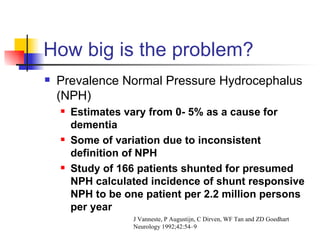
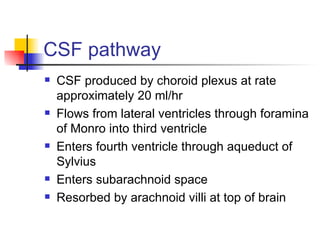
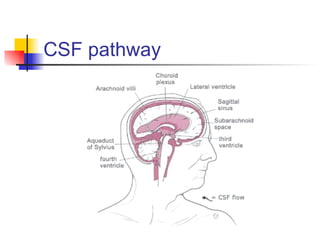
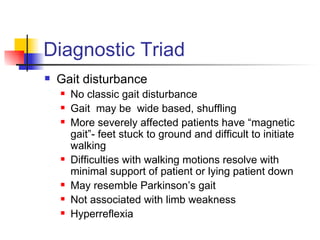
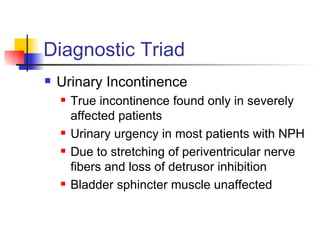
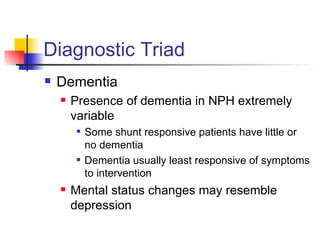
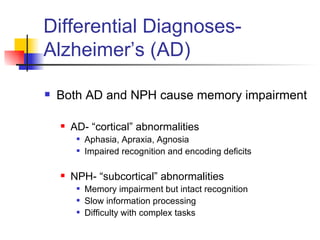
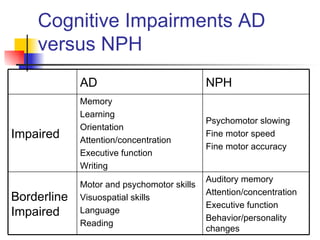
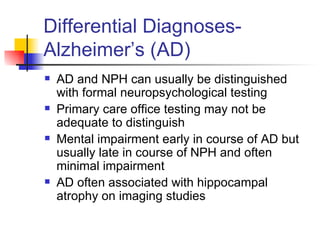
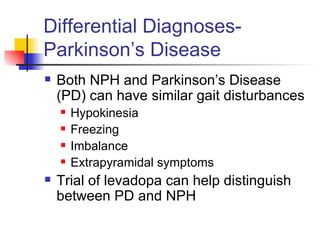
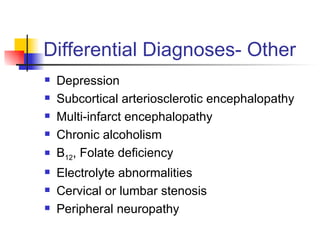
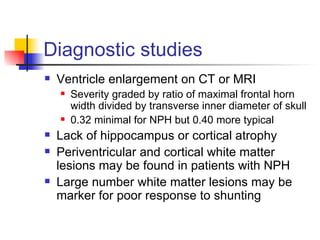
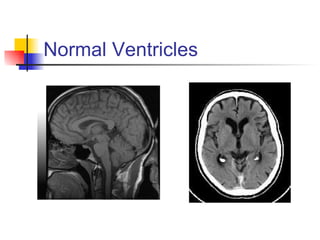
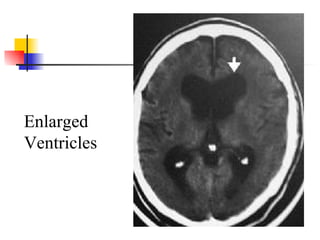
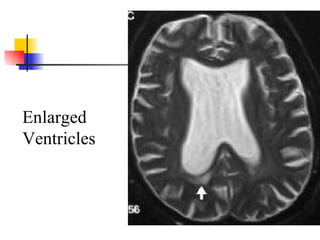
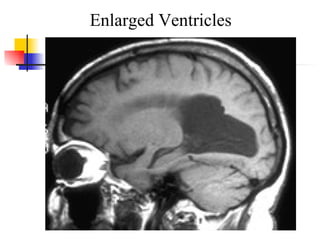
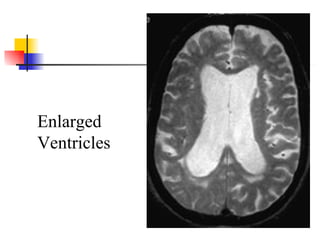
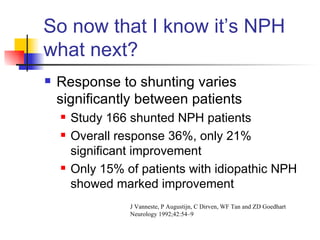
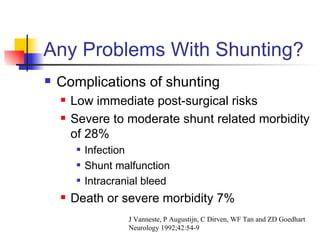
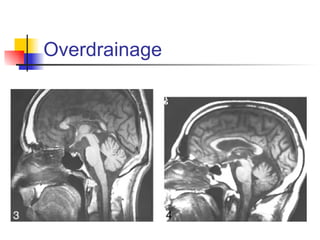
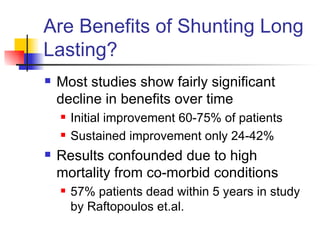
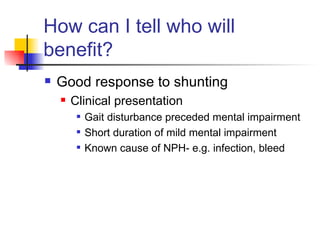
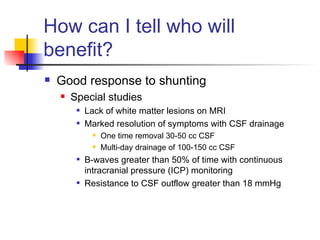
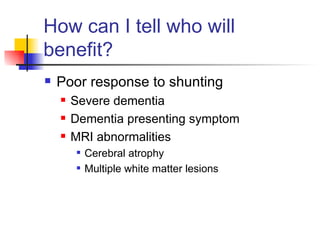
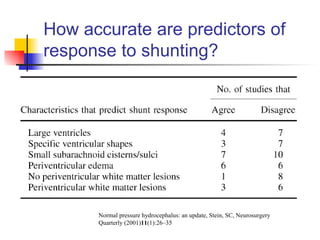
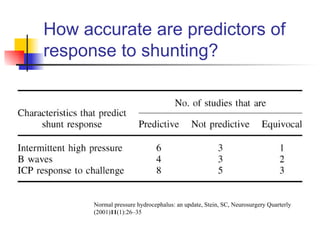
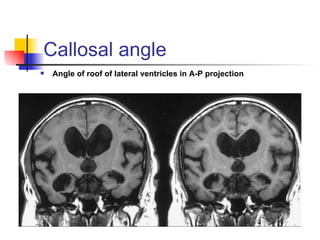
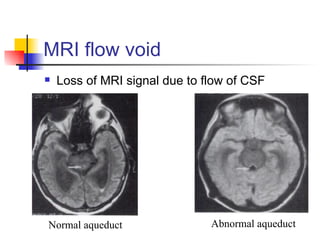
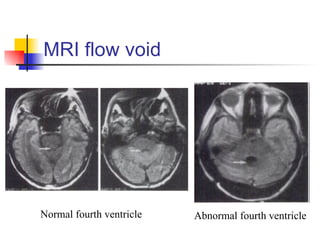
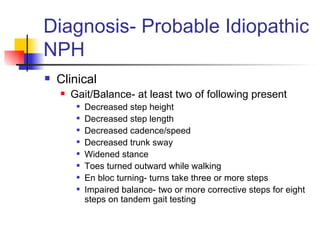
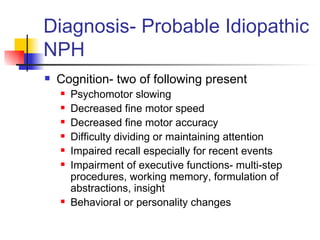
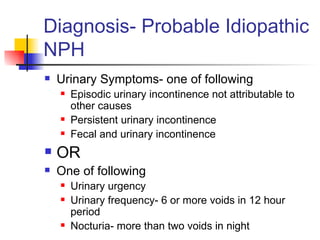
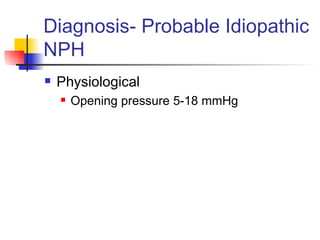
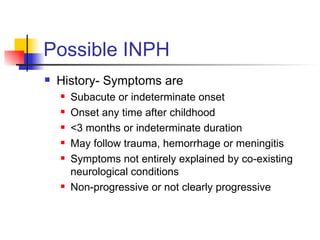
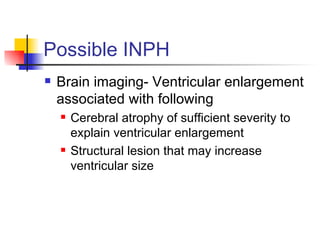
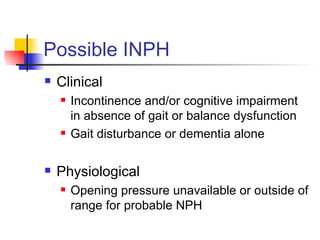
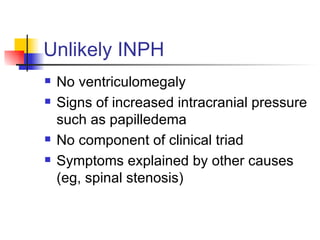
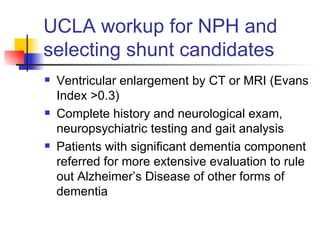
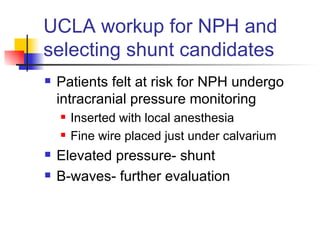
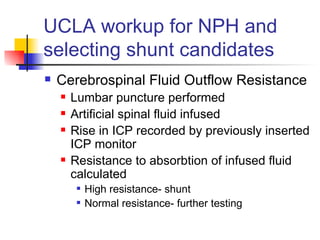
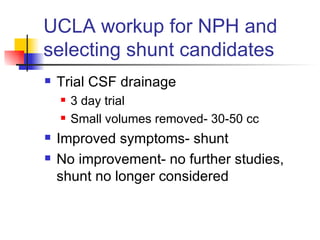
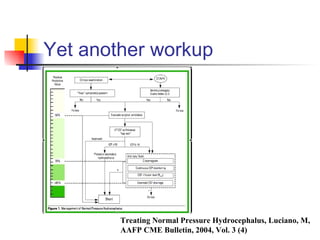
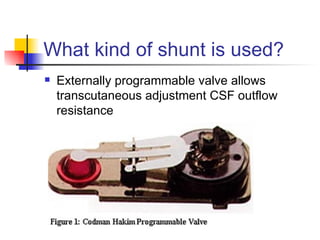
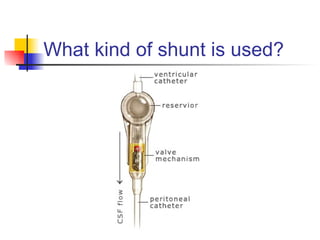
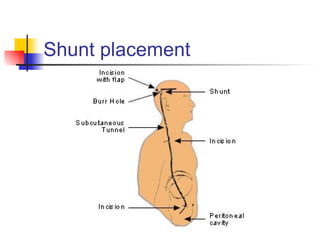
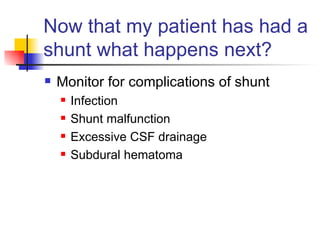
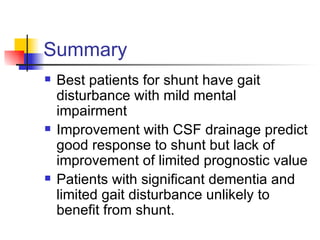
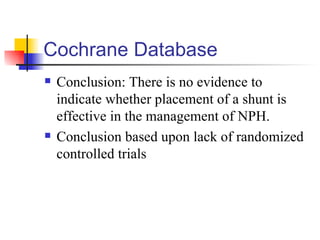
This document provides information on normal pressure hydrocephalus (NPH), including its causes, symptoms, diagnosis, treatment with shunt surgery, and patient outcomes. It discusses how NPH presents with a triad of gait disturbance, urinary incontinence, and dementia. Diagnostic tests include brain imaging and CSF flow studies. Patients with mild symptoms and gait issues are most likely to benefit from shunt surgery, while those with significant dementia tend to show little improvement. However, long-term outcomes of shunt surgery are variable, with benefits often declining over time.