The document discusses obesity, including its prevalence, complications, and treatment. Some key points:
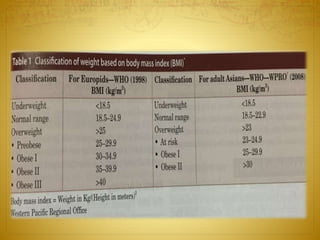
- Obesity is defined as having a BMI of over 30 or excess body fat of over 20%. It results from consuming more calories than expended.
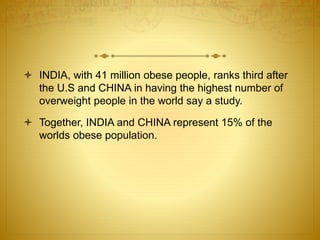
- It is common worldwide and in countries like India and China. In the US, over 30% of adults are obese, costing $147 billion annually.
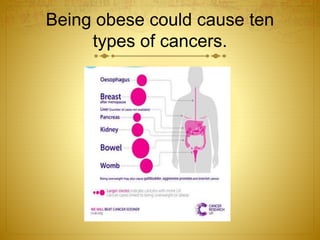
- Obesity increases the risk of conditions like diabetes, high blood pressure, high cholesterol, heart disease, stroke, arthritis, and some cancers.
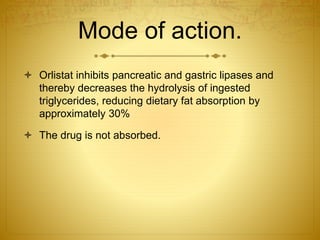
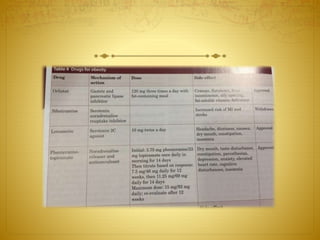
- Treatment involves lifestyle changes like diet and exercise. For higher-risk patients, treatment may include medication or surgery to help with weight loss and reduce