This document provides an overview of obesity including its definition, prevalence, health consequences, assessment, treatment approaches, and guidelines. Some key points:
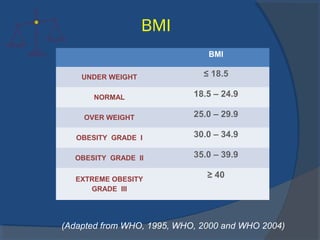
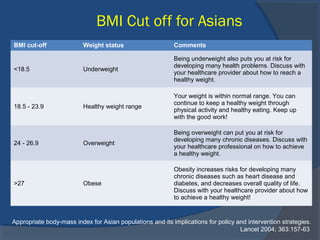
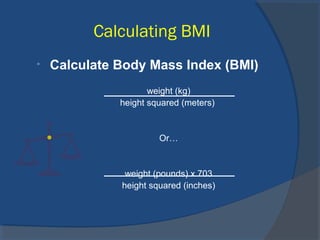
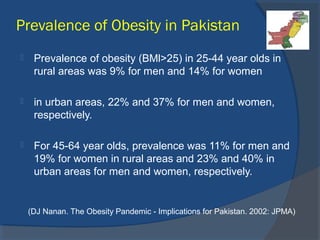
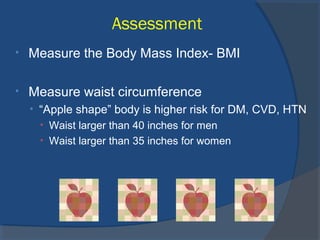
- Obesity is defined as a BMI of 30 or higher. It affects over 60 million US adults and rates have doubled globally in the last 30 years.
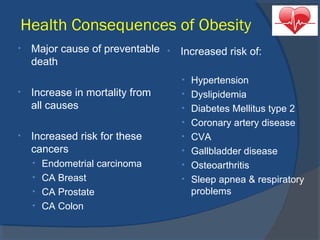
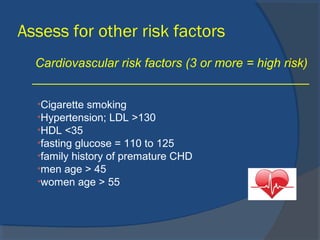
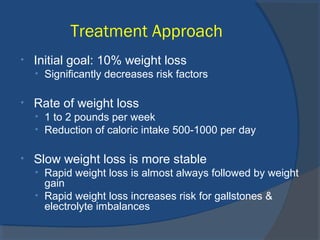
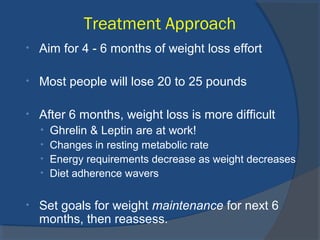
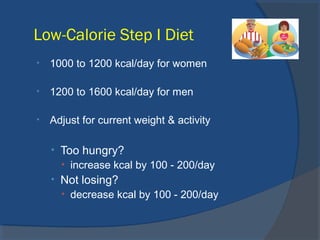
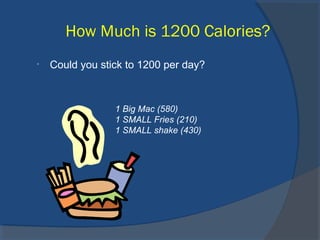
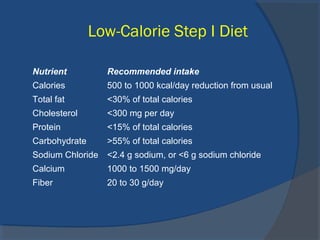
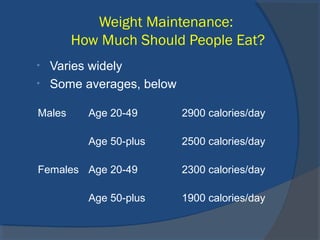
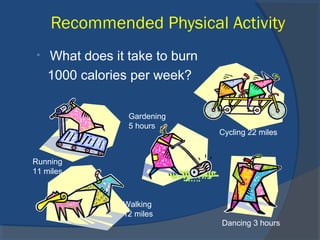
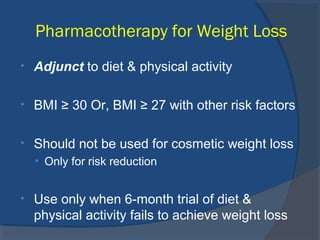
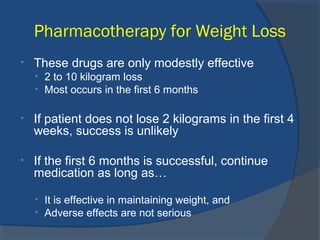
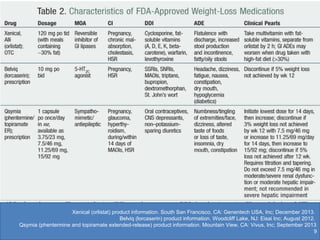
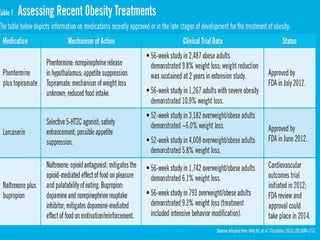
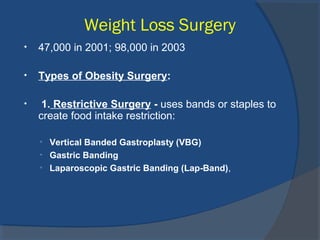
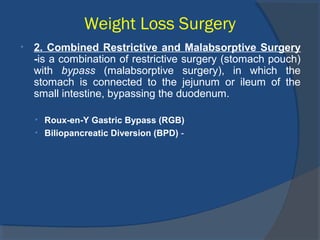
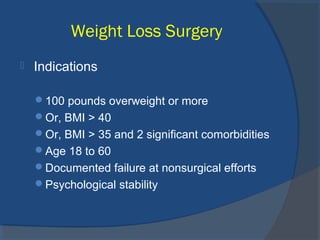
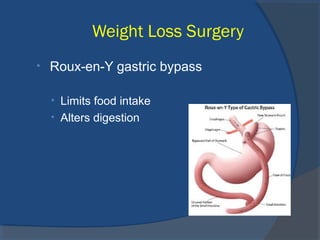
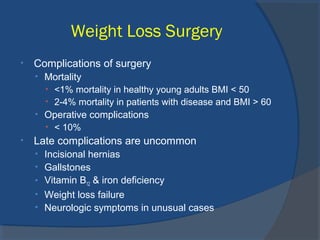
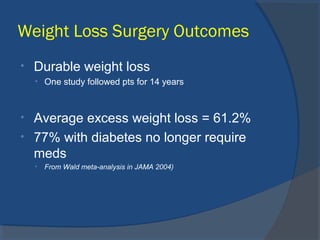
- It increases the risk of diseases like diabetes, heart disease, and cancer. Treatment involves diet, exercise, behavior change and sometimes medication or surgery.
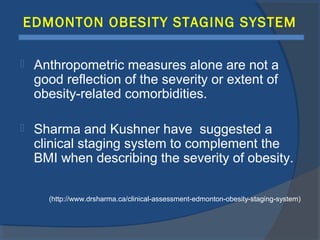
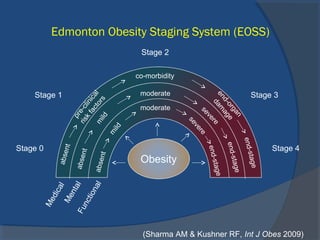
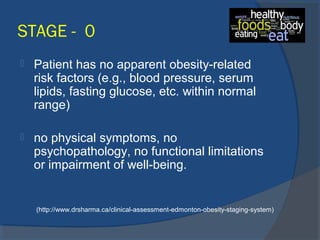
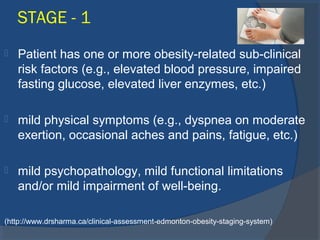
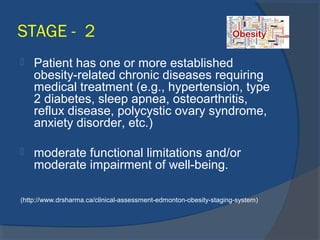
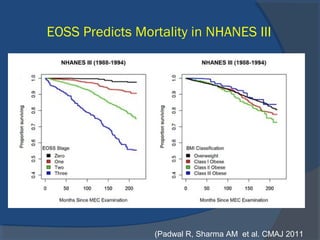
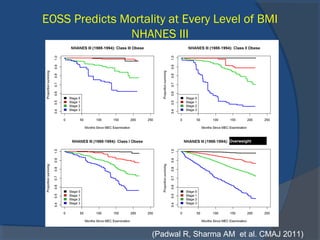
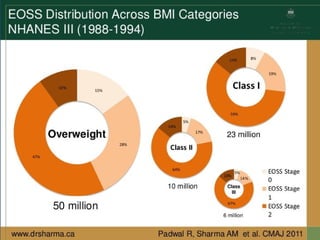
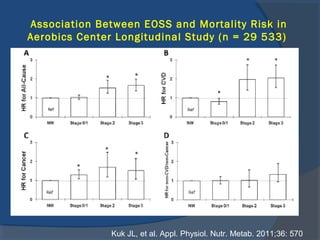
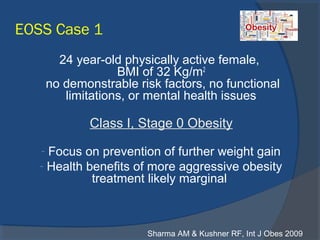
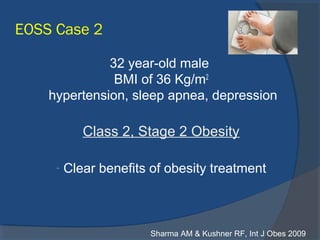
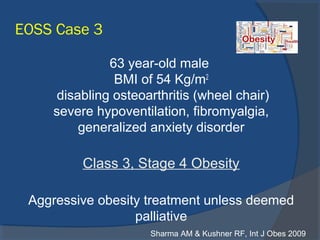
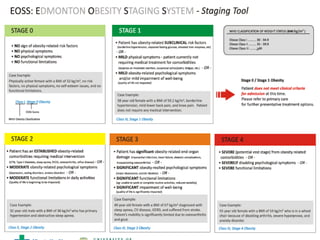
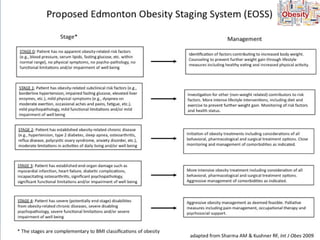
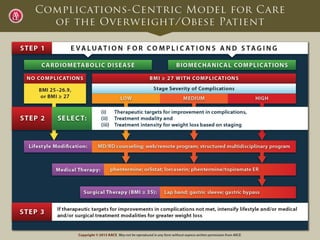
- The Edmonton Obesity Staging System complements BMI by assessing medical complications, functional limitations, and quality of life across 5 stages from no risk factors to end-stage disease.