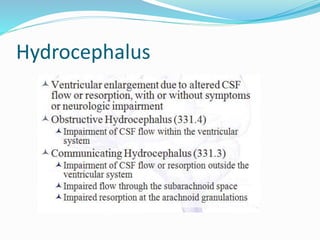
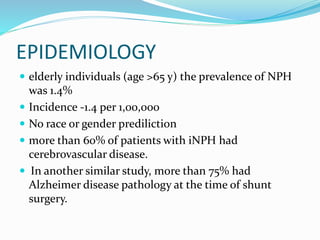
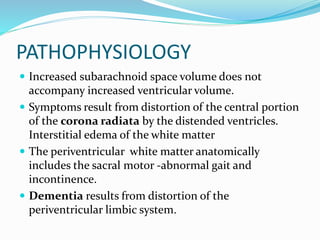
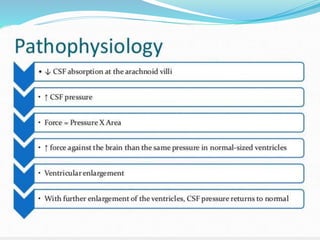
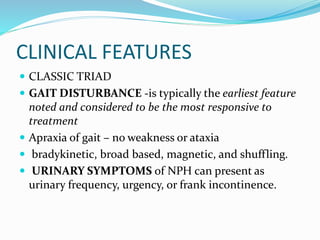
1) Normal pressure hydrocephalus (NPH) is characterized by abnormal gait, urinary incontinence, and dementia. It is most common in the elderly and can be caused by conditions like subarachnoid hemorrhage.
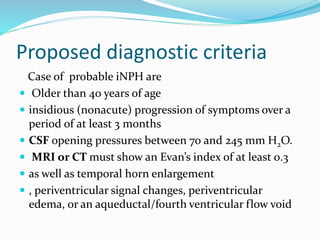
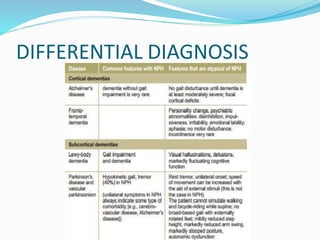
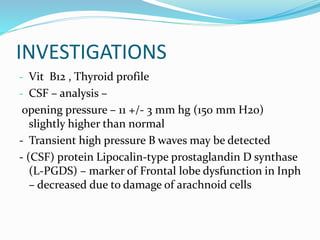
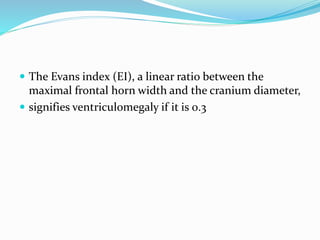
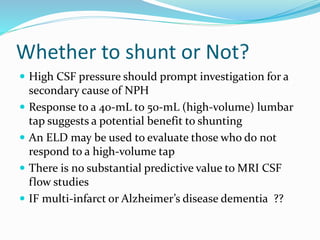
2) Diagnosis involves evaluating symptoms, imaging tests showing disproportionate ventricle enlargement, and tests like lumbar puncture to check CSF pressure and flow.
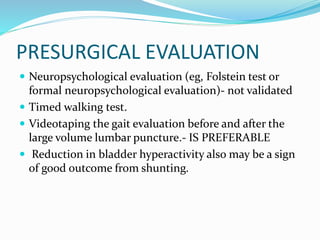
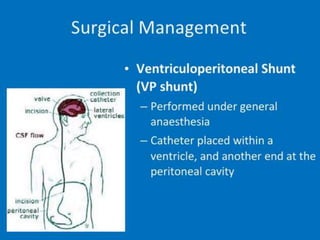
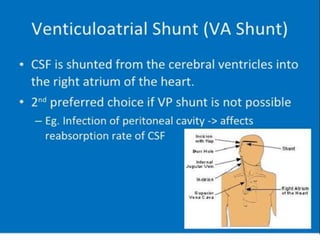
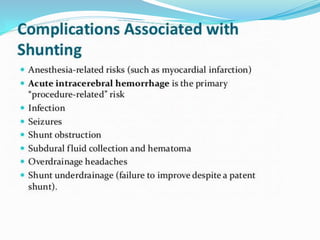
3) Treatment usually involves surgically placing a CSF shunt if symptoms improve with temporary drainage, with benefits seen in 50-61% of cases but also a high risk of complications.