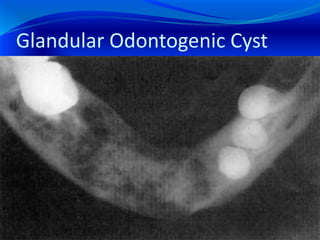
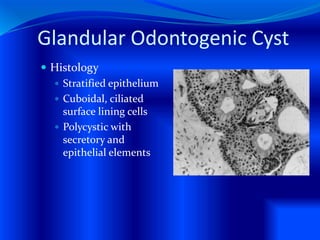
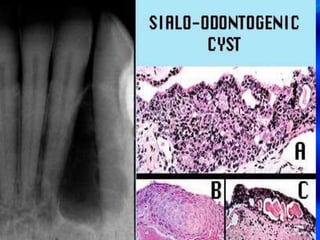
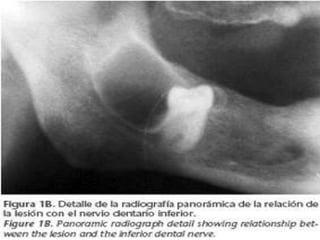
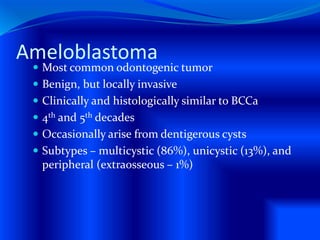
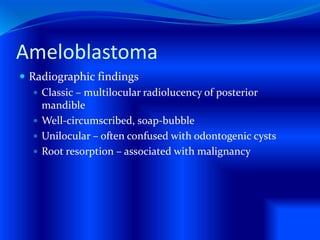
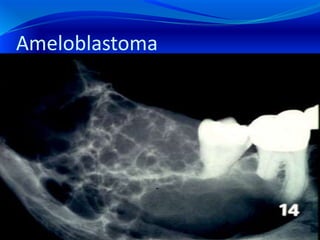
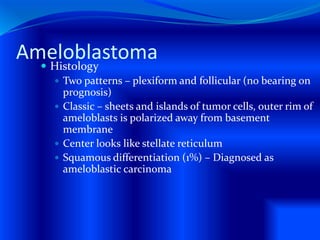
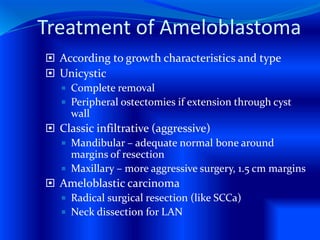
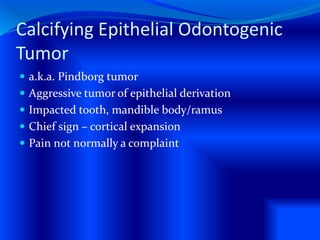
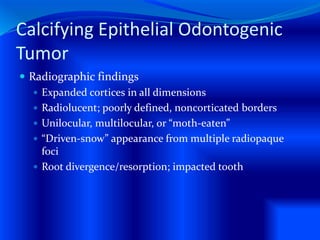
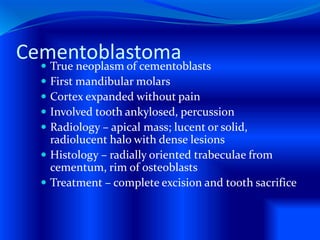
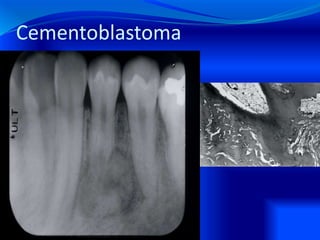
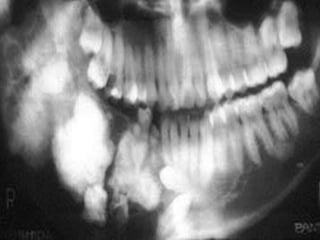
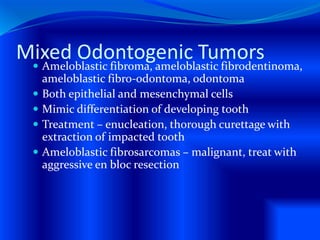
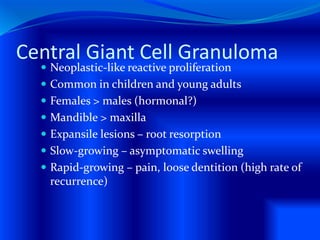
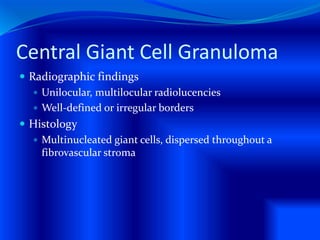
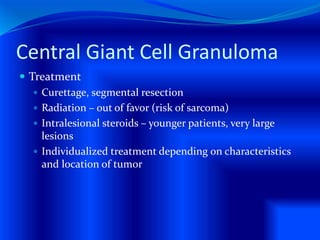
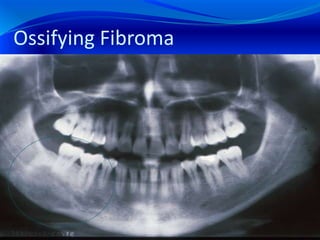
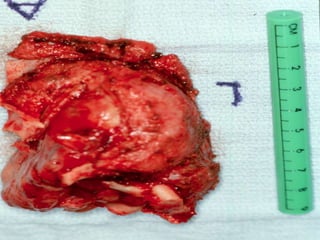
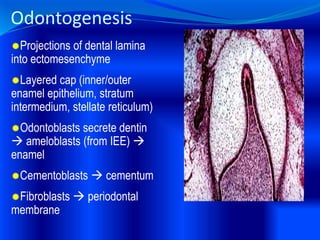
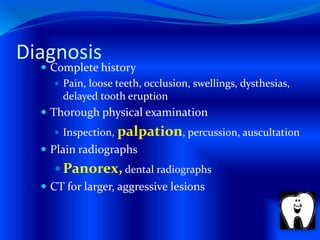
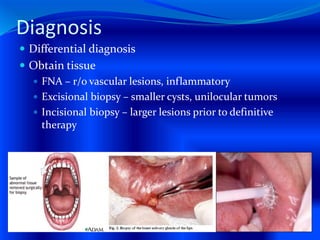
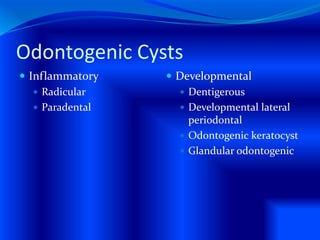
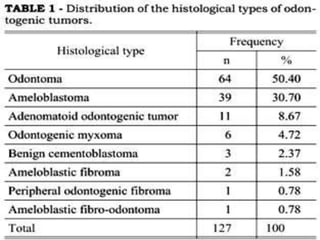
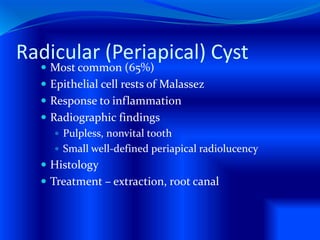
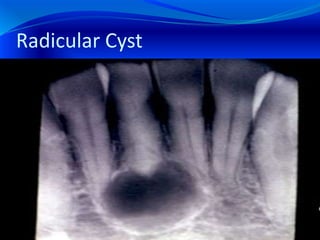
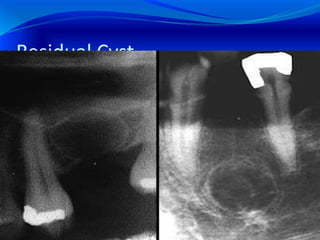
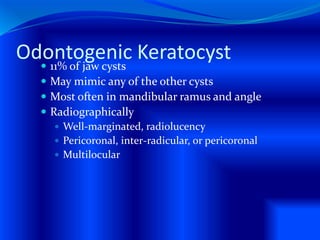
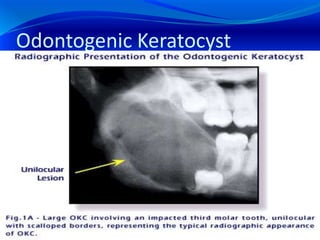
The document provides an overview of various odontogenic cysts and tumors, including their pathology, diagnosis, and treatment options. It covers types such as radicular, dentigerous, and odontogenic keratocysts, as well as tumors like ameloblastoma and calcifying epithelial odontogenic tumors. Diagnosis involves clinical assessment and radiographic findings, while treatment varies from enucleation to more aggressive surgical interventions.












![Glandular Odontogenic Cyst
More recently described (45 cases)
Gardner, 1988
Mandible (87%), usually anterior
Very slow progressive growth (CC: swelling, pain
[40%])
Radiographic findings
Unilocular or multilocular radiolucency](https://image.slidesharecdn.com/odontogenictumors-101117205541-phpapp02/85/Odontogenic-tumors-34-320.jpg)