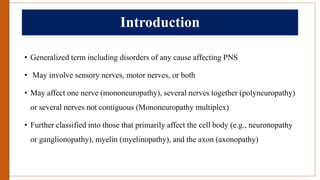
This document provides an overview of peripheral neuropathy, including:
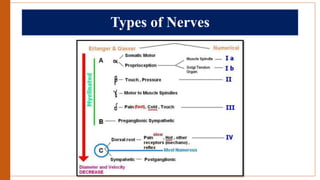
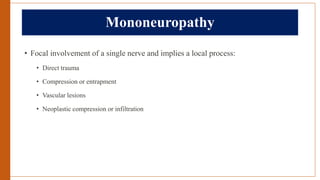
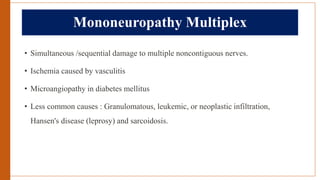
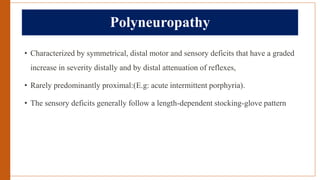
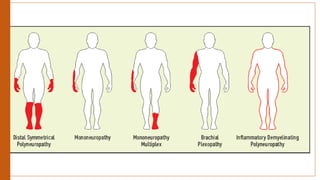
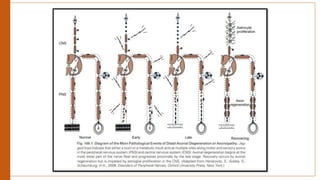
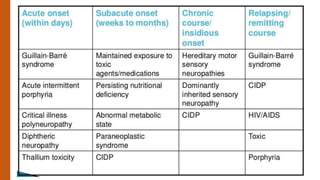
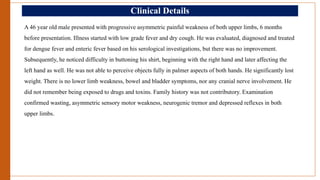
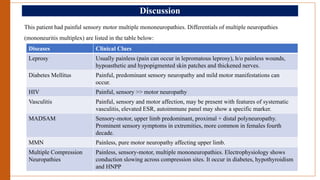
- Types of peripheral neuropathy are classified based on whether they primarily affect motor nerves, sensory nerves, or both.
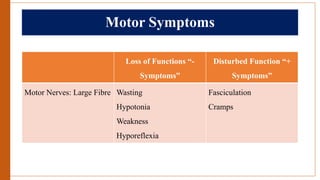
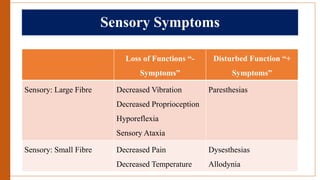
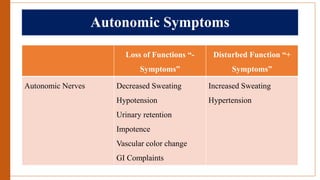
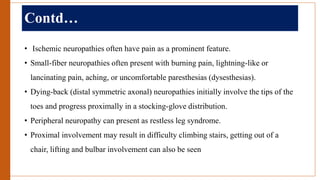
- The main symptoms of motor, sensory, and autonomic neuropathies are described.
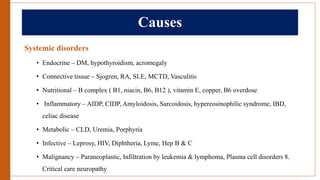
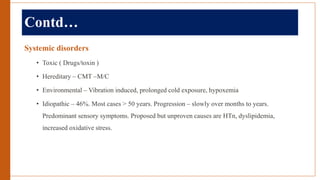
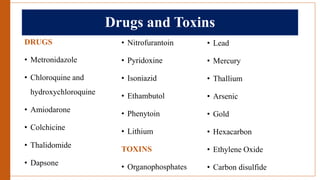
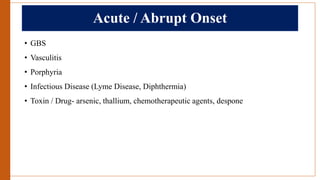
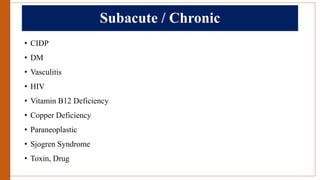
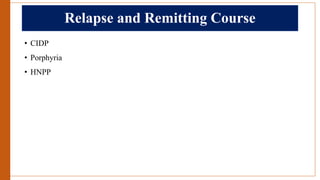
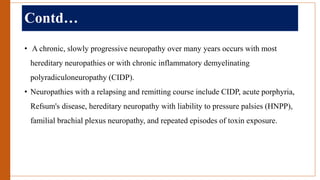
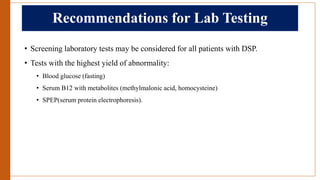
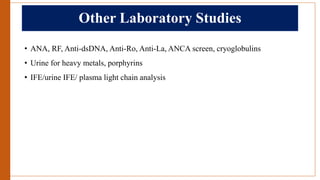
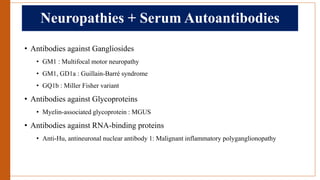
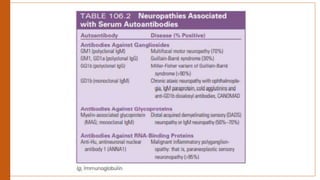
- The most common causes of peripheral neuropathy include systemic disorders like diabetes, connective tissue diseases, nutritional deficiencies, infections, malignancies and toxic neuropathies.
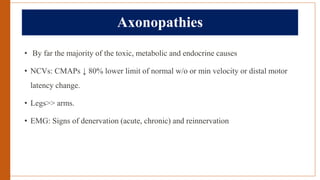
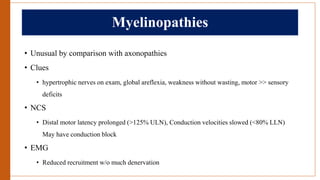
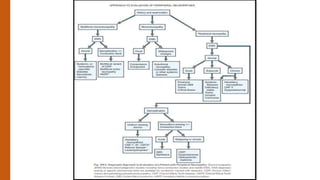
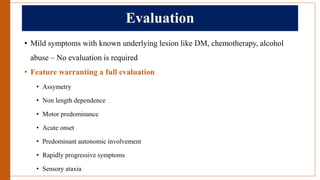
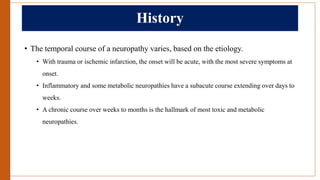
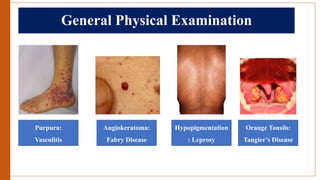
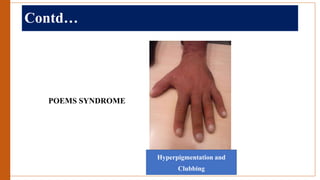
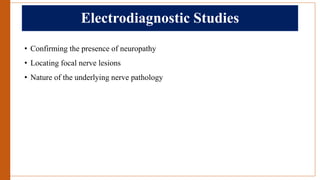
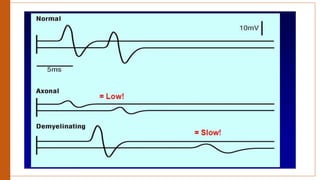
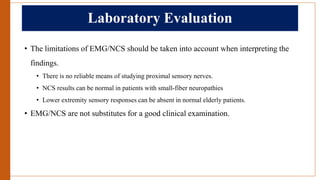
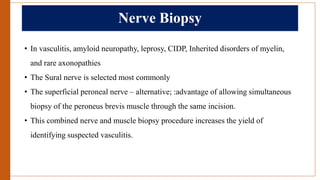
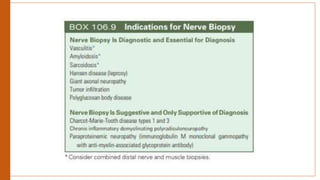
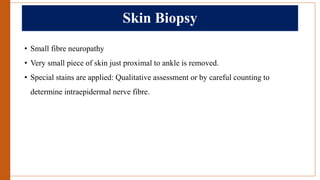
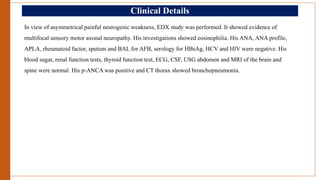
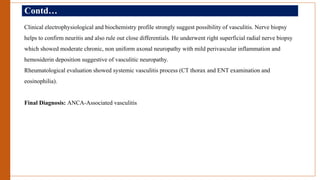
- The approach to evaluating a patient with peripheral neuropathy involves obtaining a history, neurological exam, electrodiagnostic studies and sometimes nerve biopsy to identify the location and cause of the neuropathy.