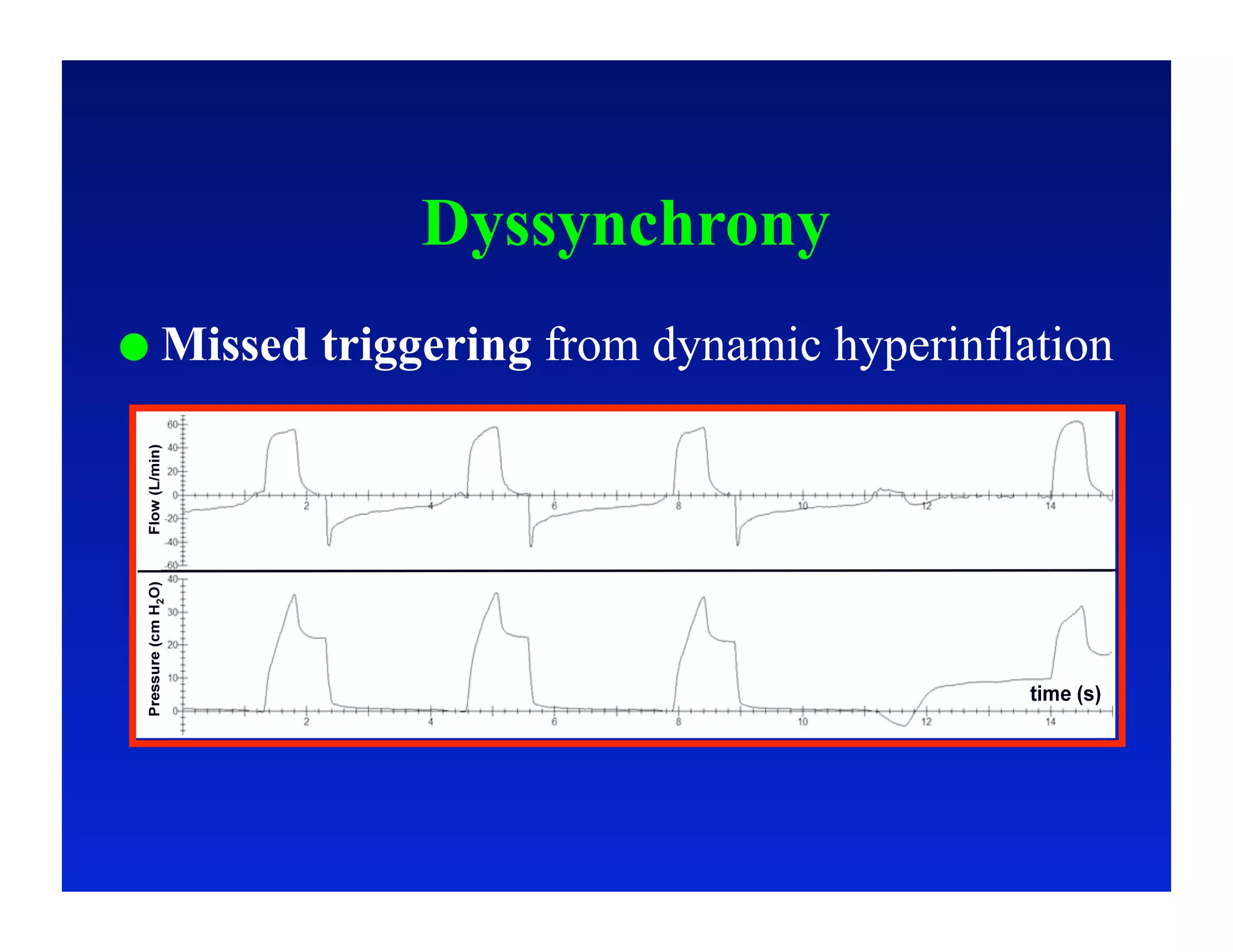
3. How changes in ventilator settings and patient physiology affect breath delivery and waveforms.
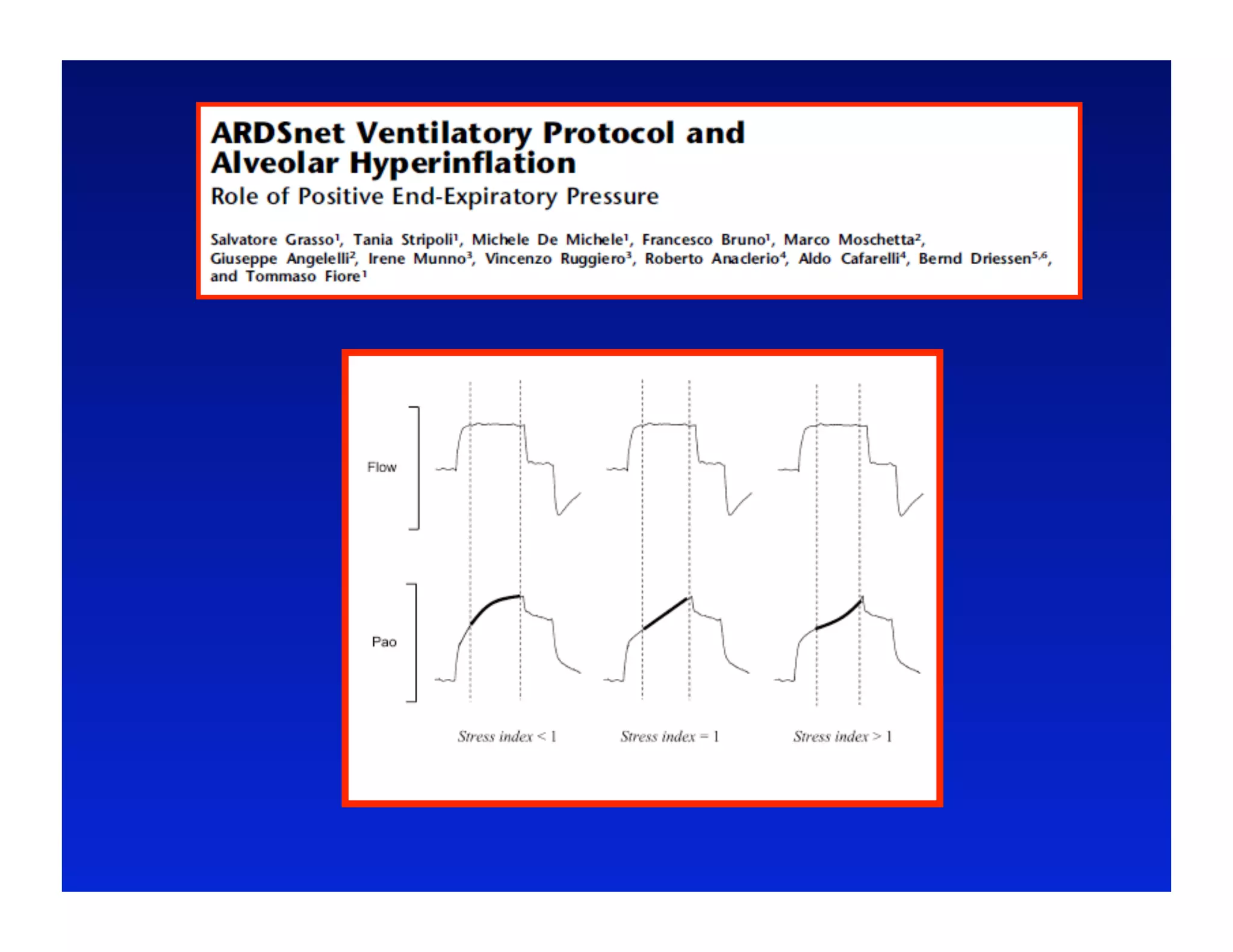
4. Specific situations like ARDS and weaning where understanding waveforms can help guide ventilation.