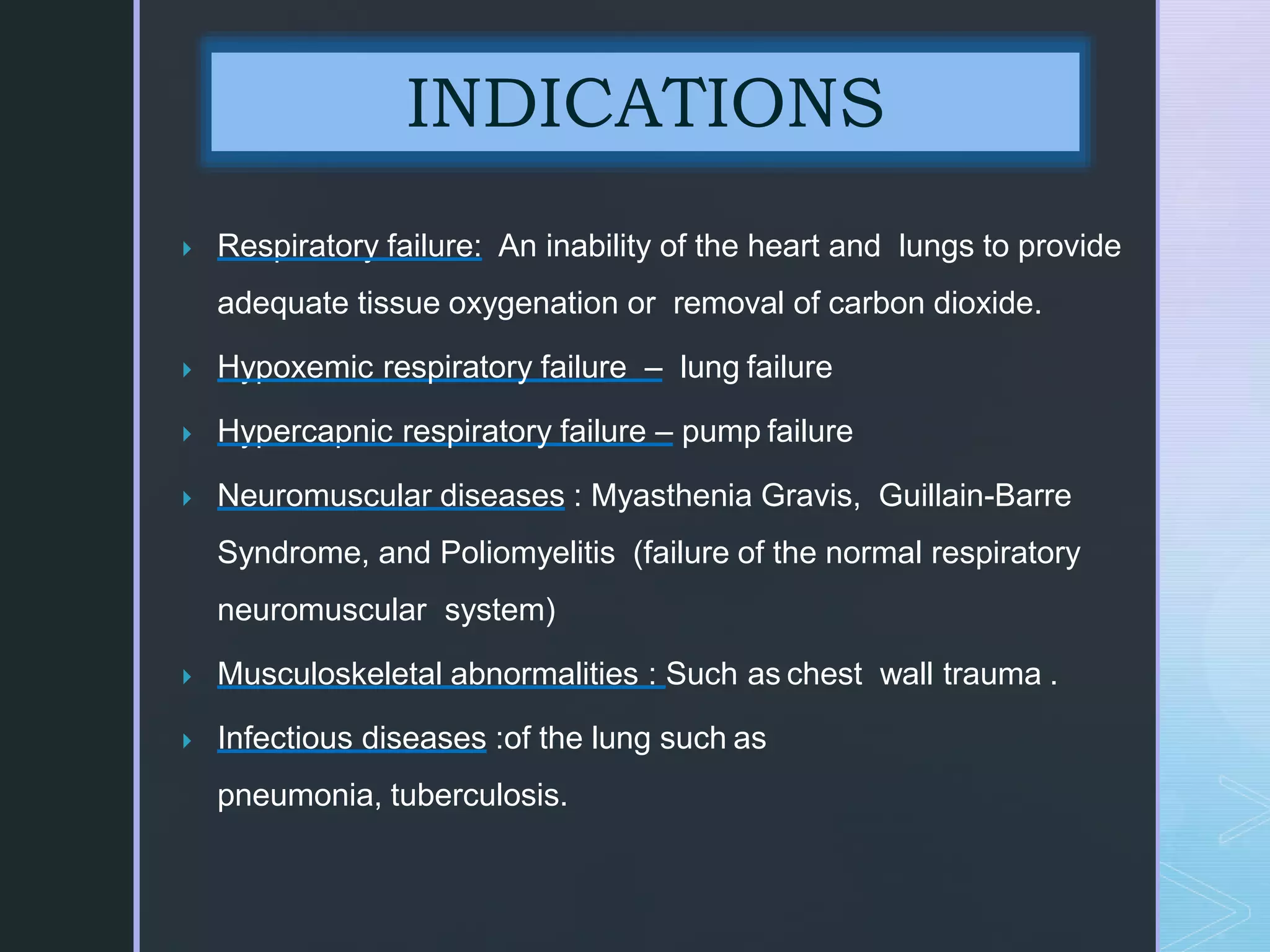
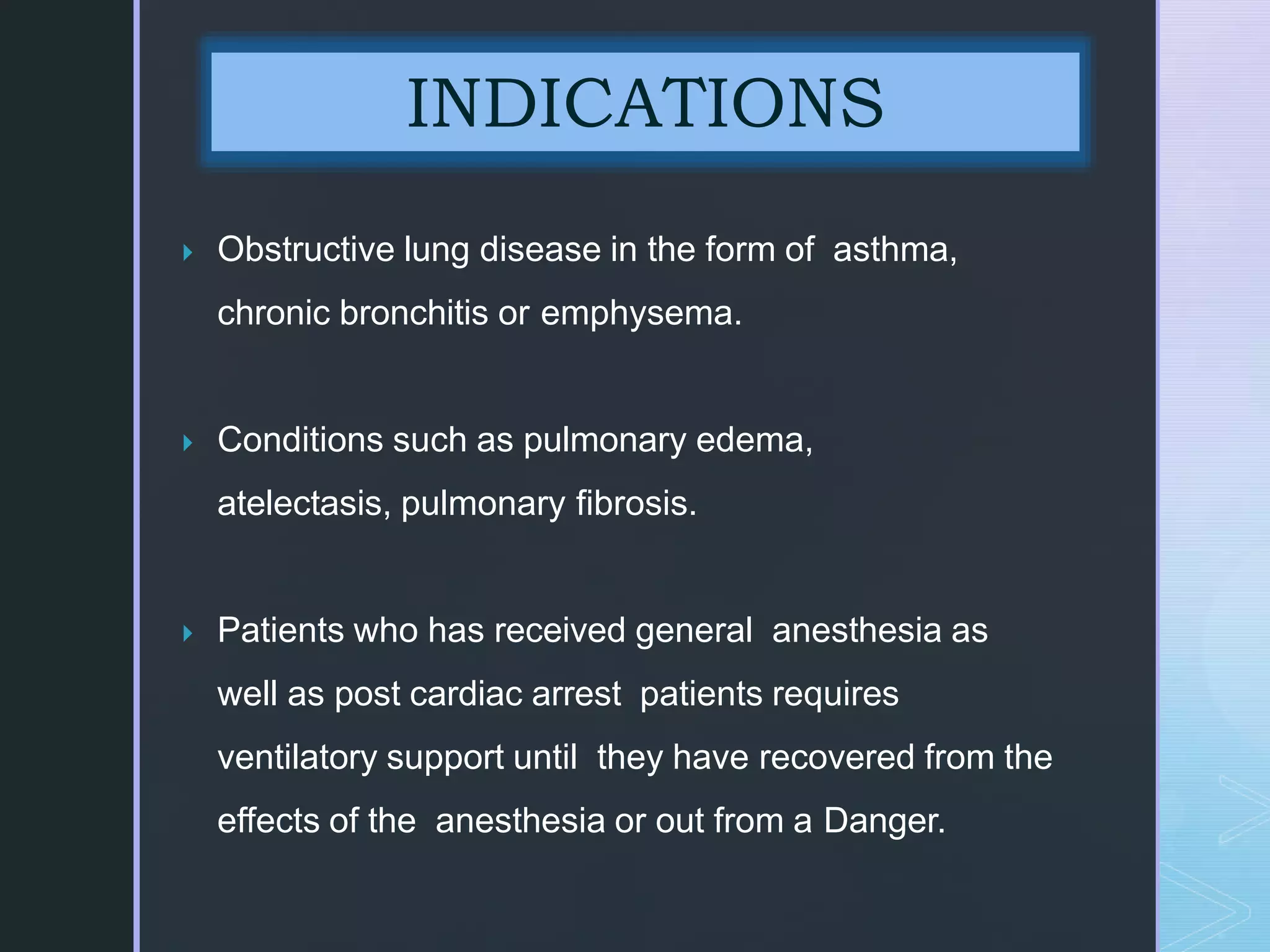
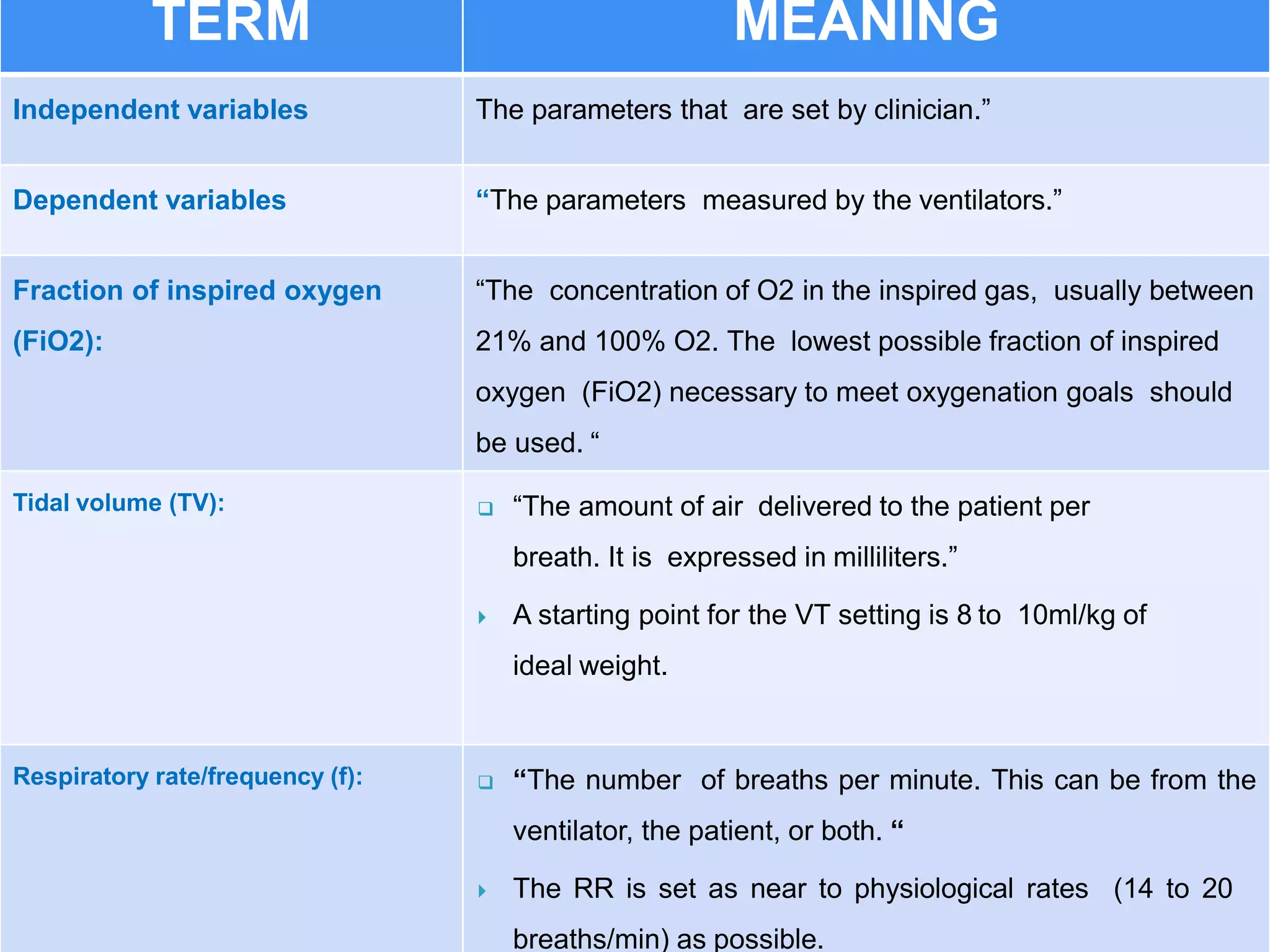
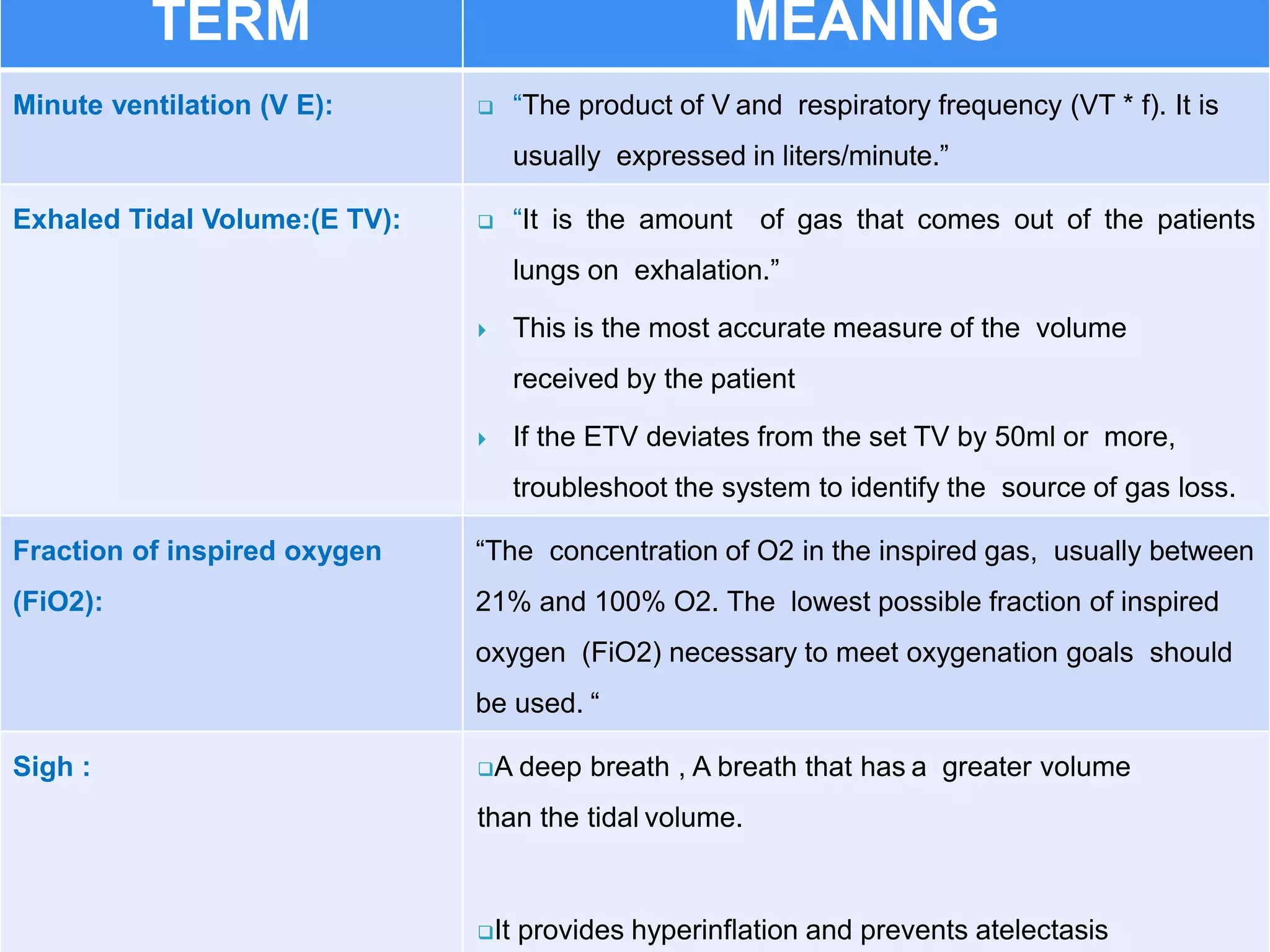
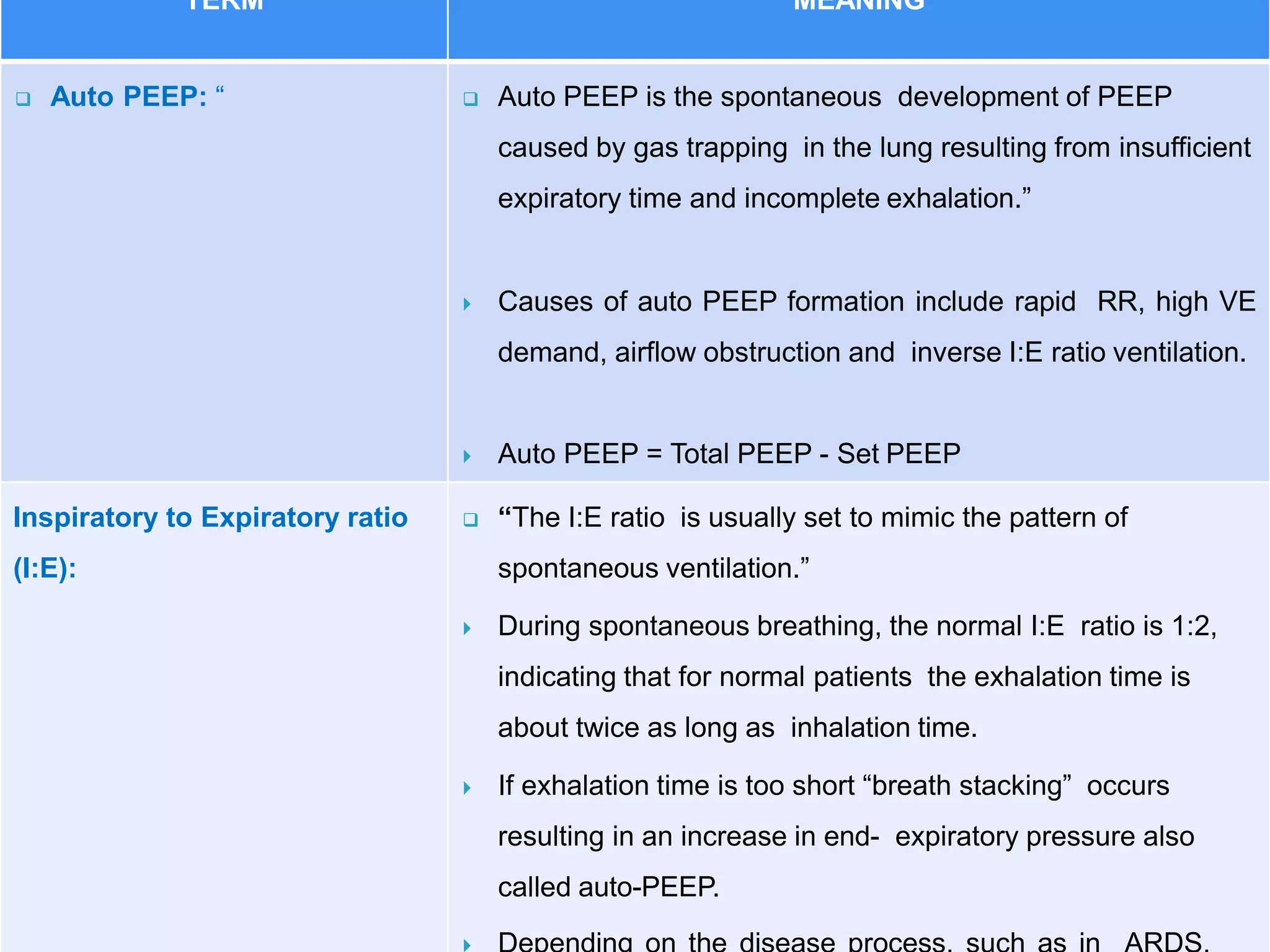
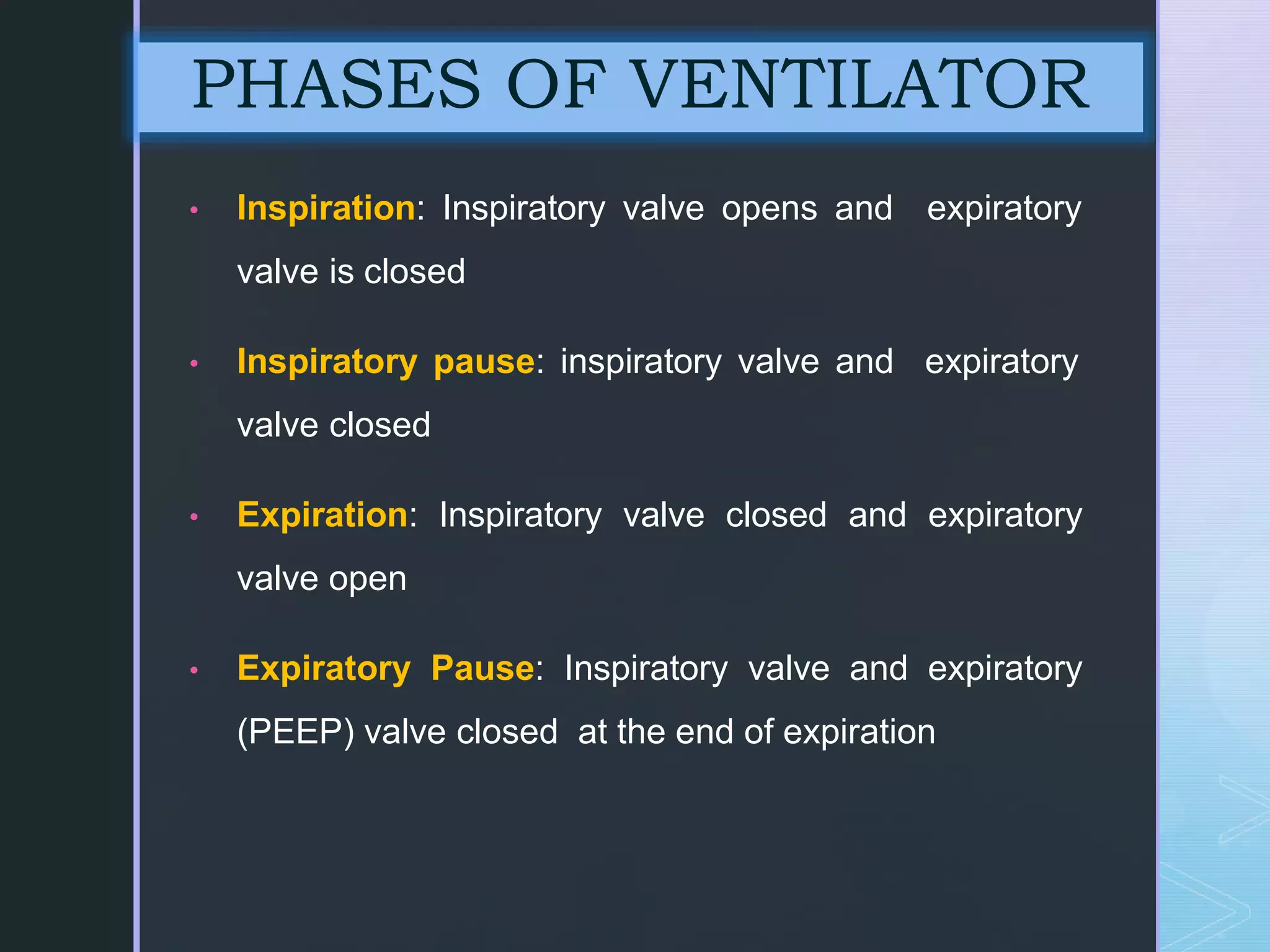
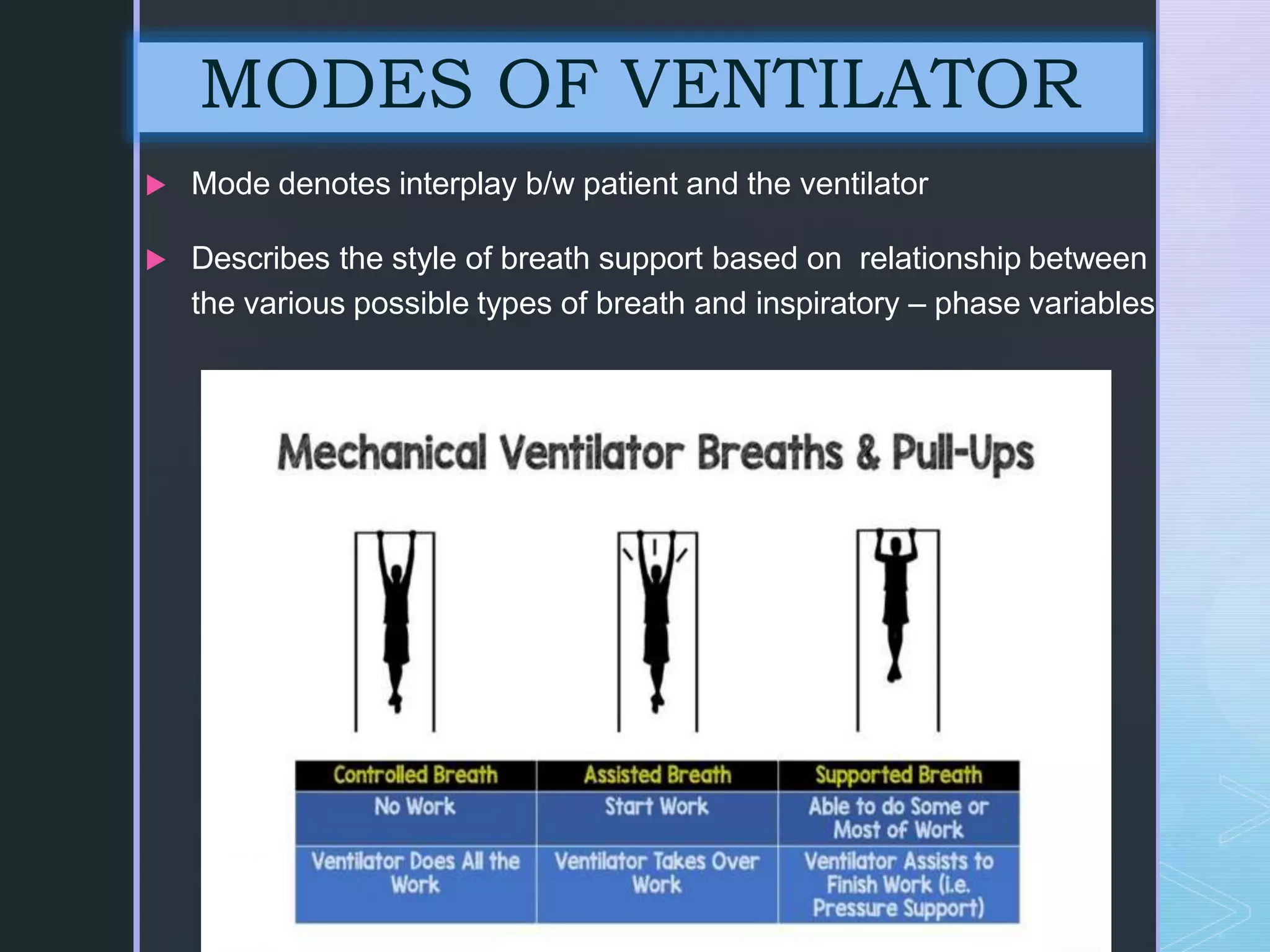
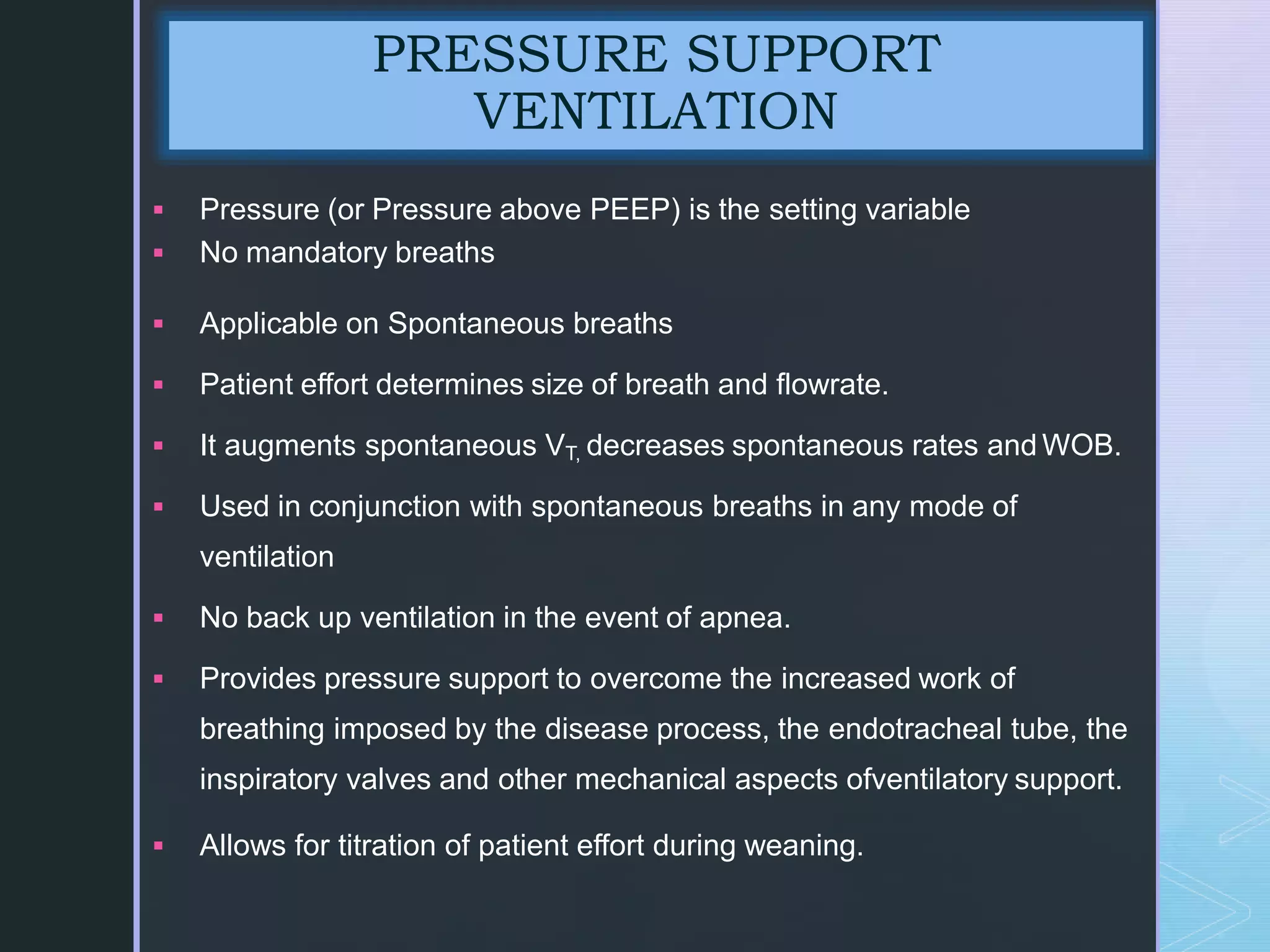
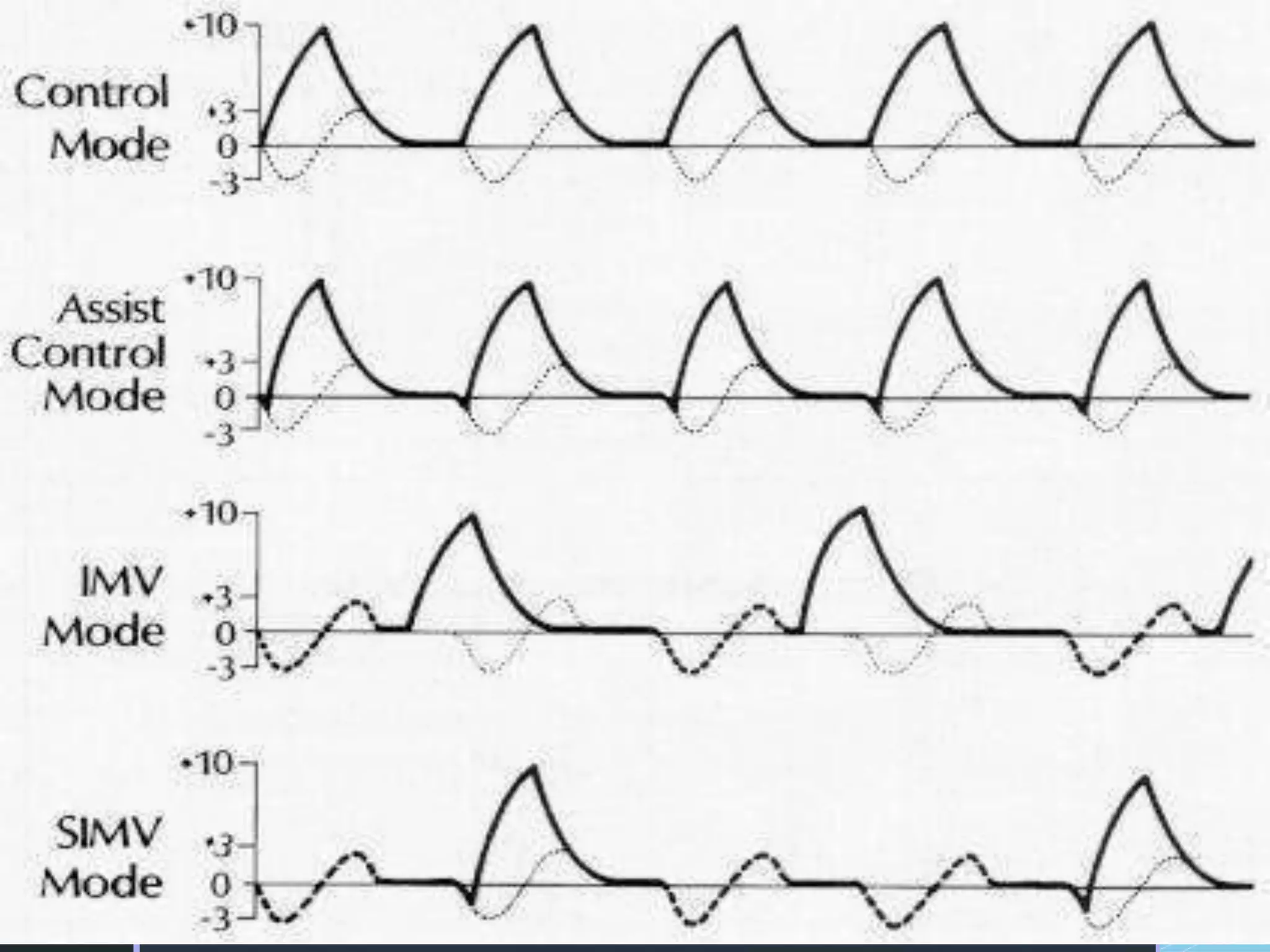
Mechanical ventilation involves using a ventilator to mechanically move air into and out of the lungs to maintain proper oxygen and carbon dioxide levels. It has several purposes including improving gas exchange, relieving respiratory distress, and avoiding complications. There are various modes of ventilation including pressure control, volume control, and time-cycled modes. Parameters like tidal volume, respiratory rate, and PEEP must be set and monitored appropriately for different patients and conditions.