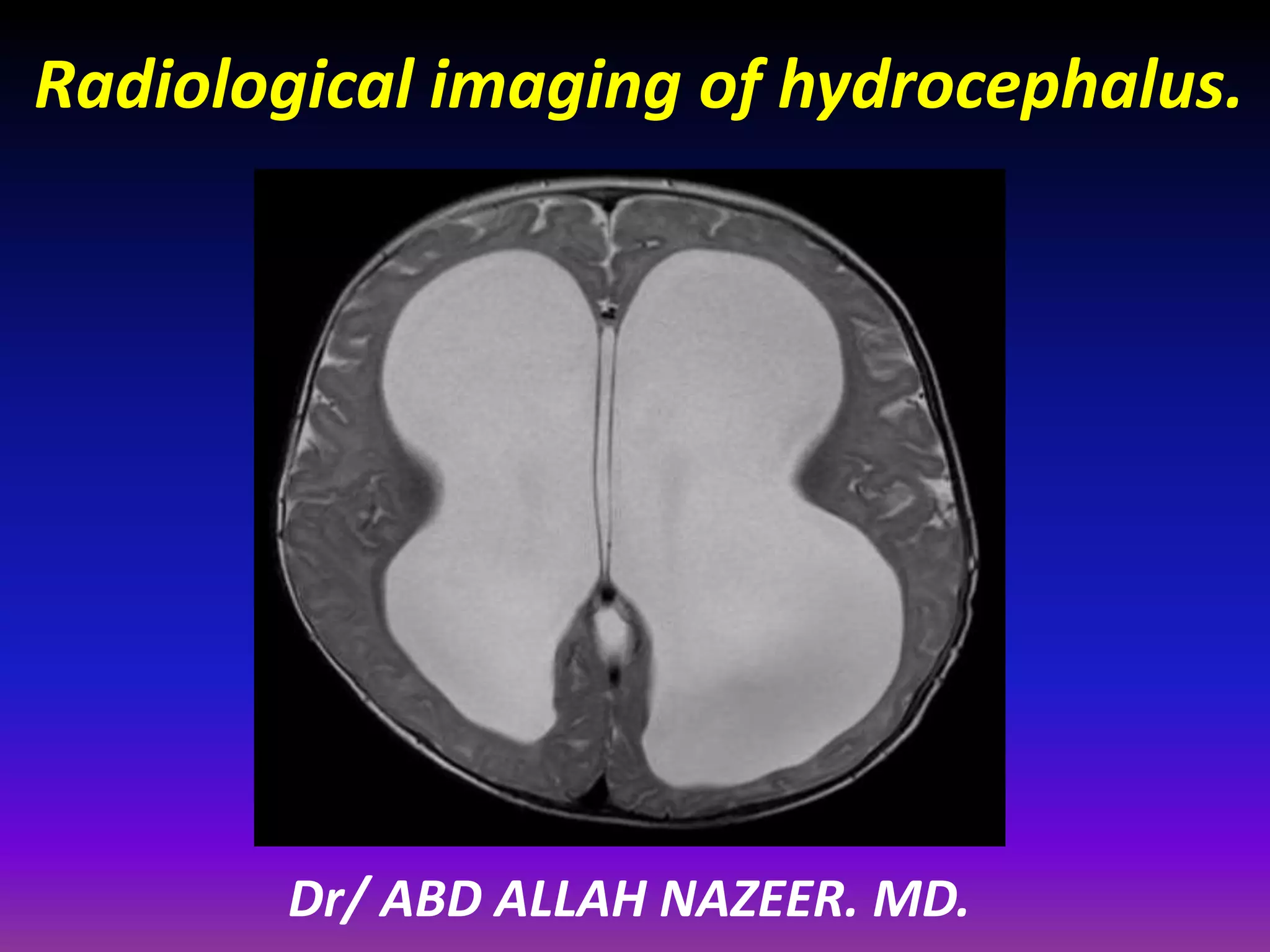
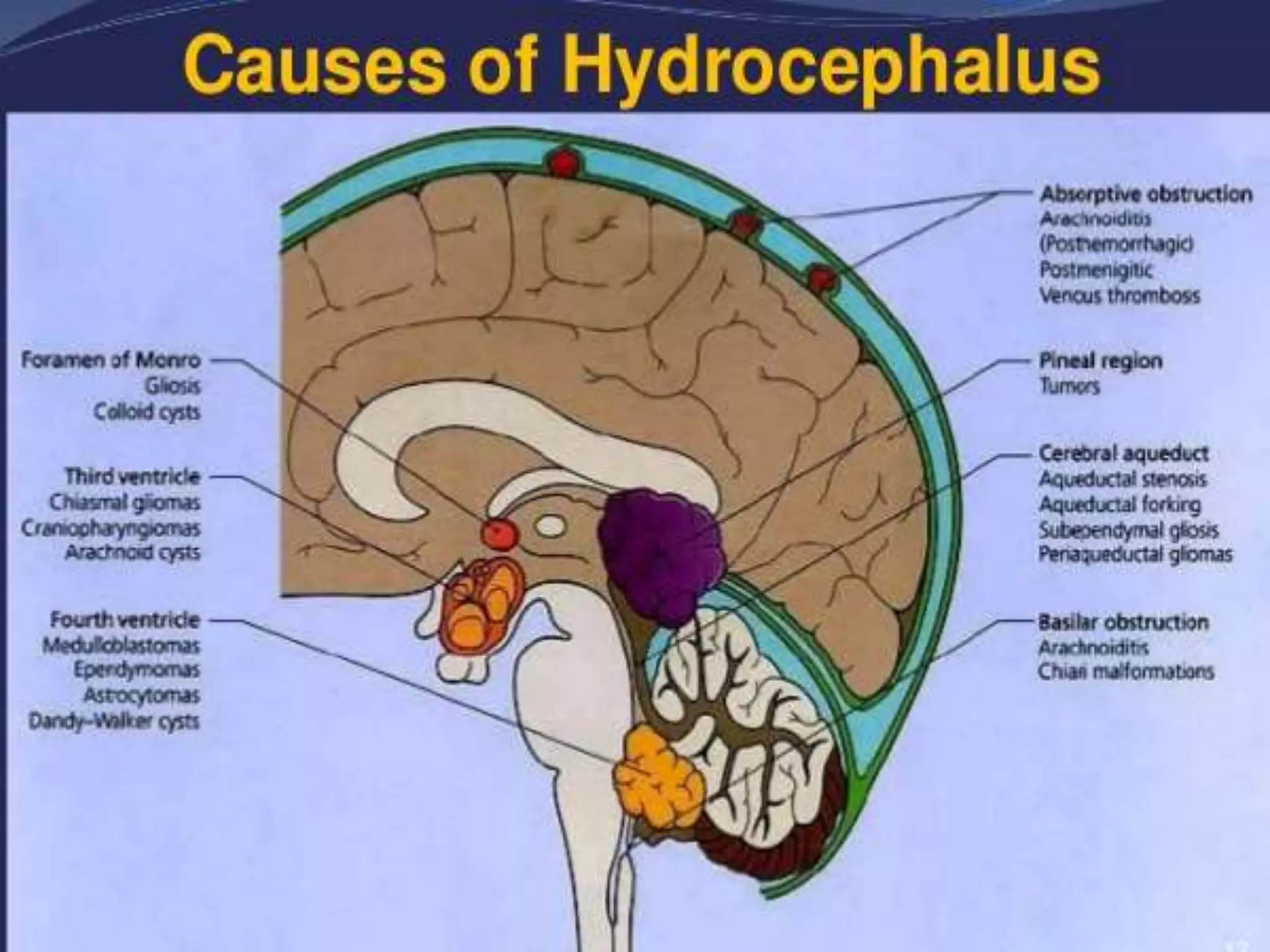
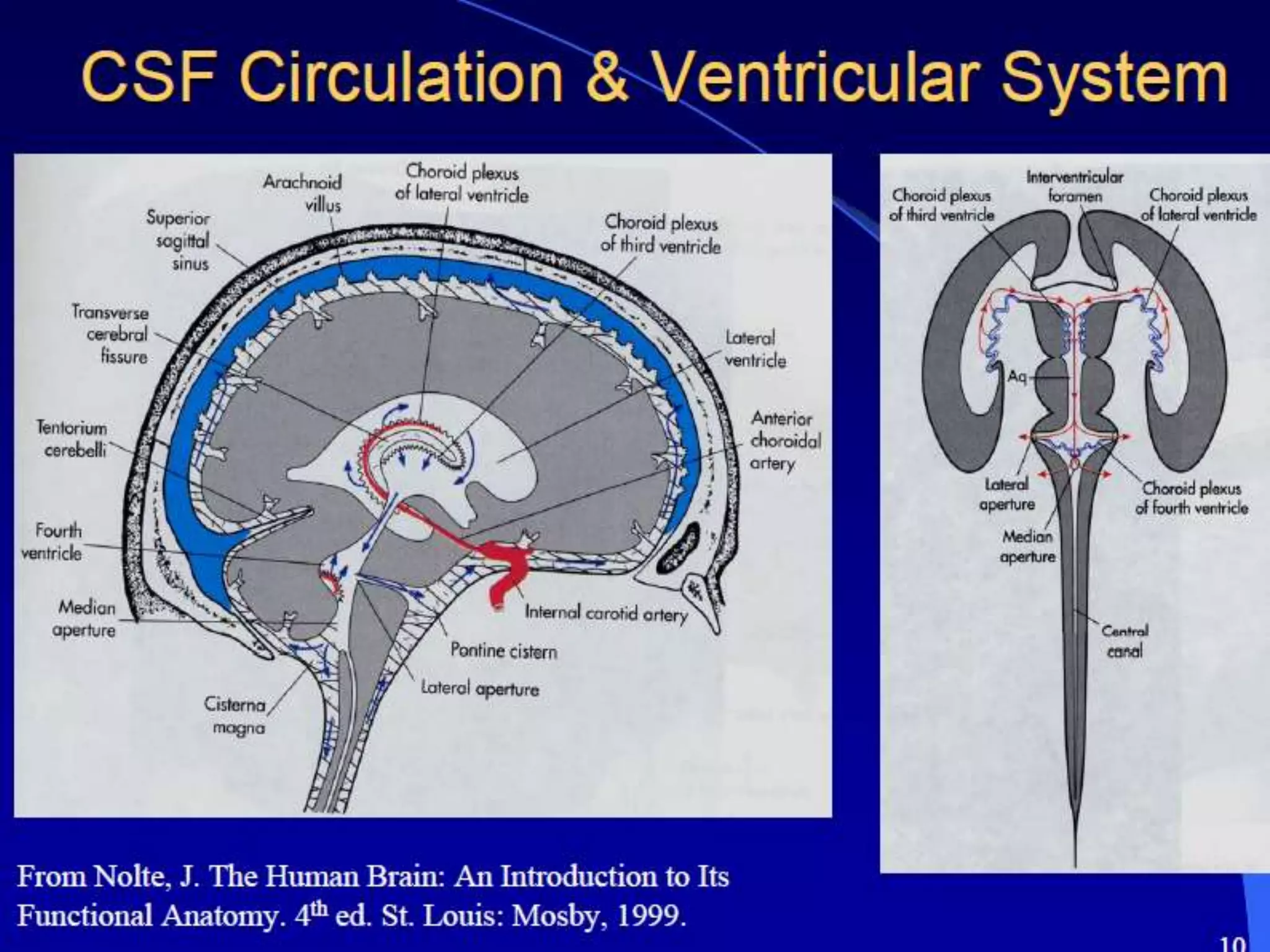
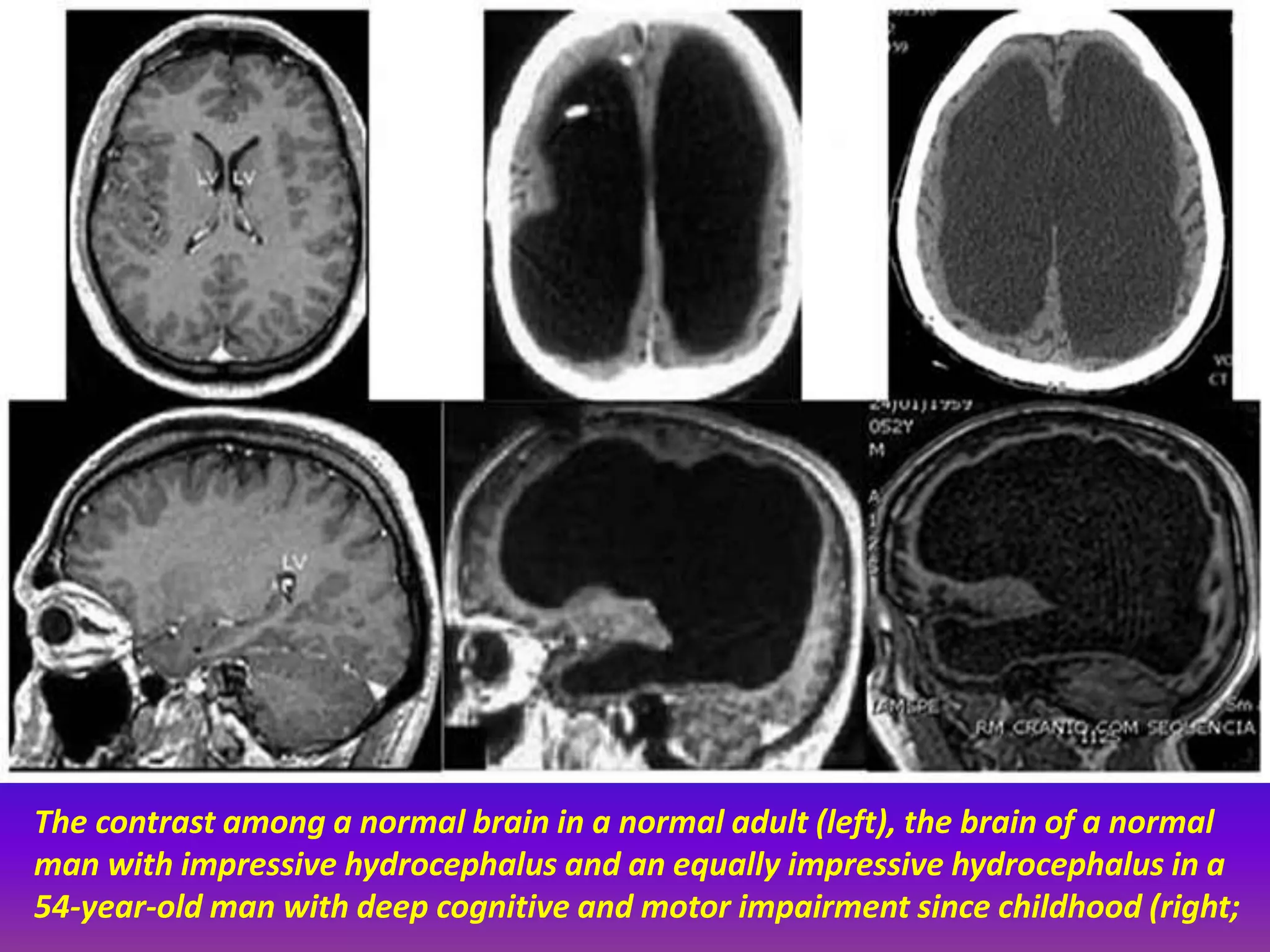
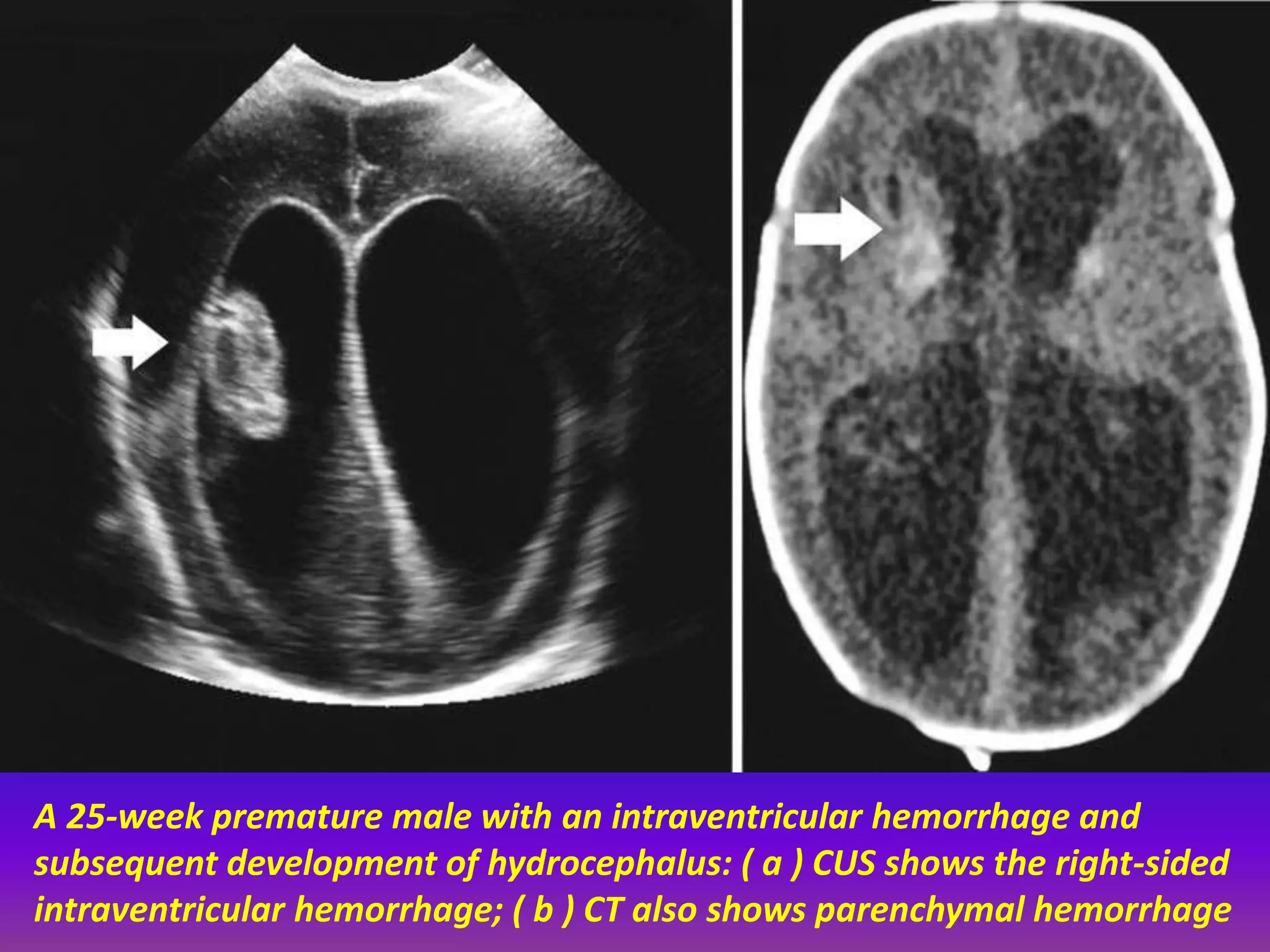
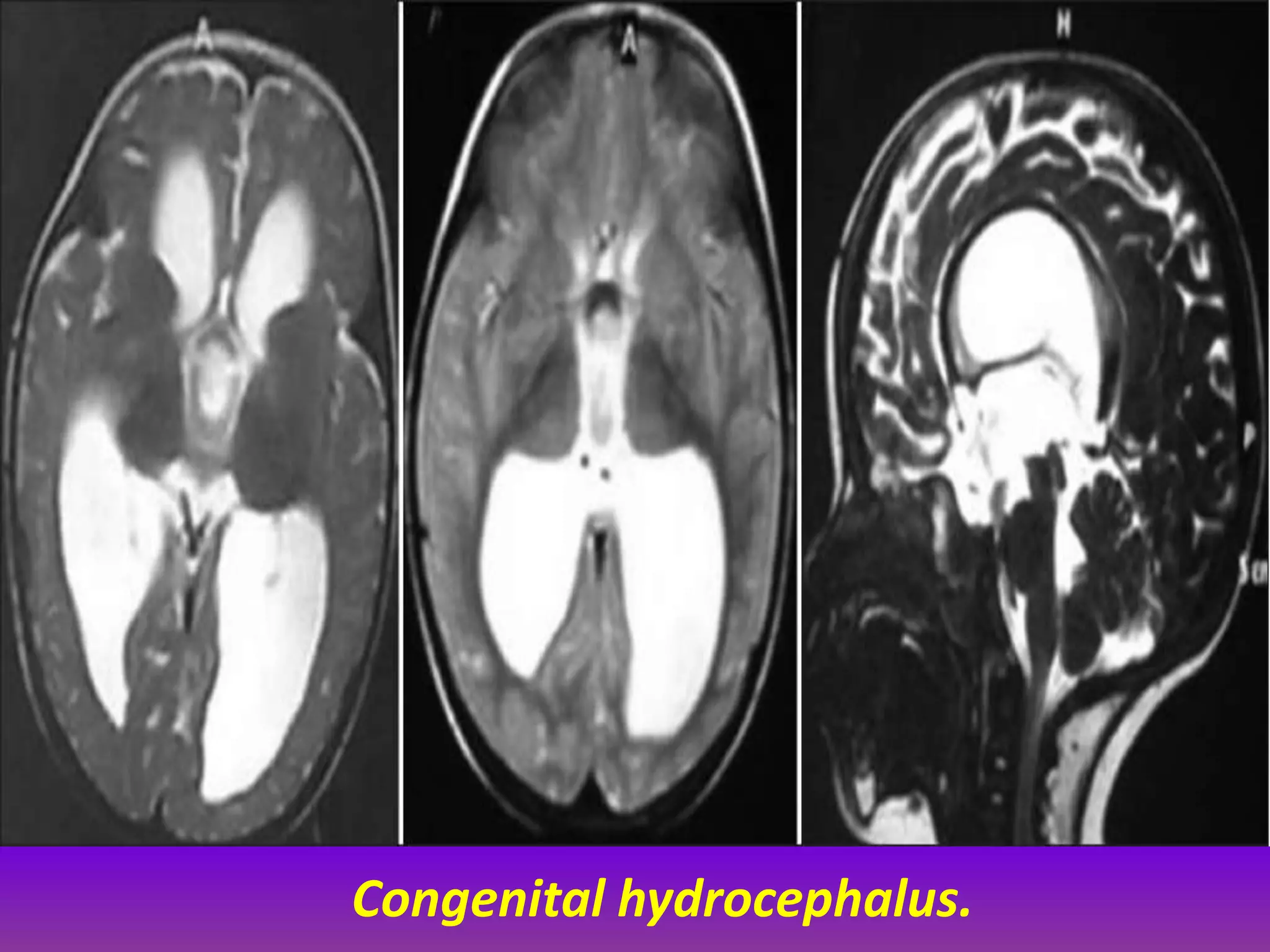
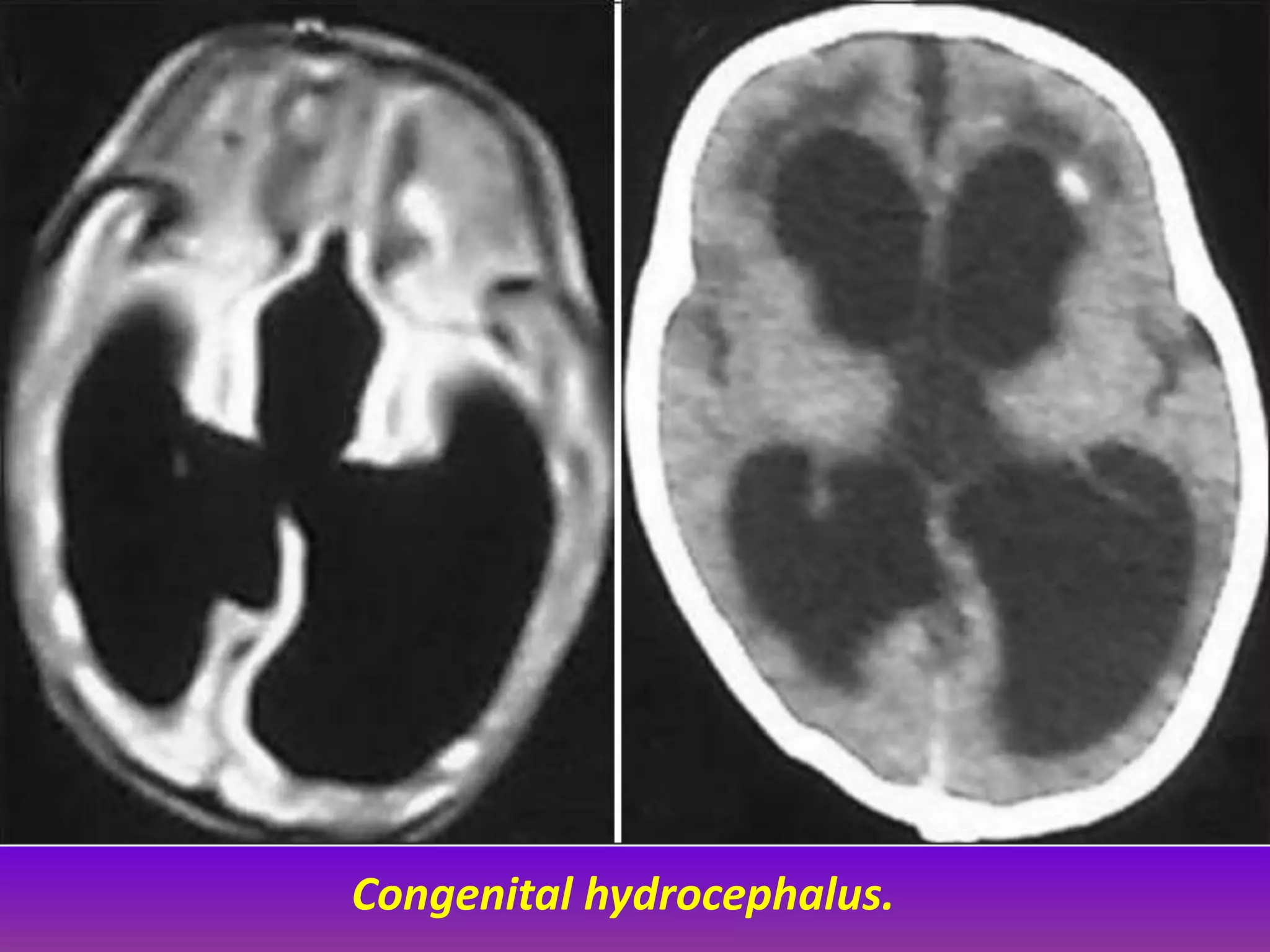
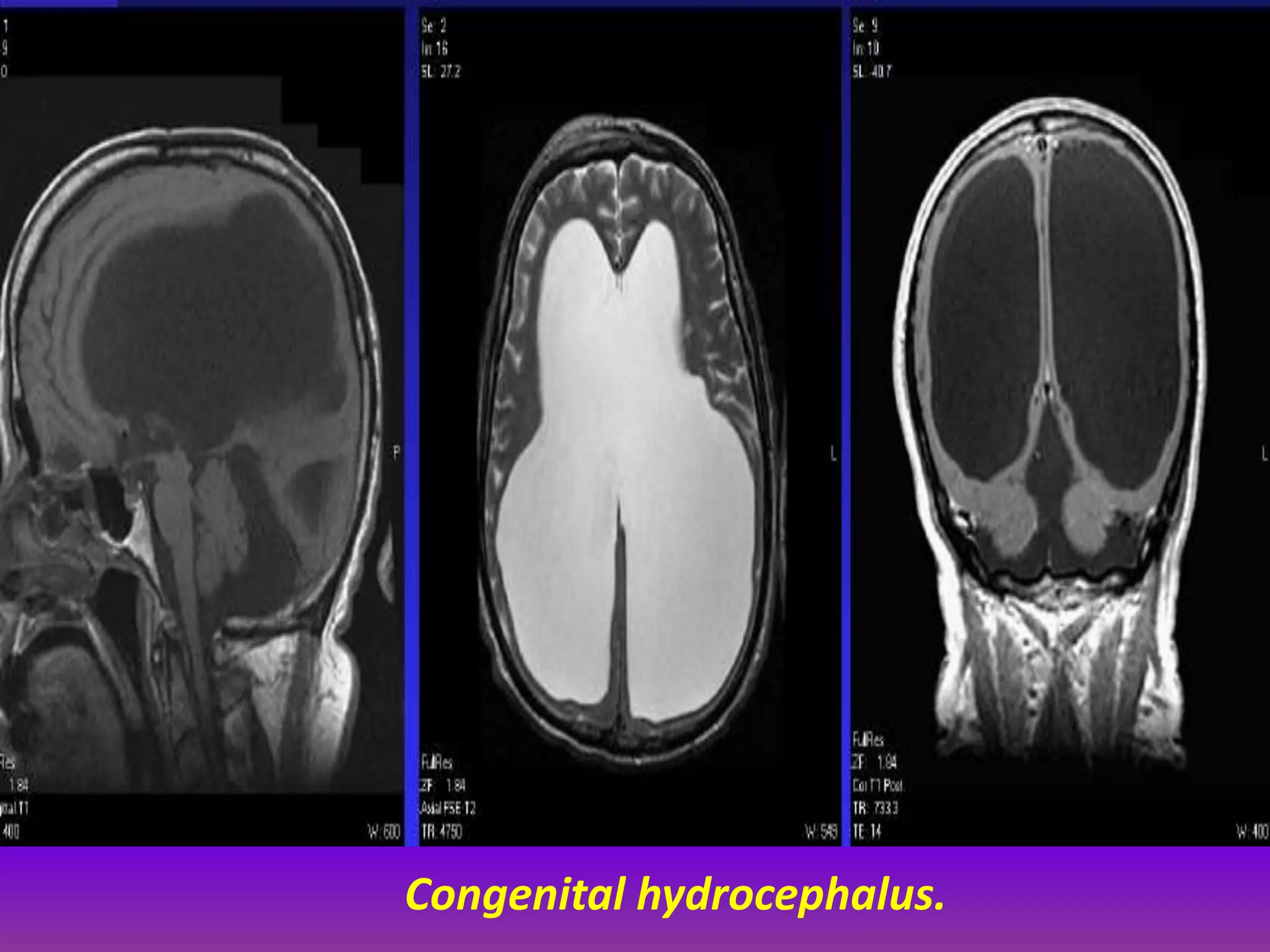
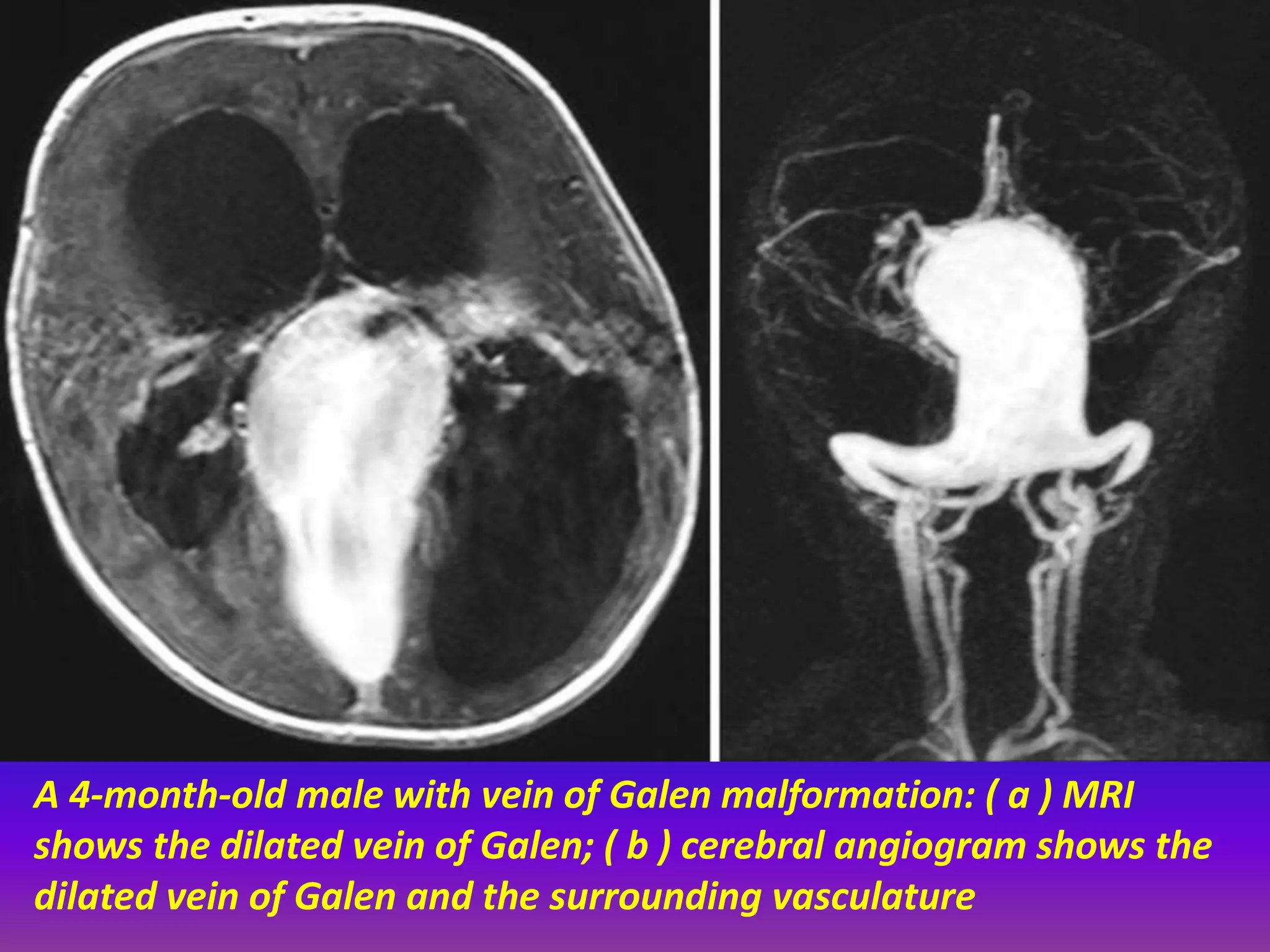
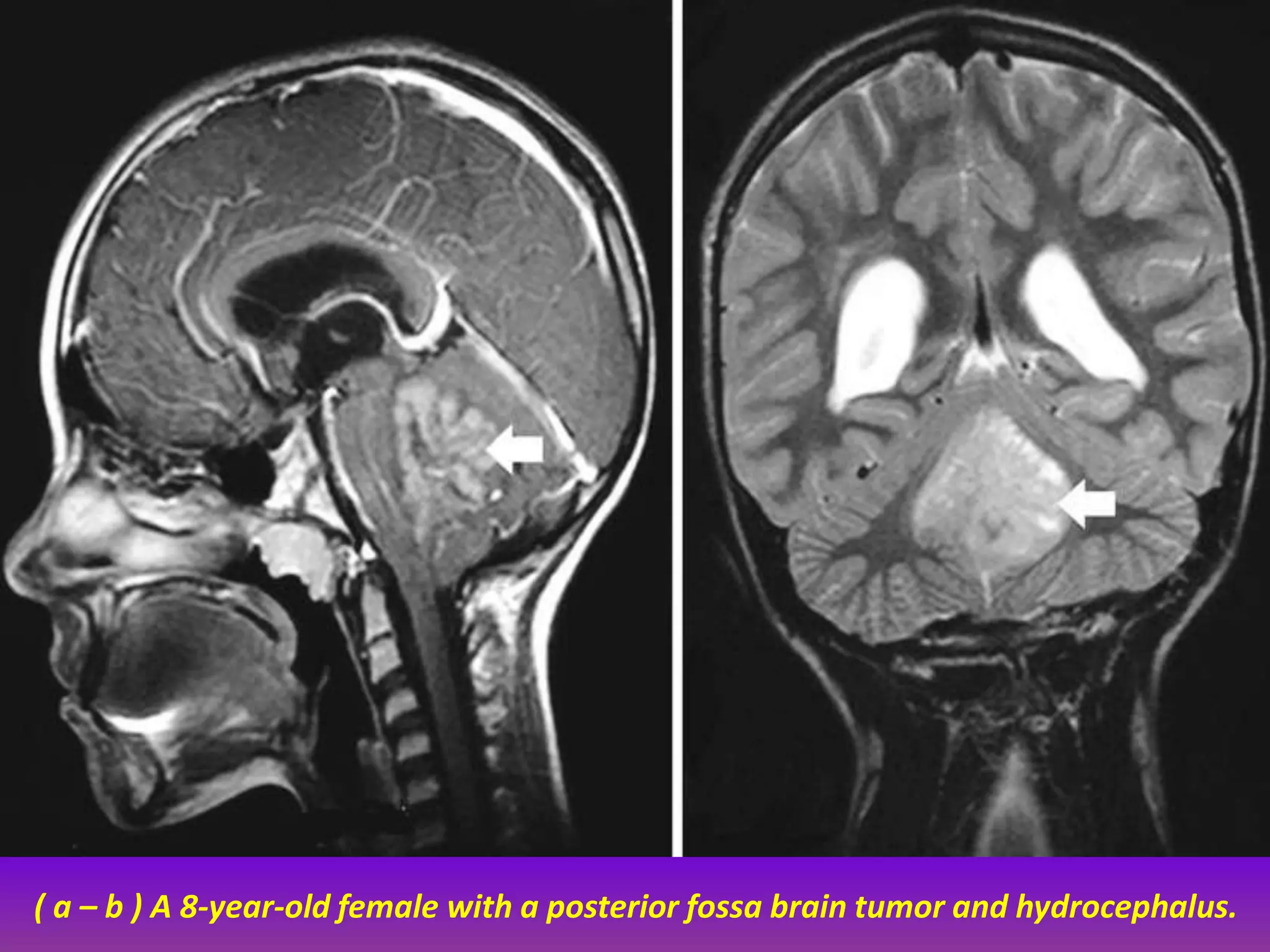
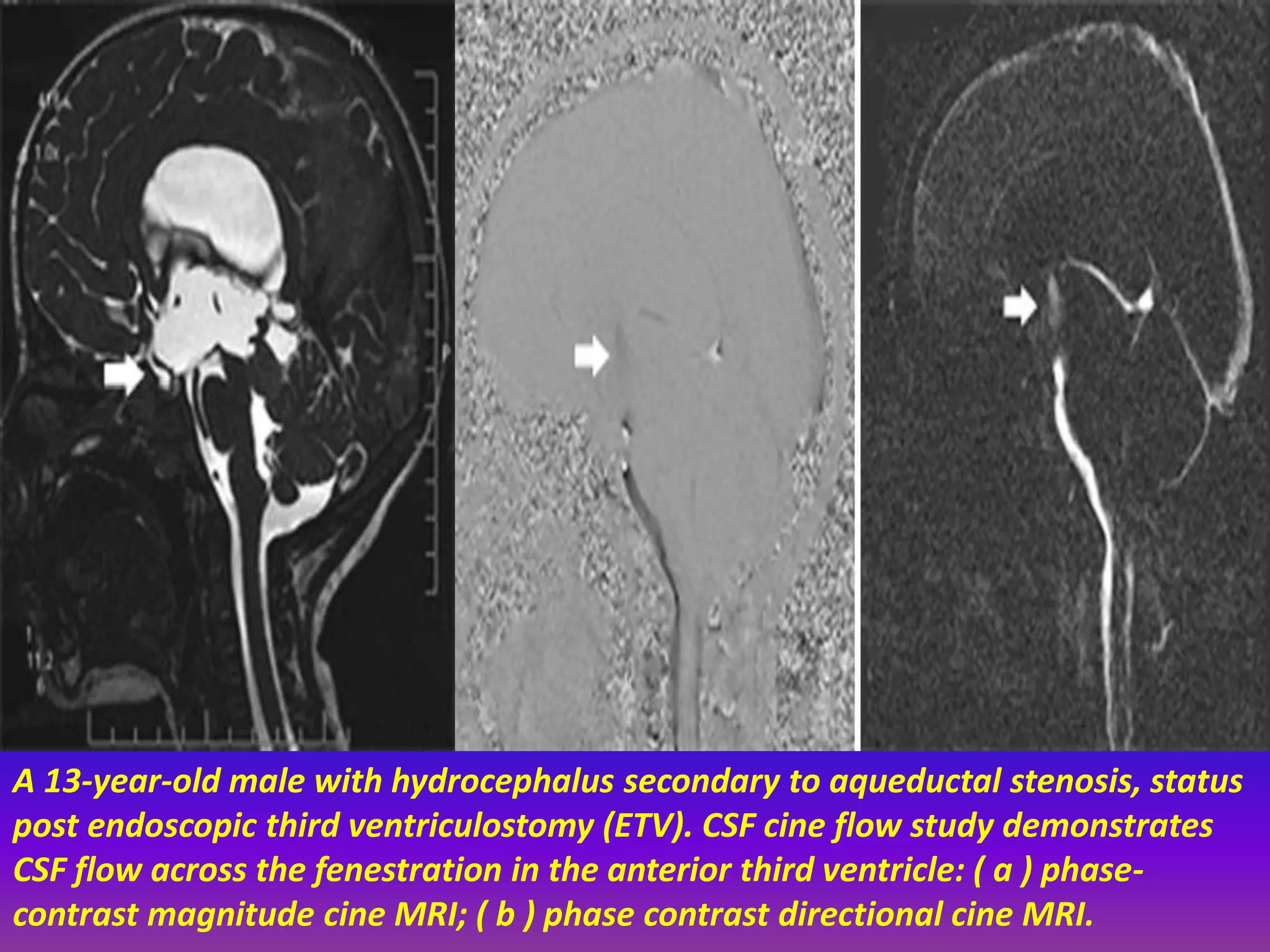
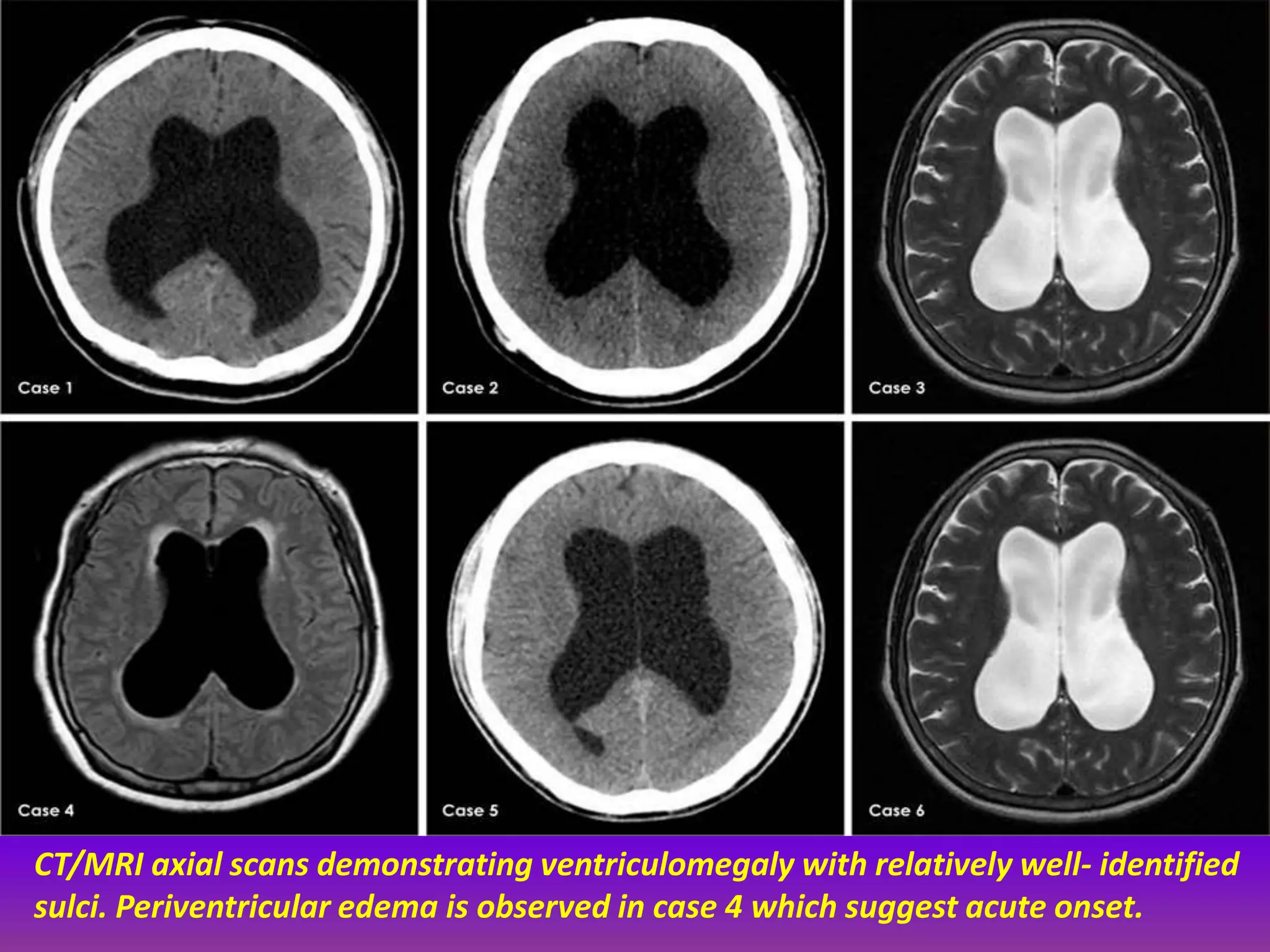
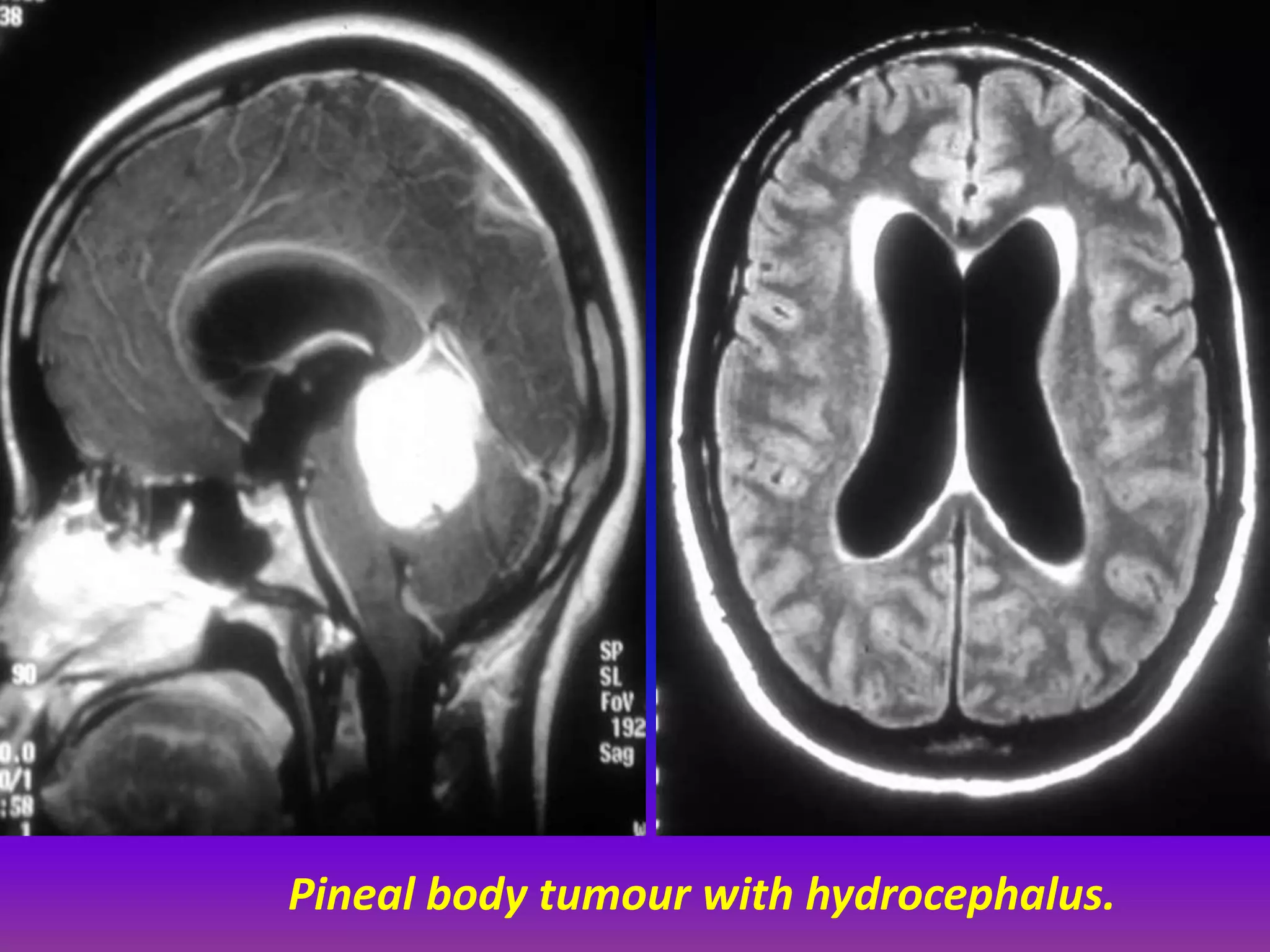
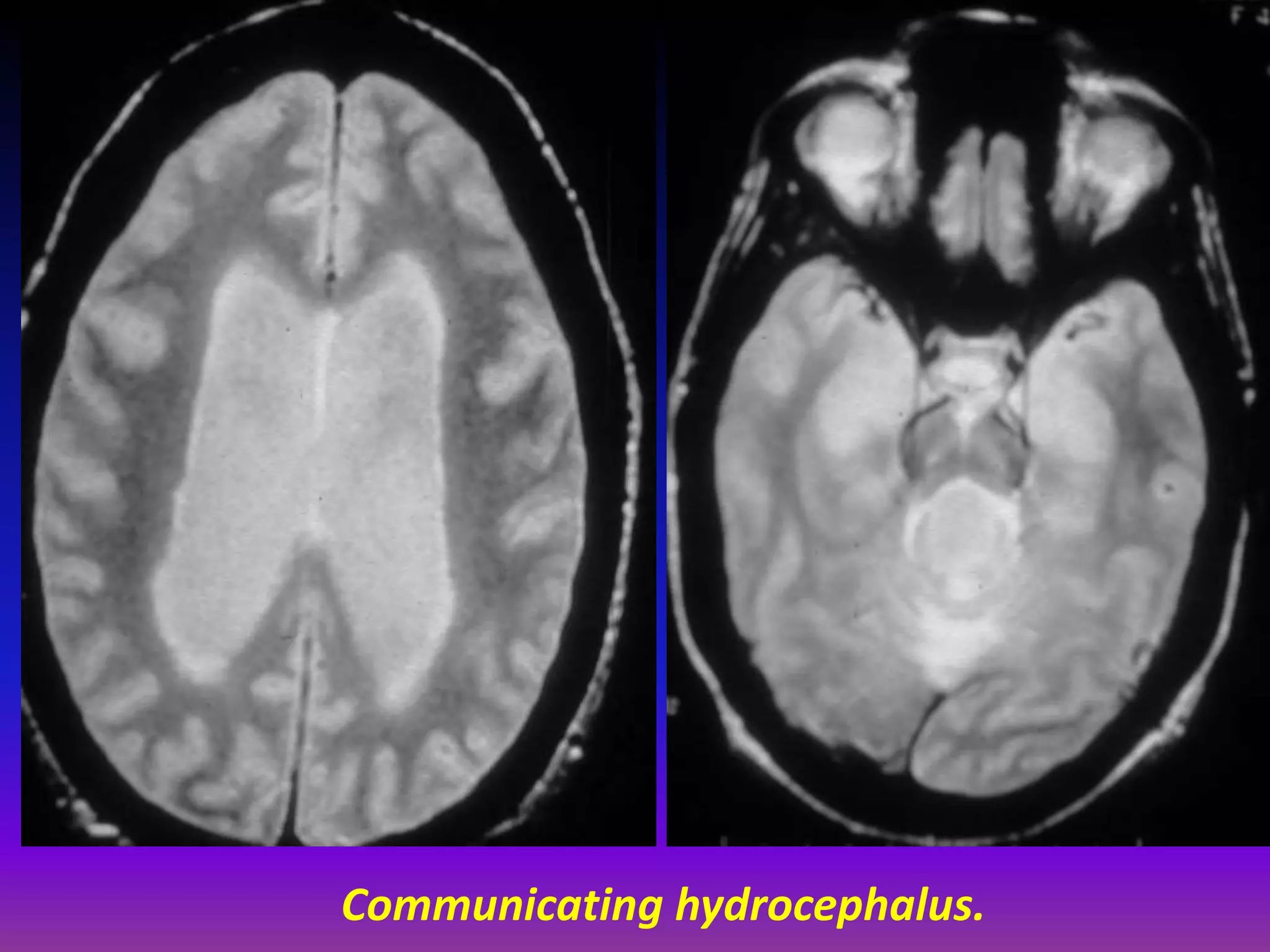
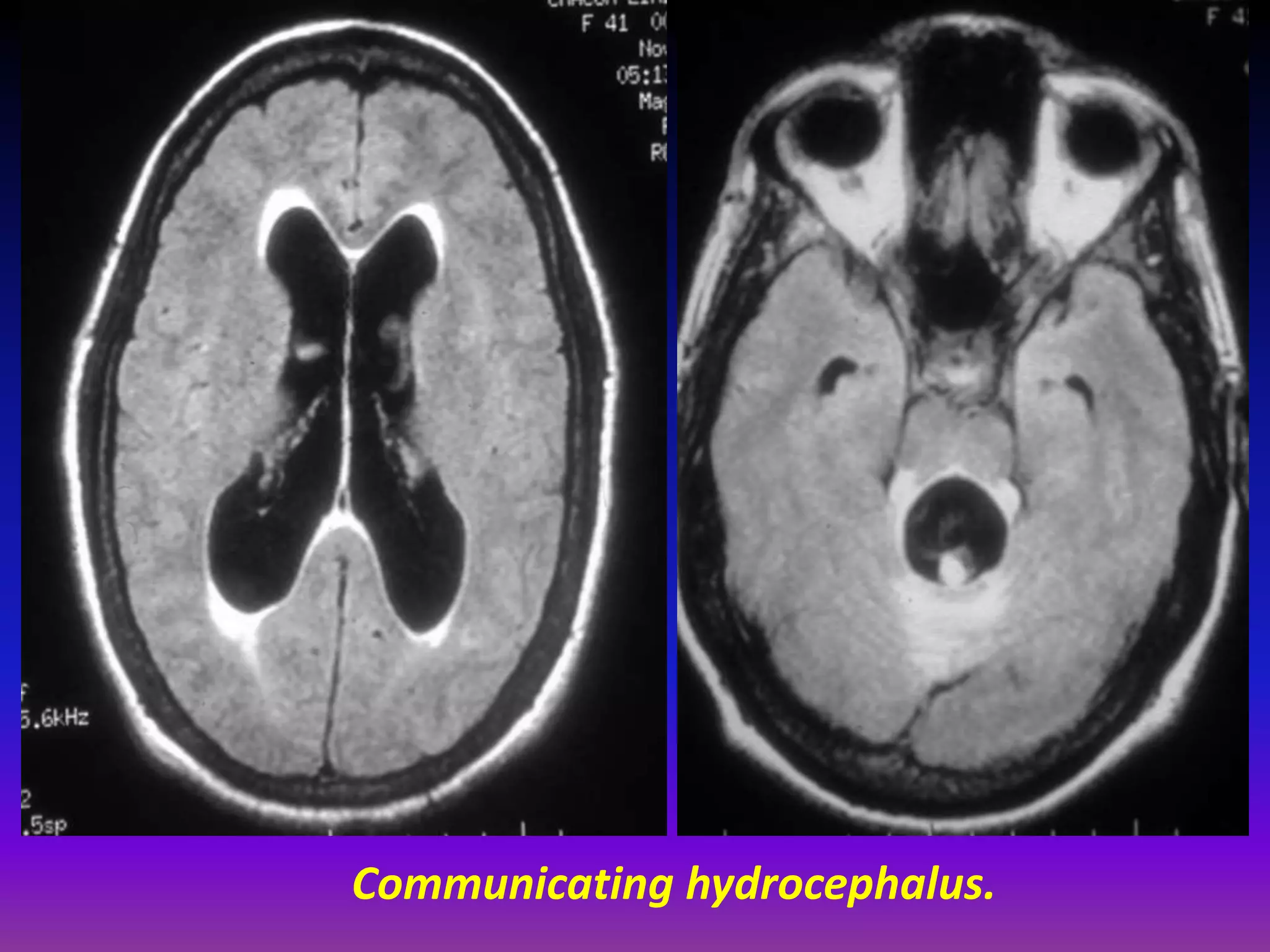
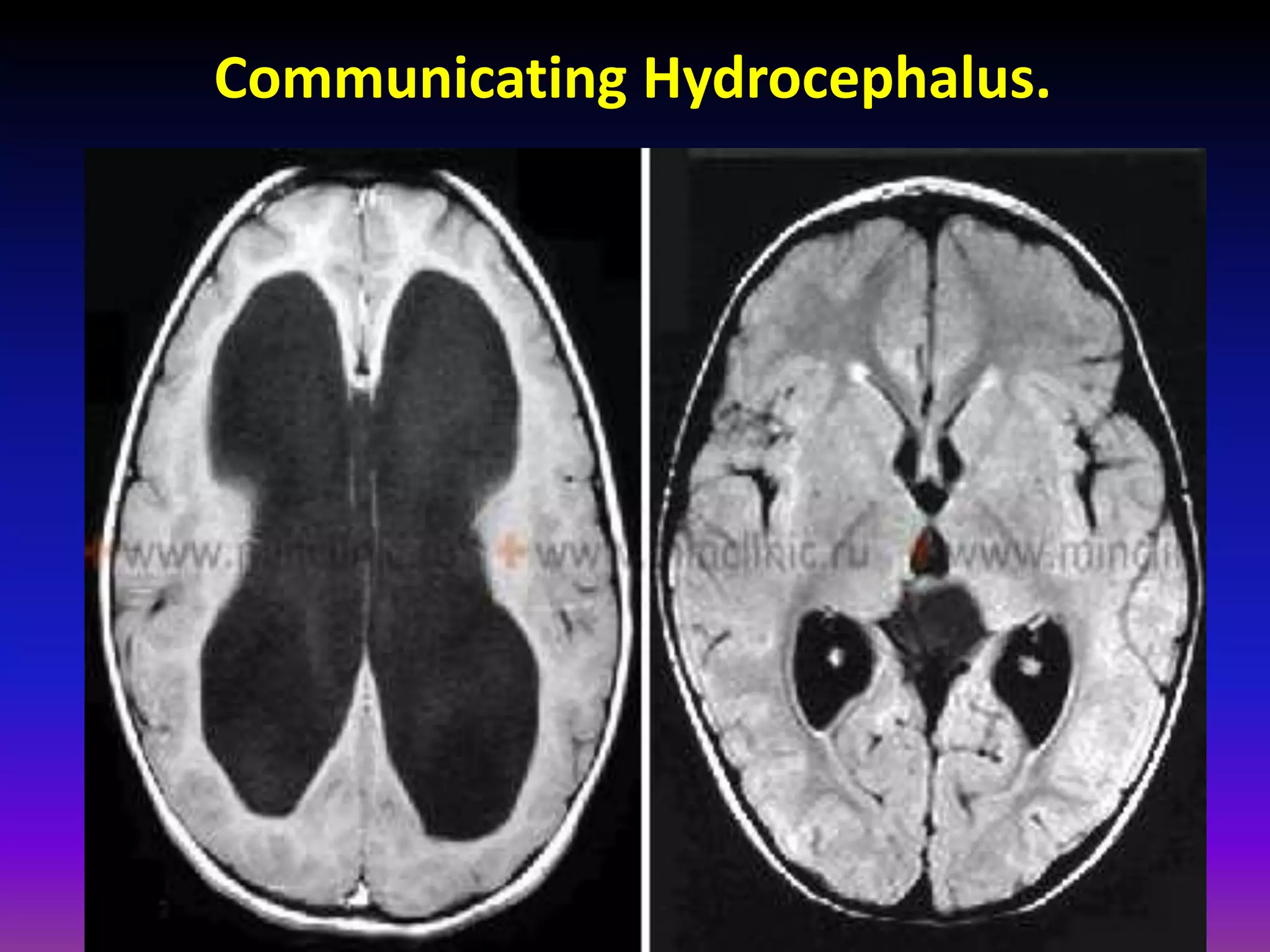
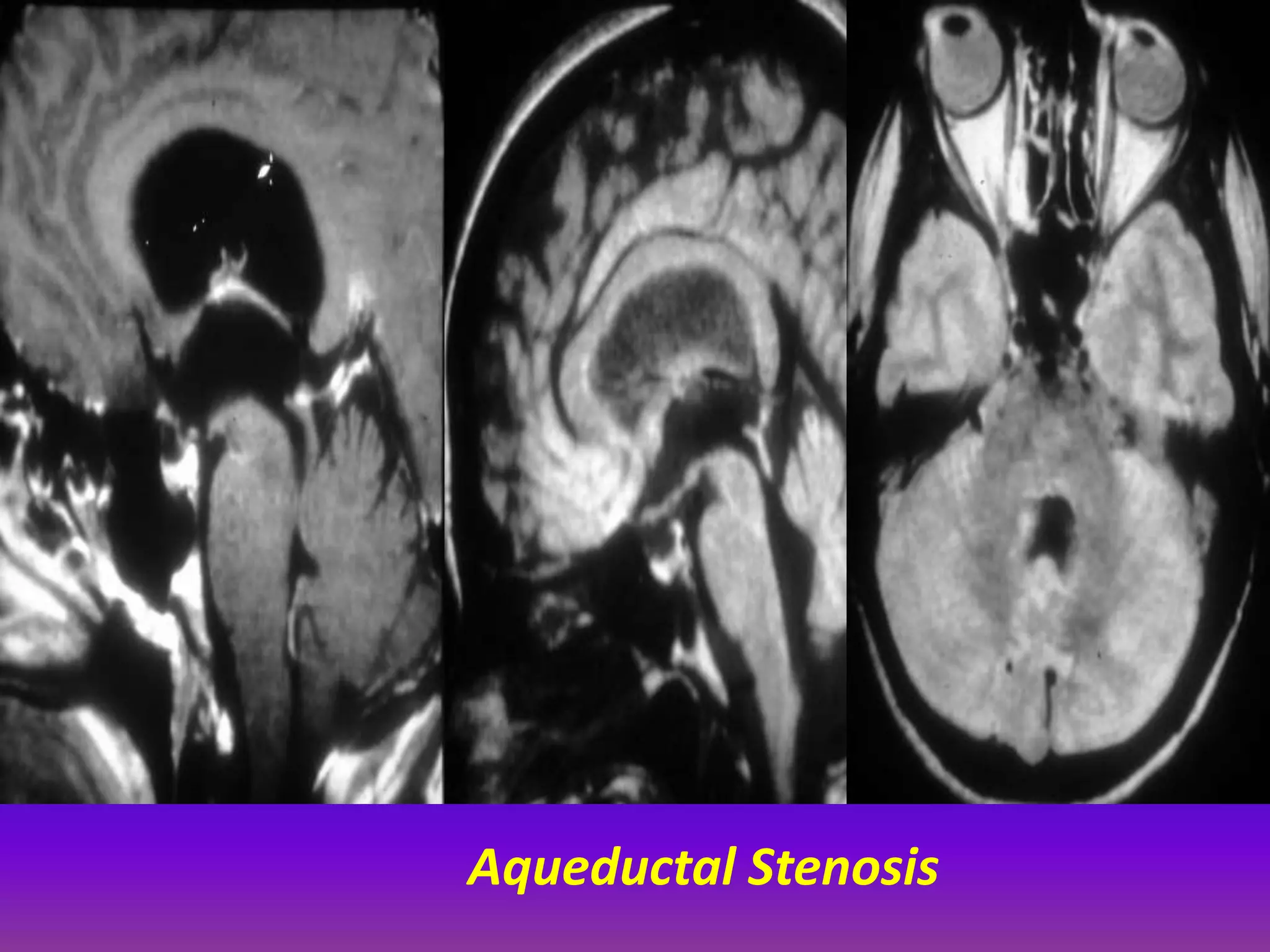
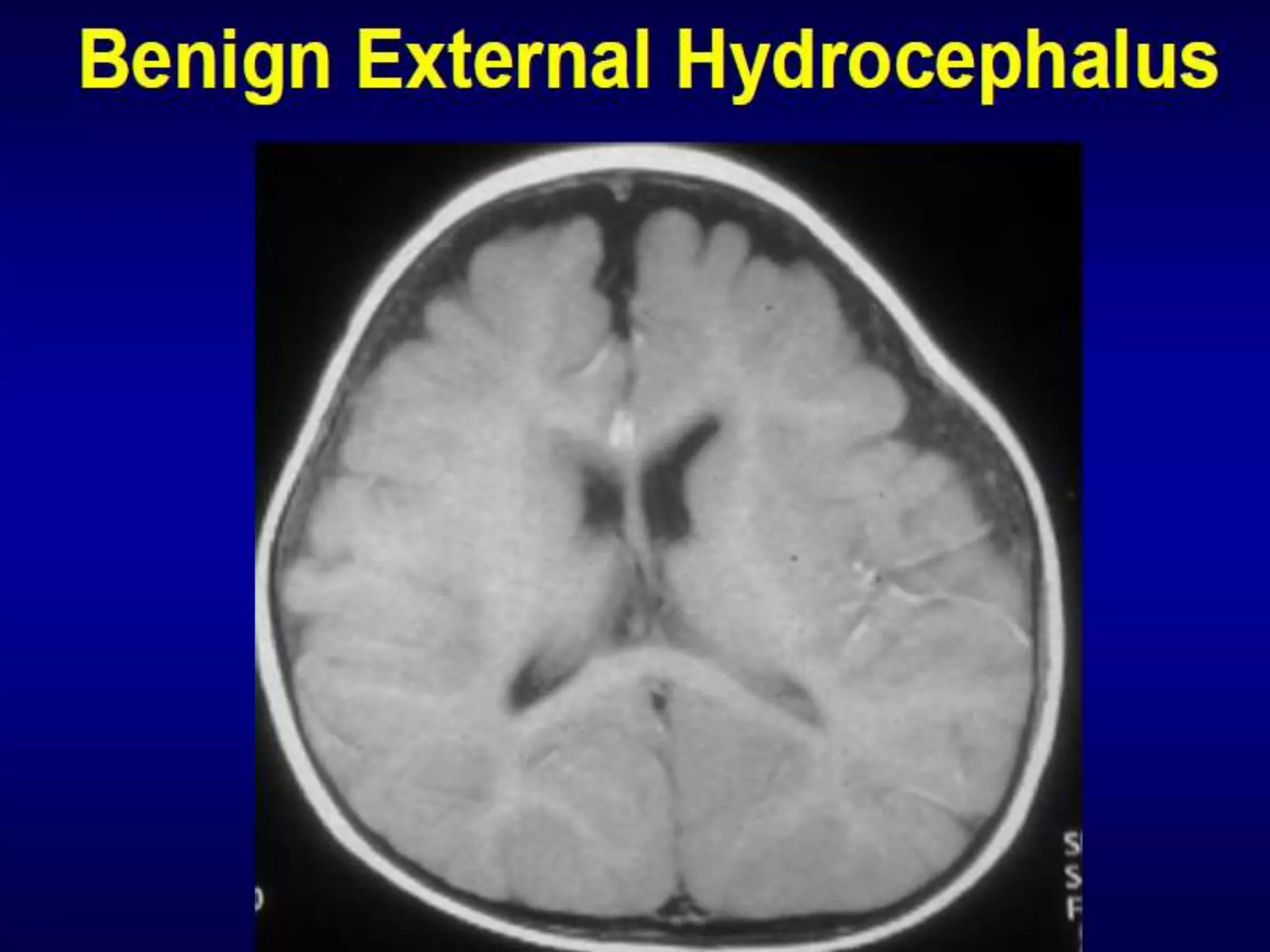
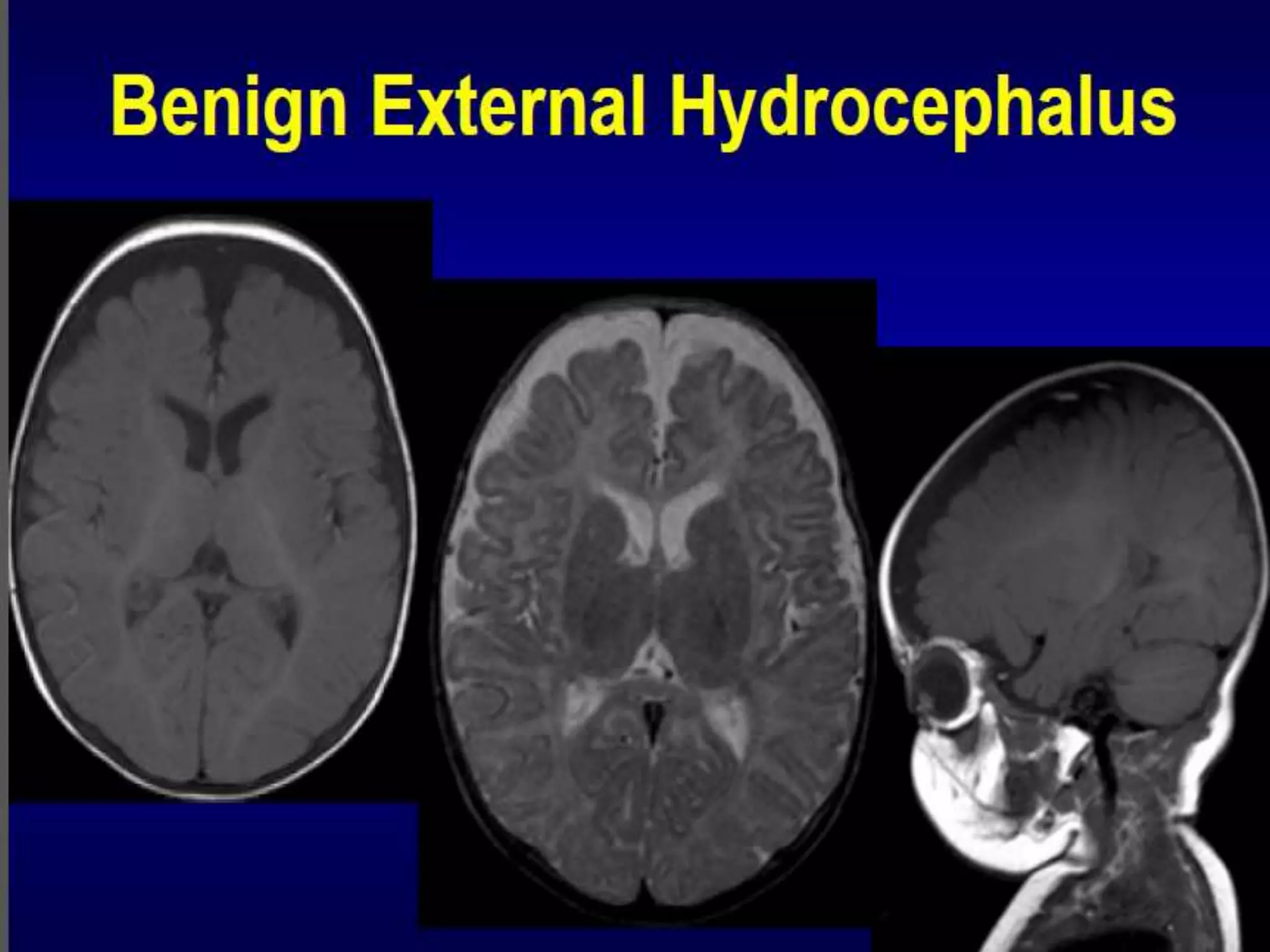
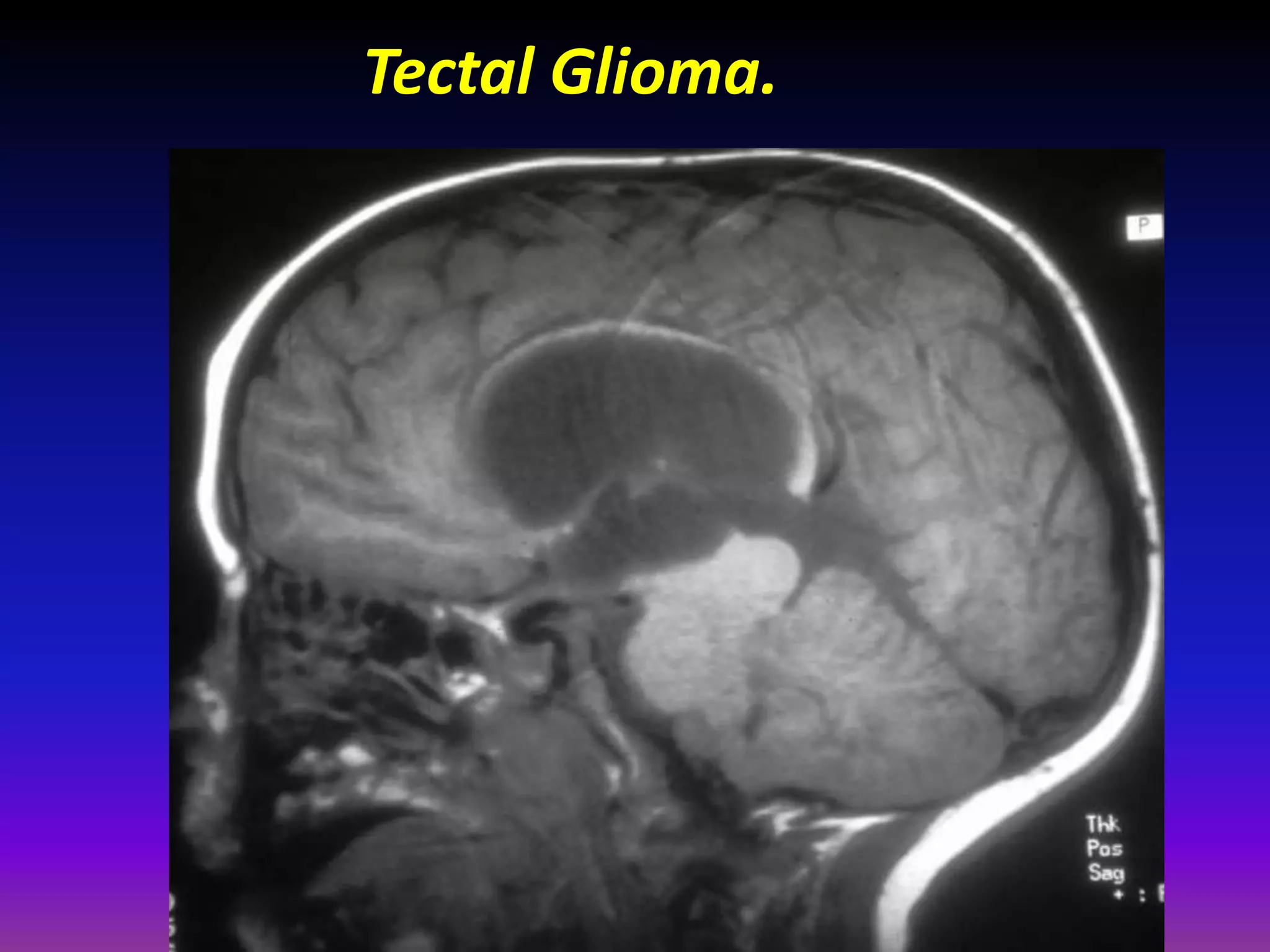
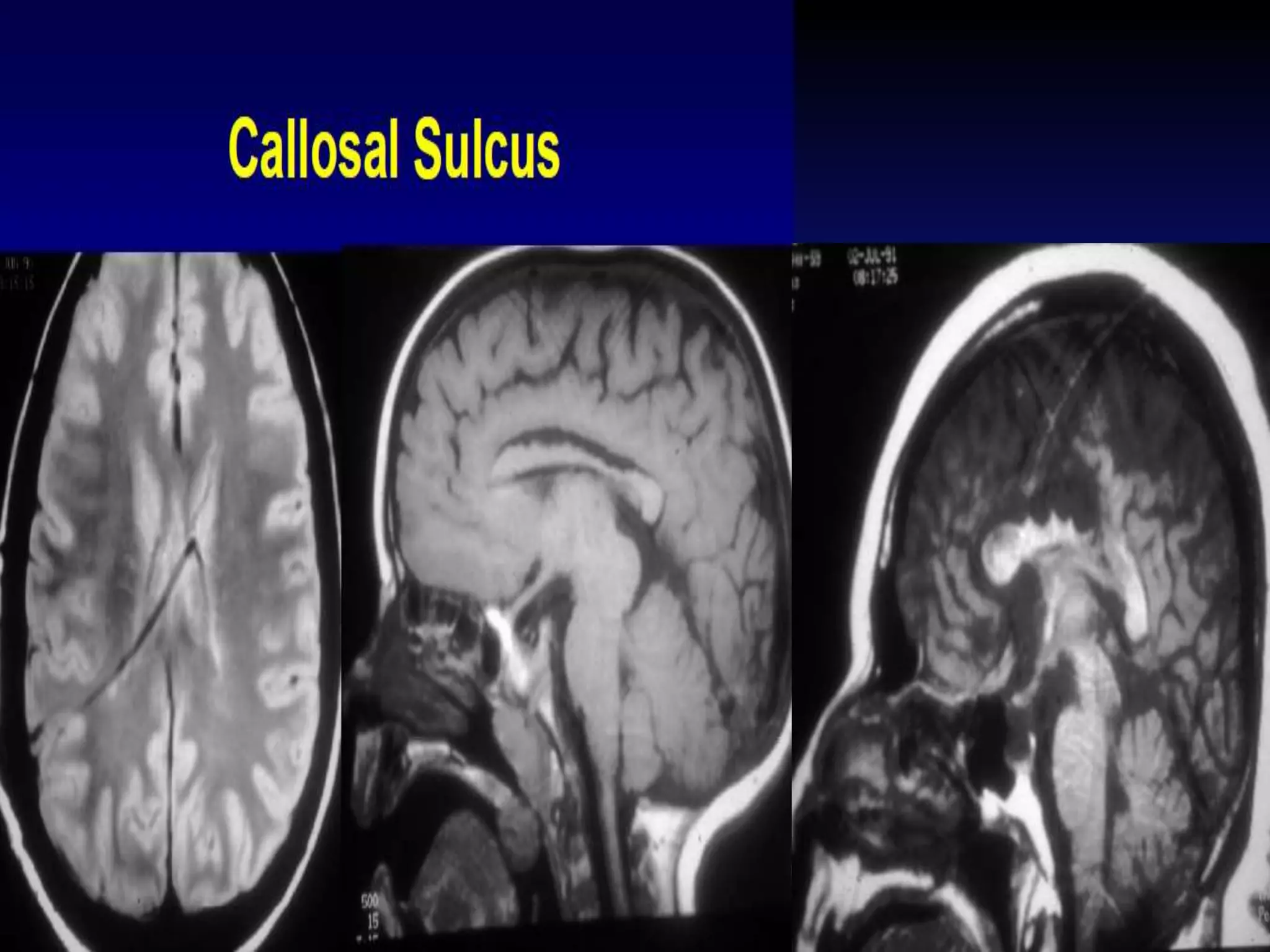
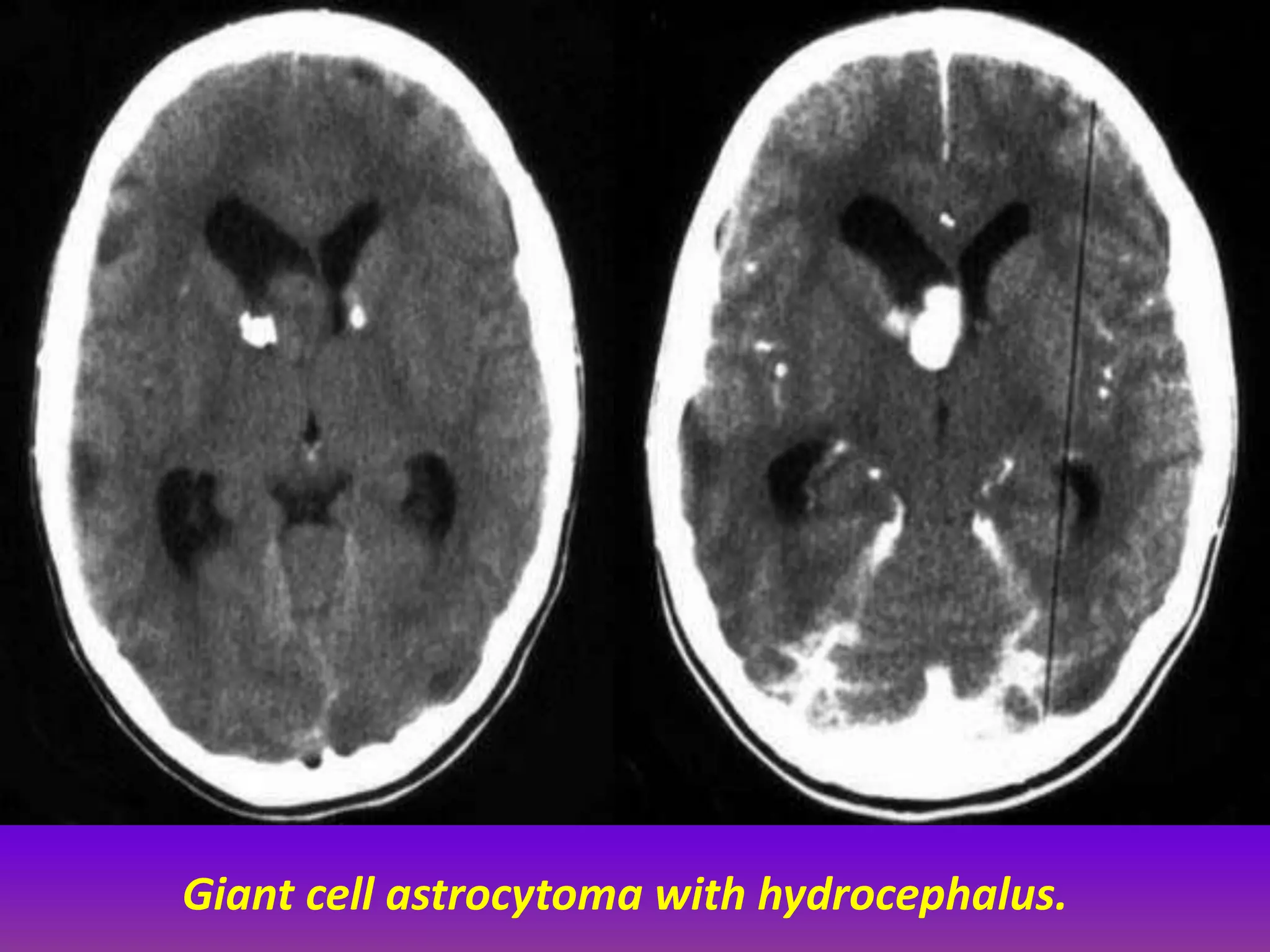
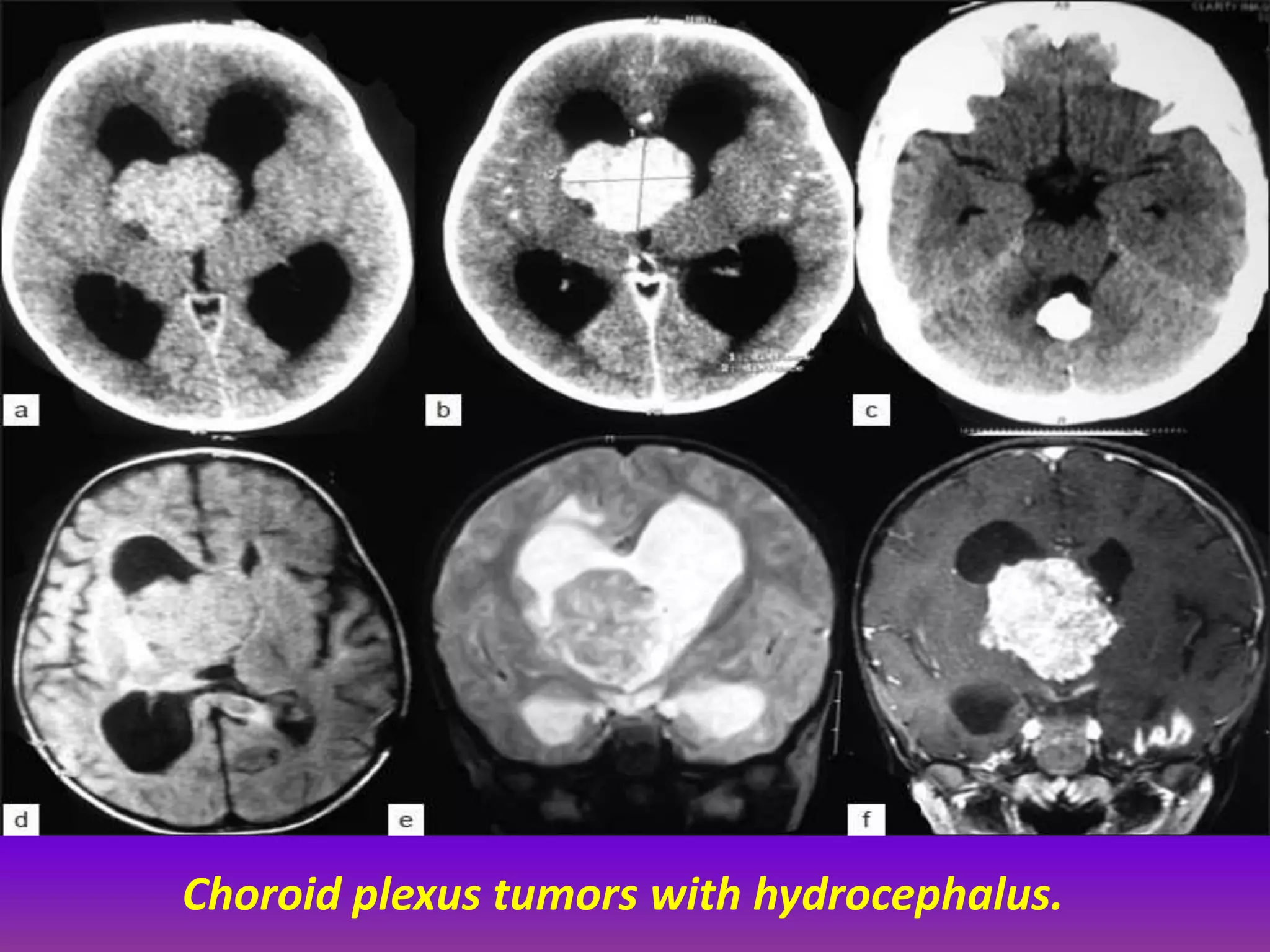
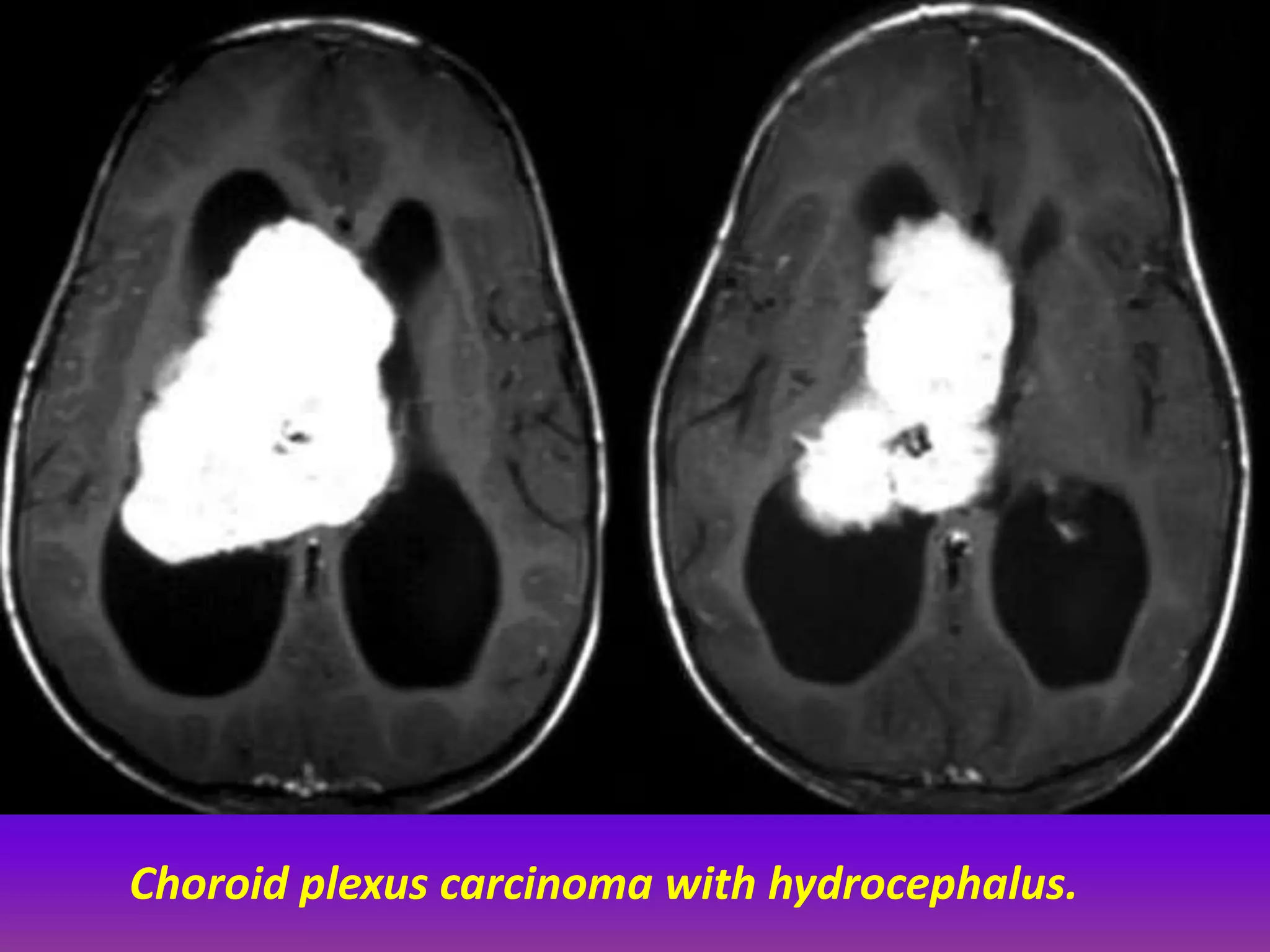
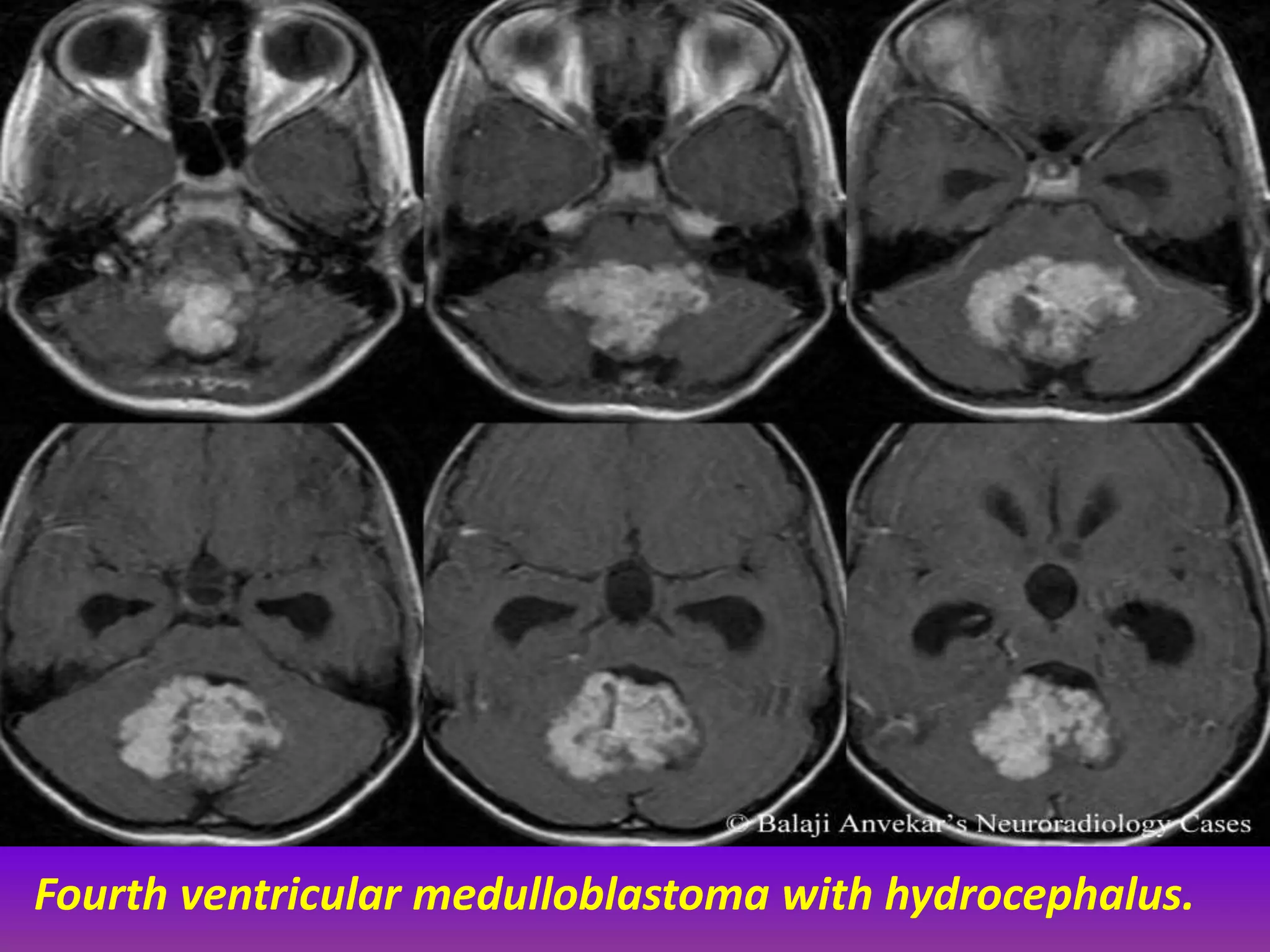
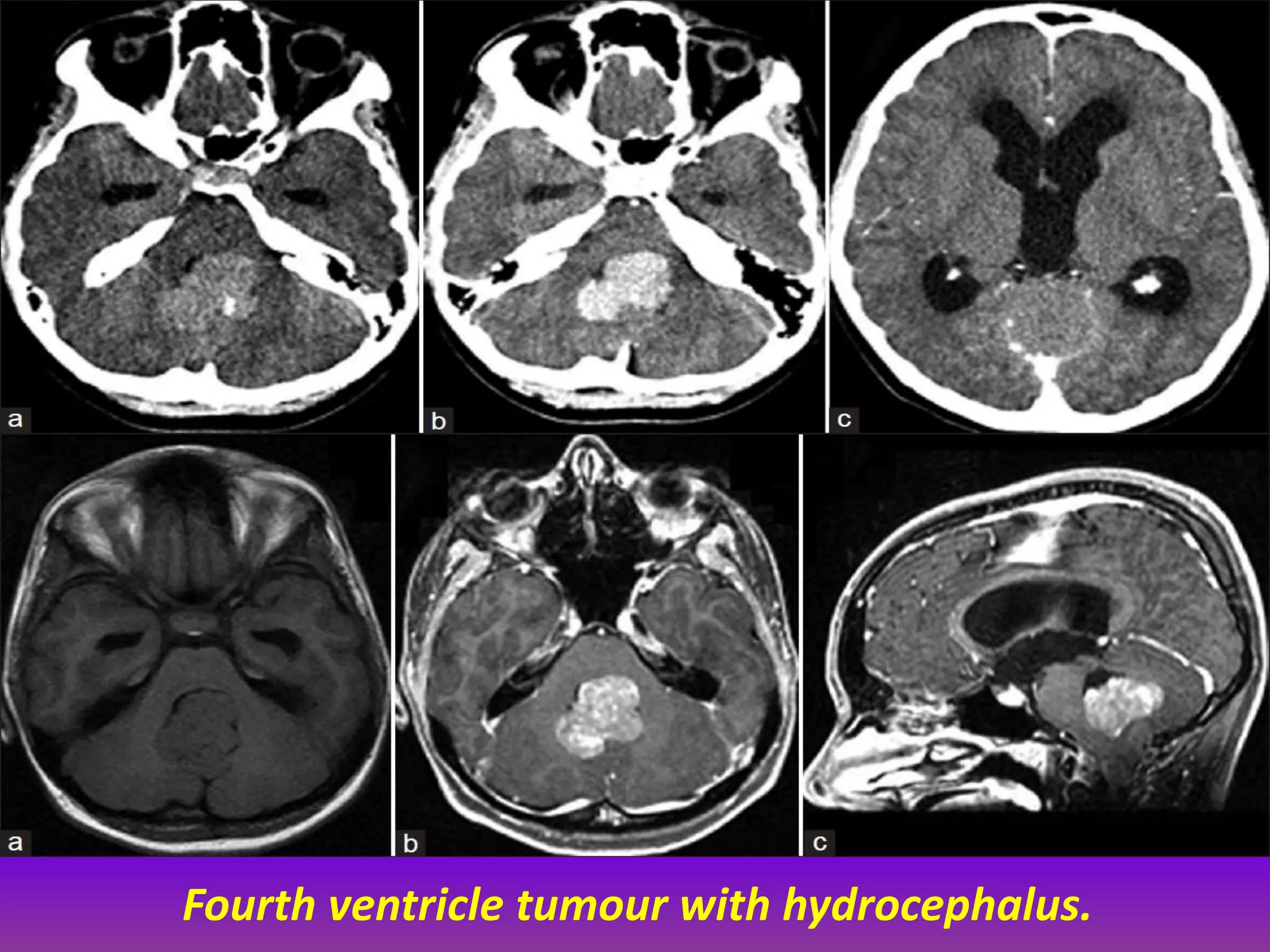
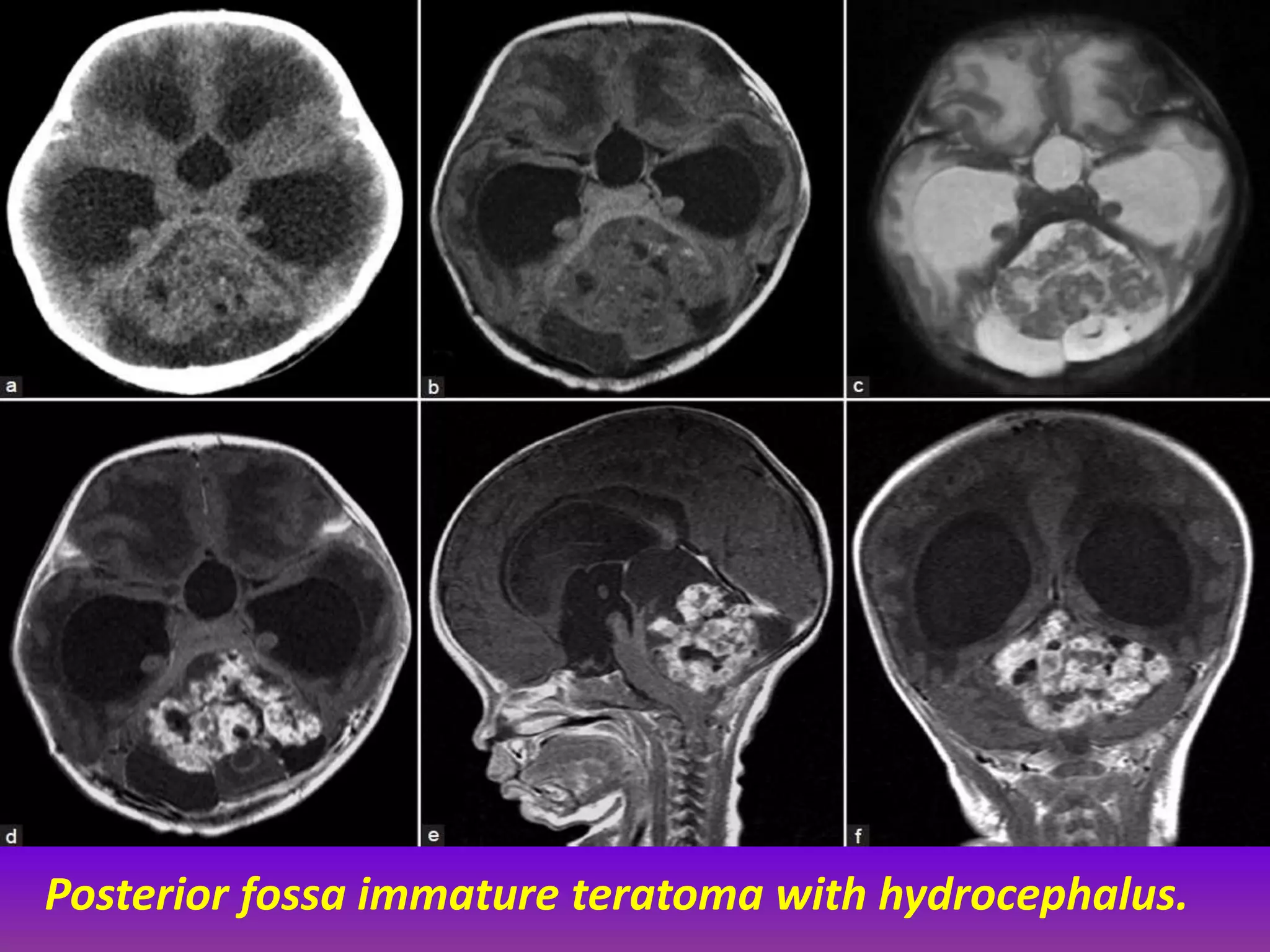
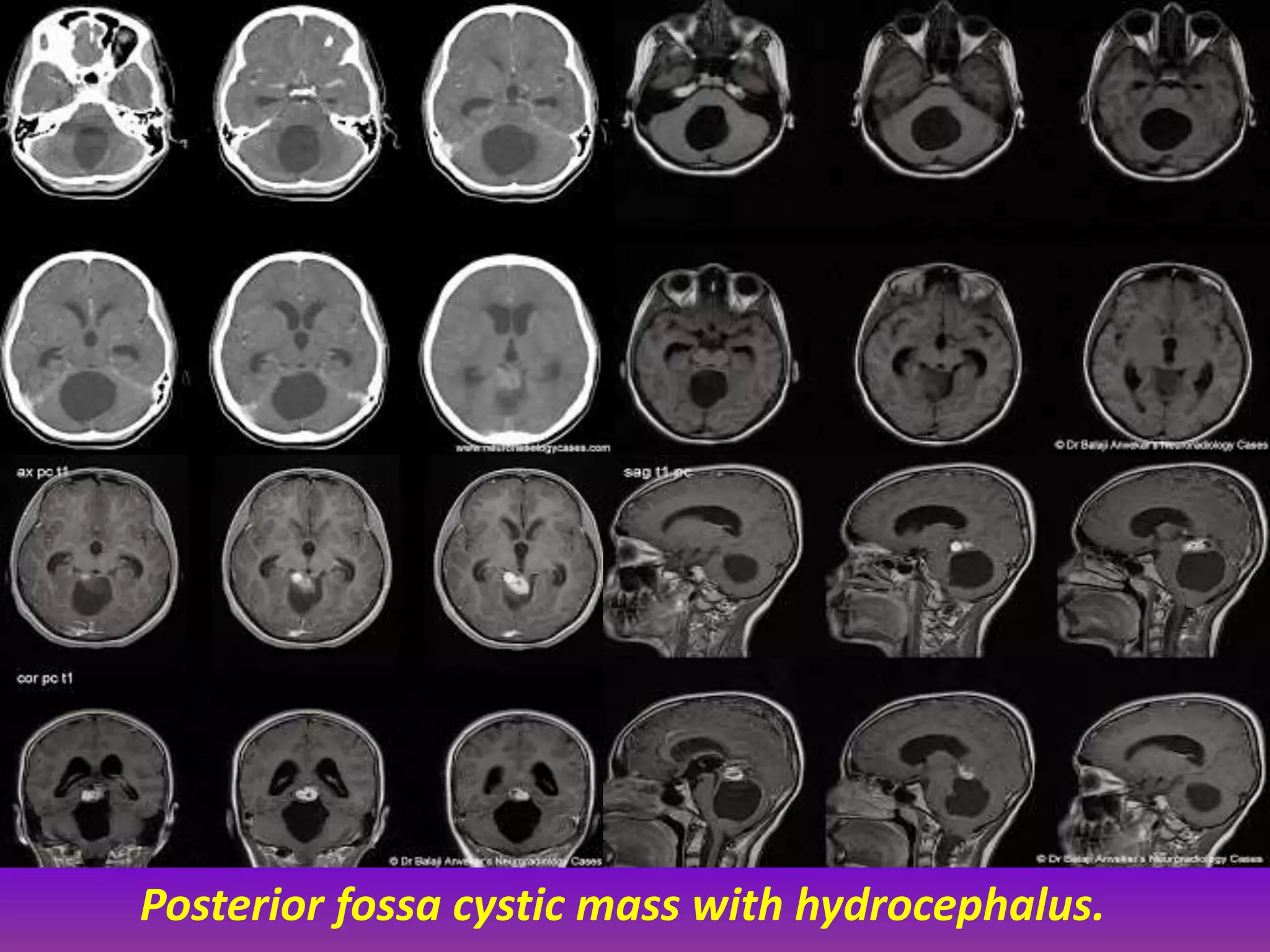
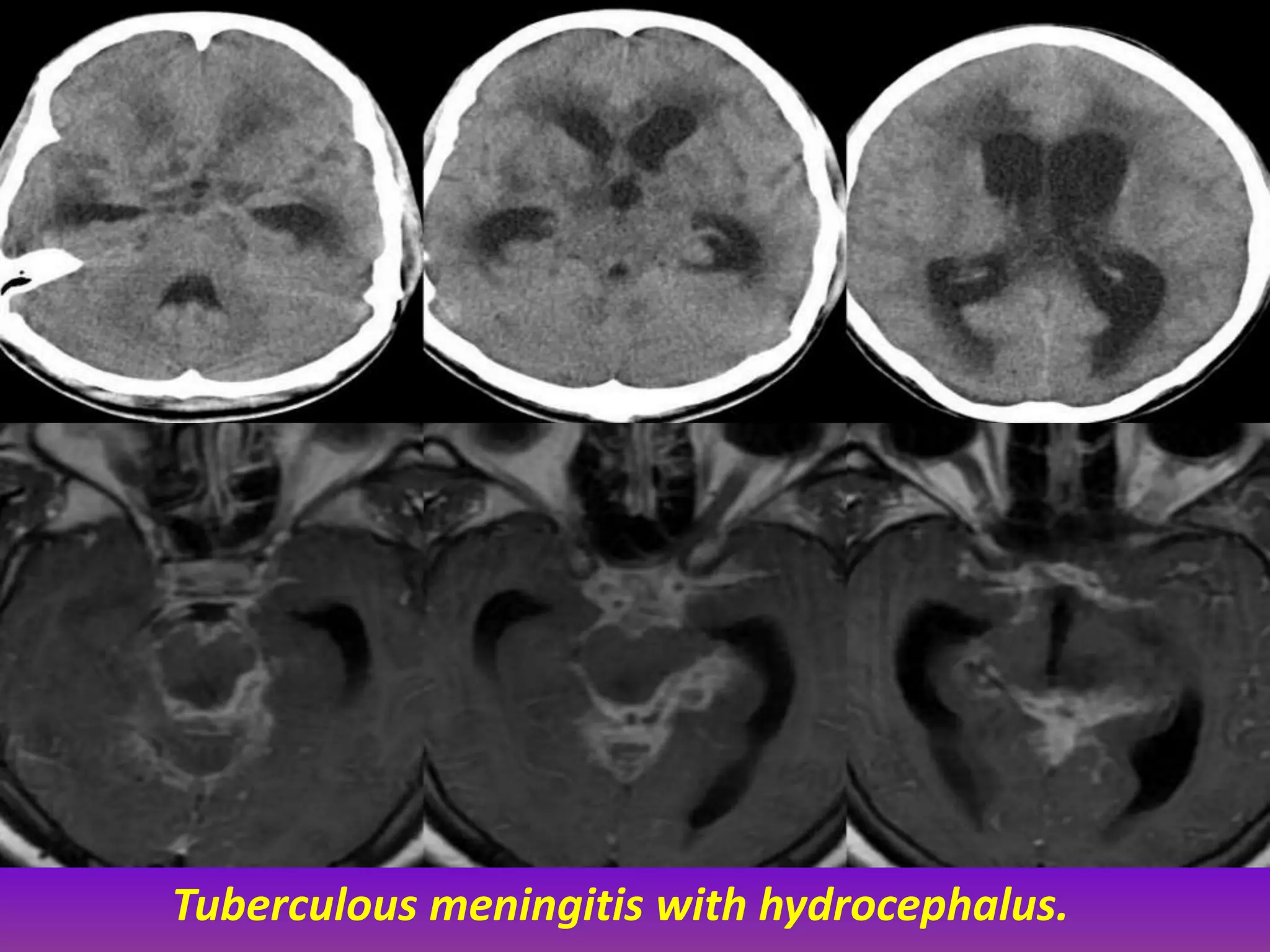
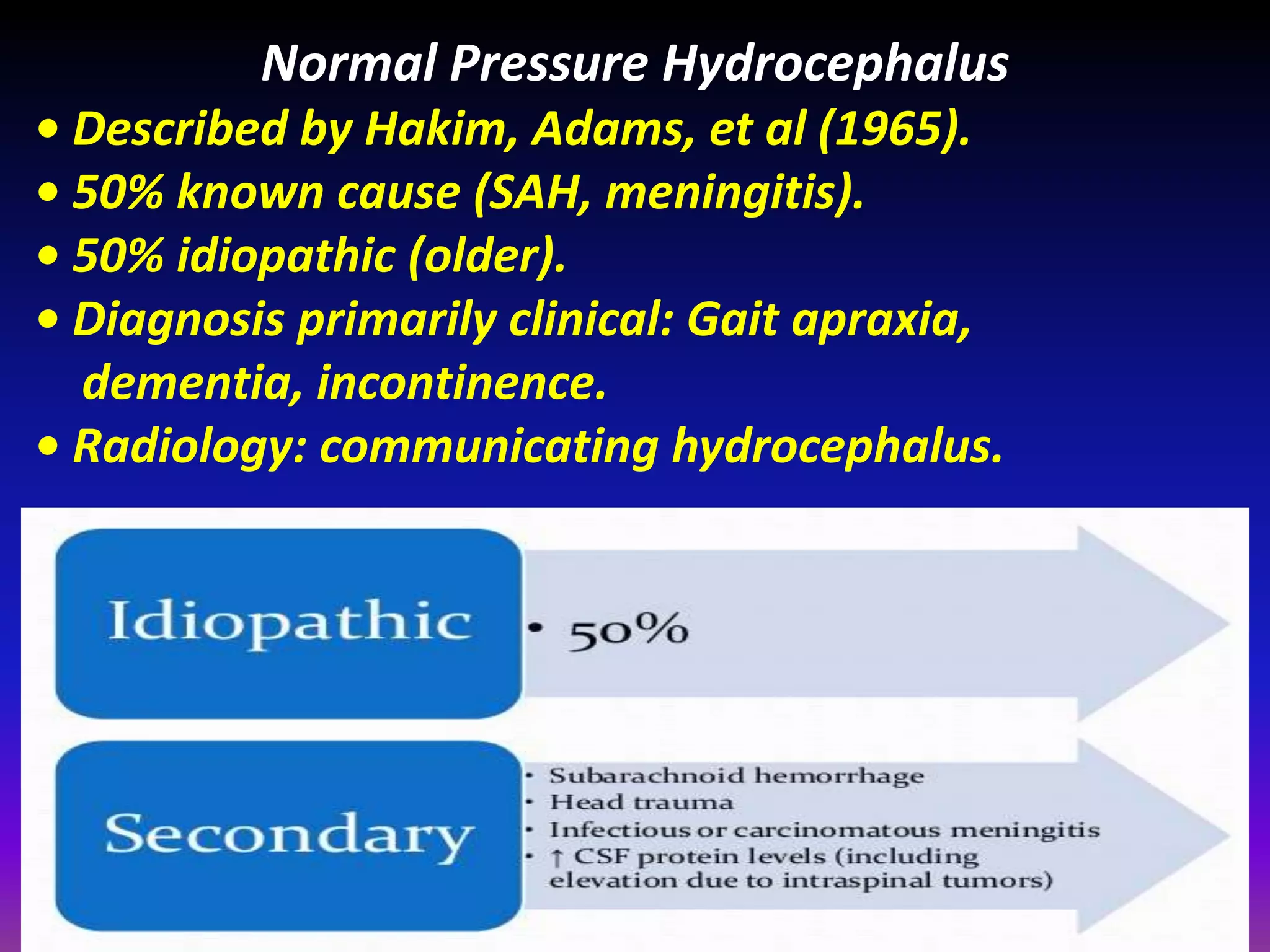
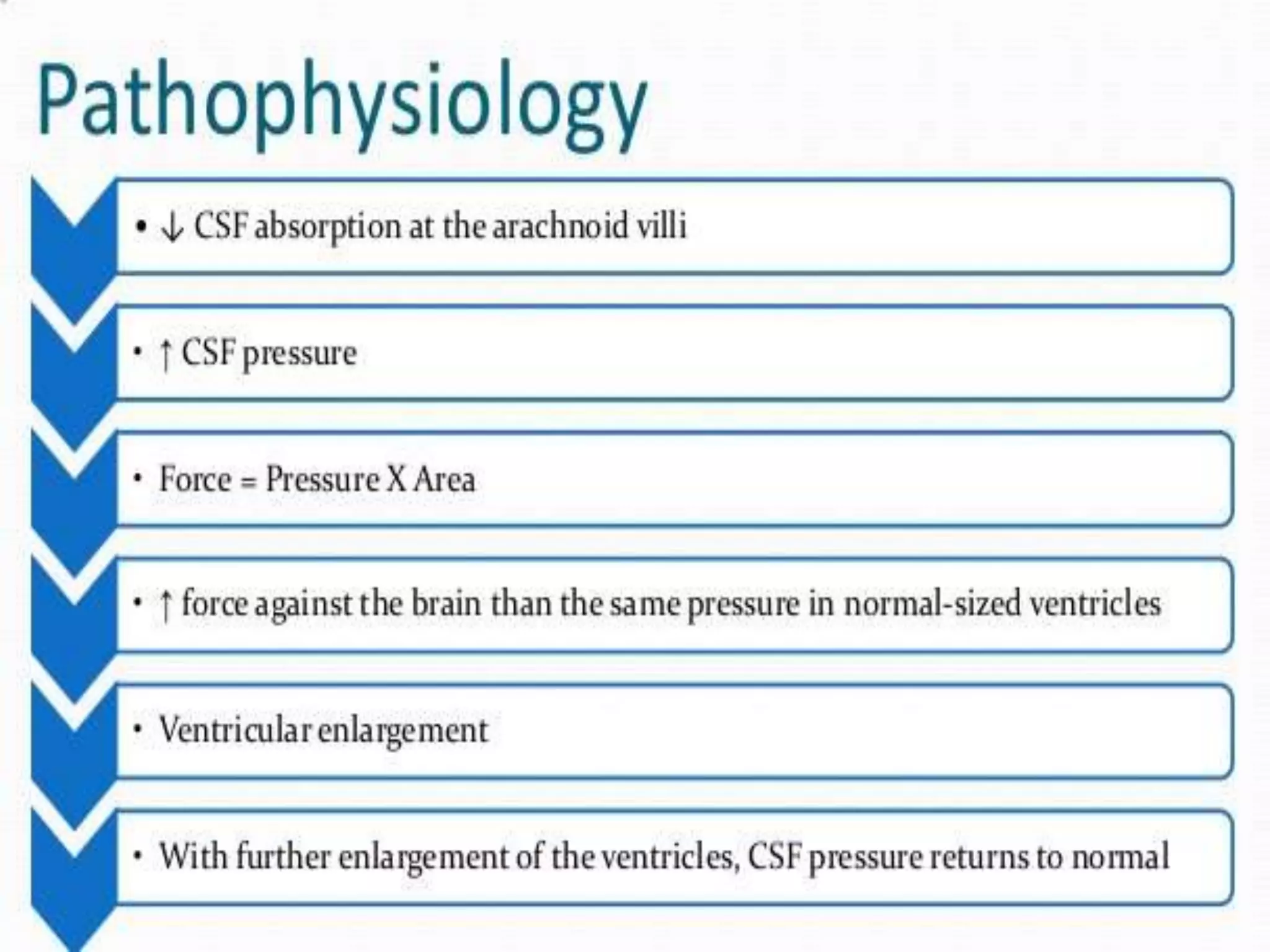
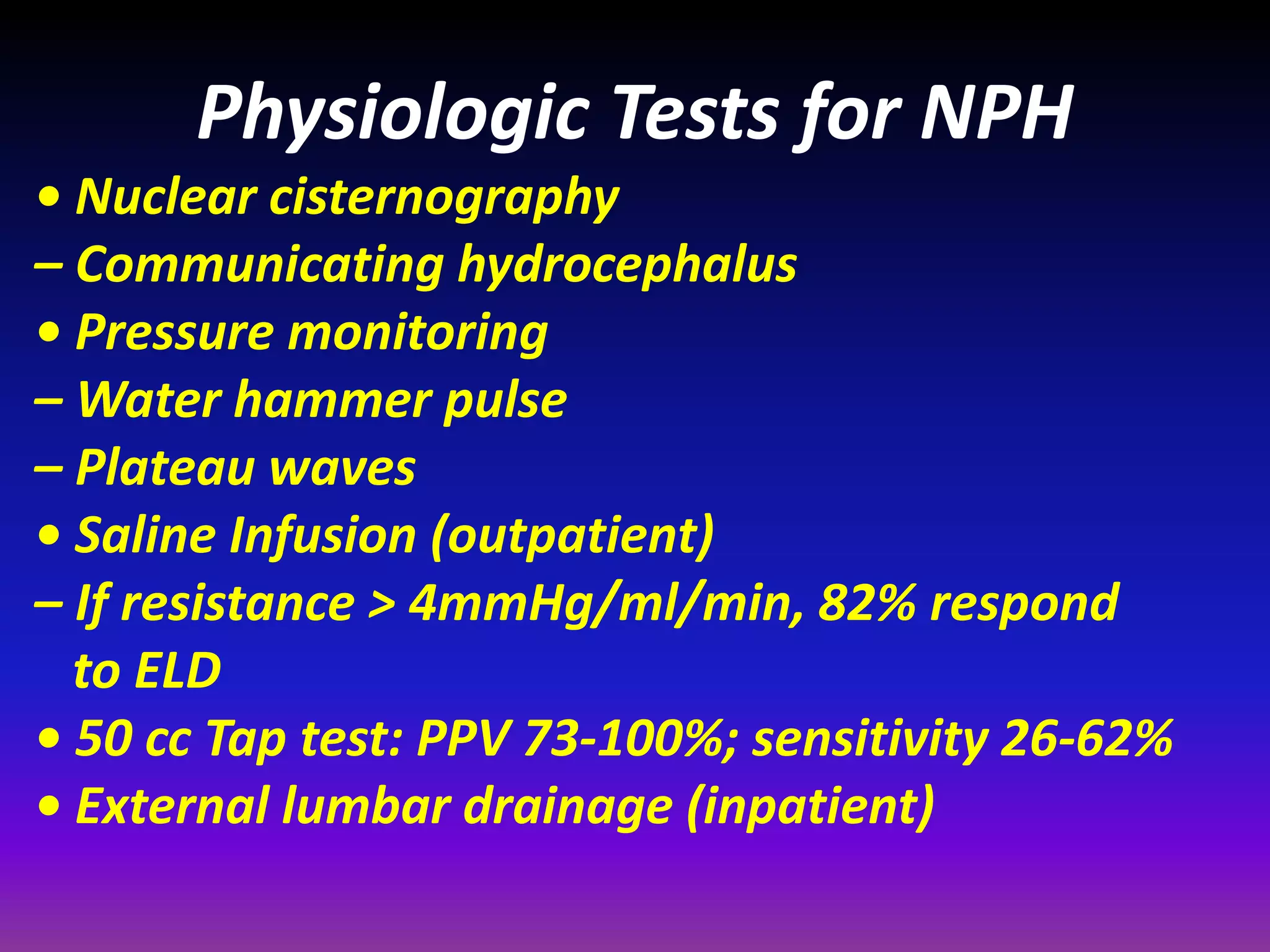
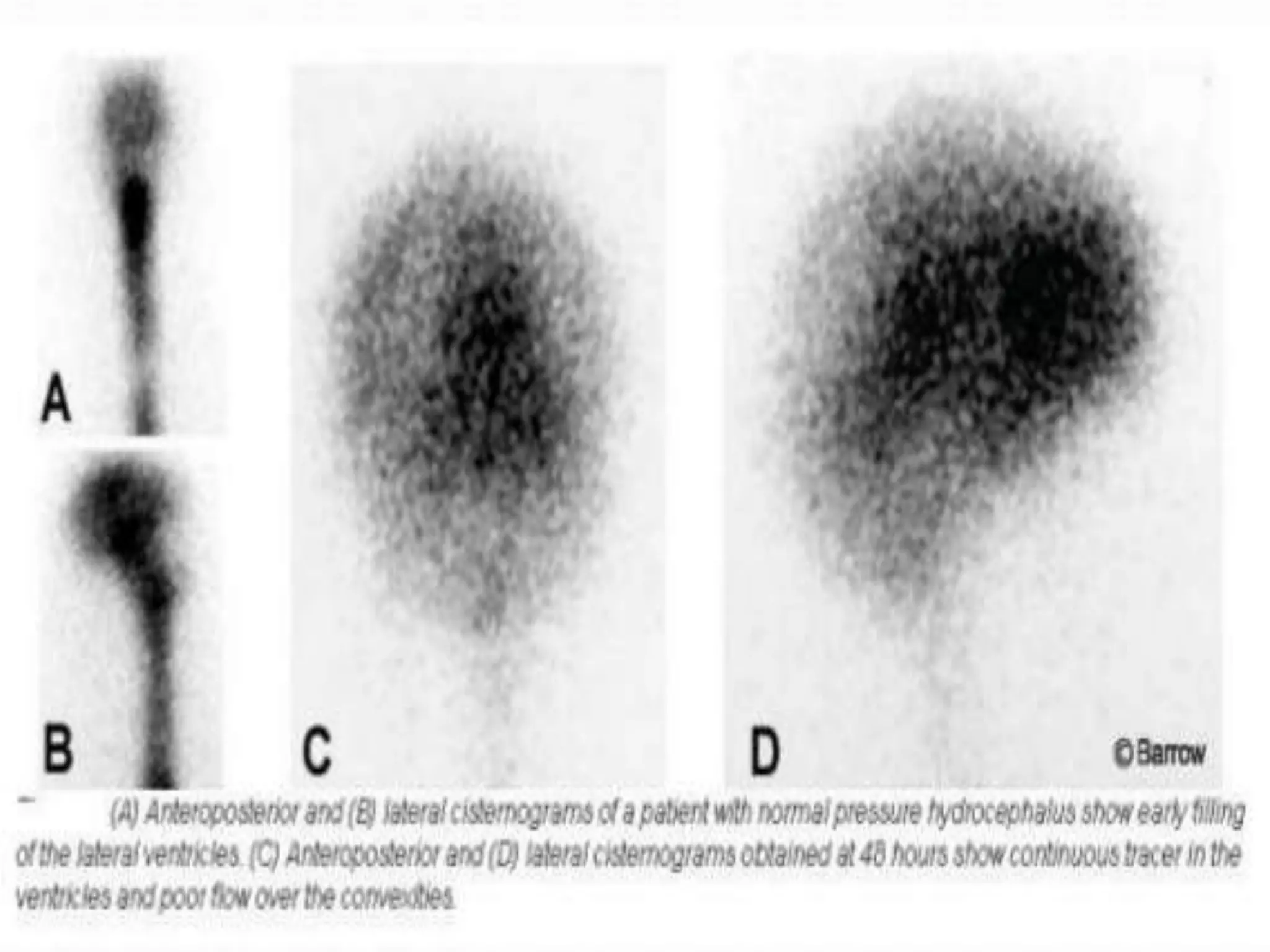
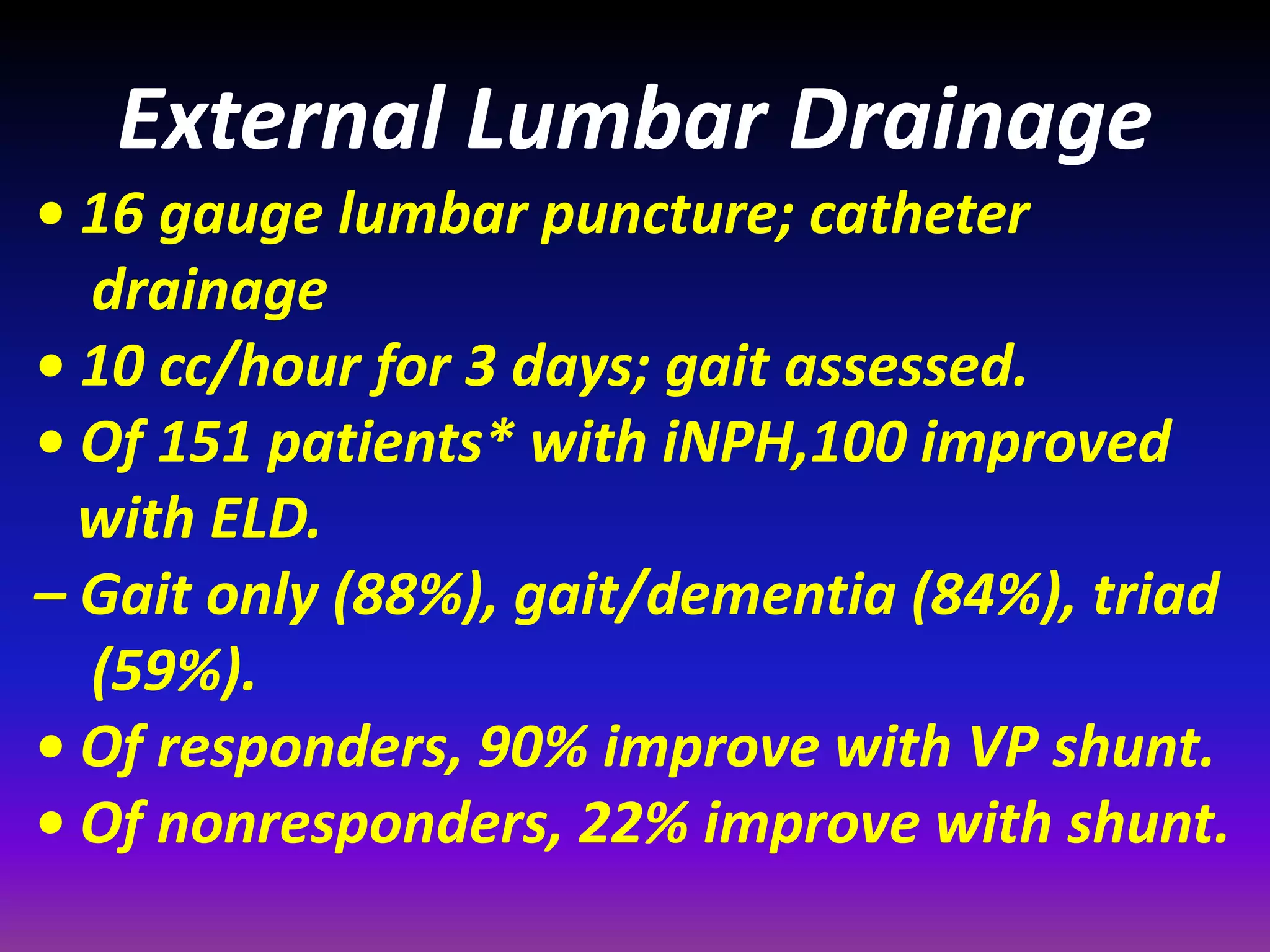
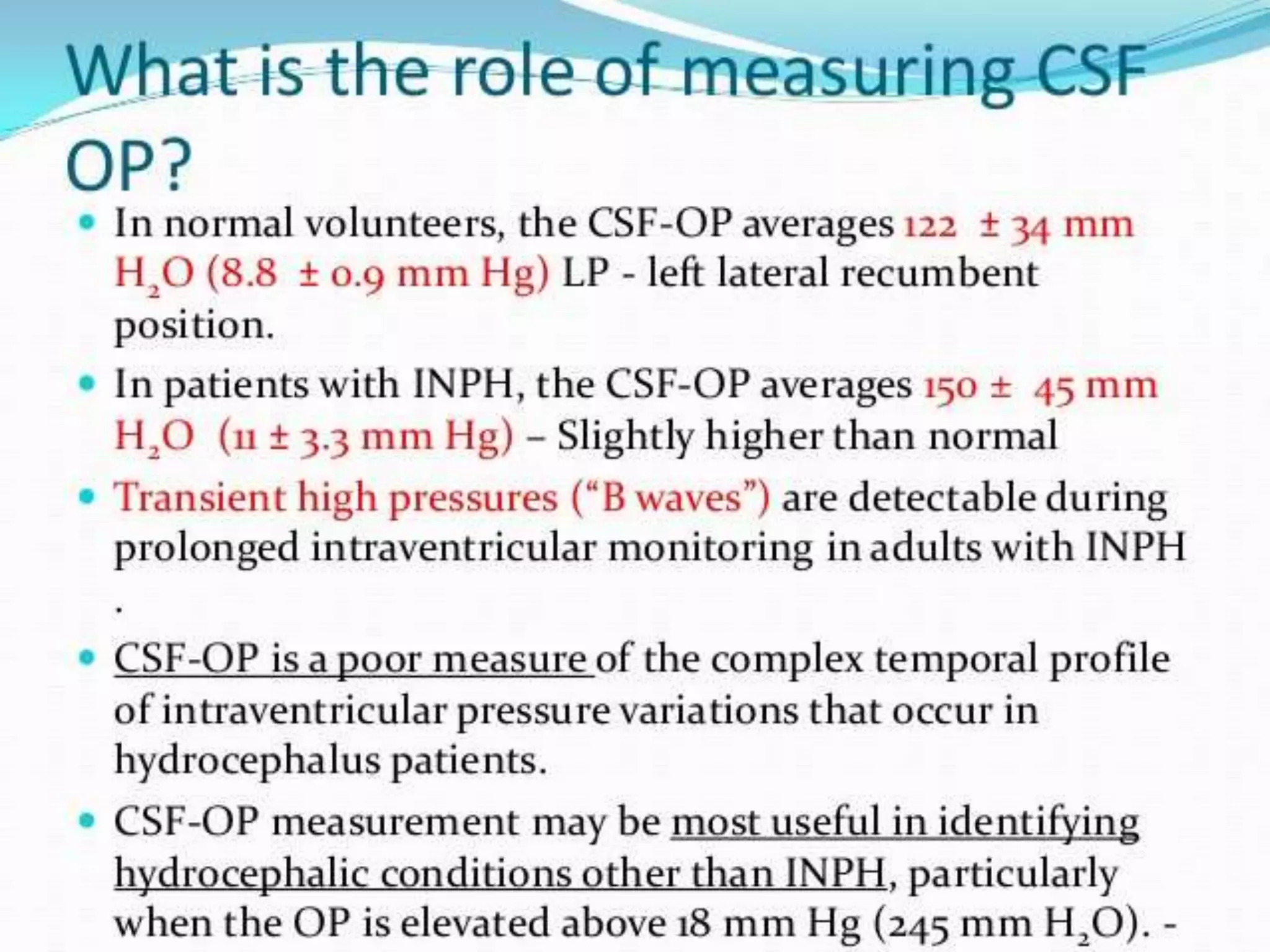
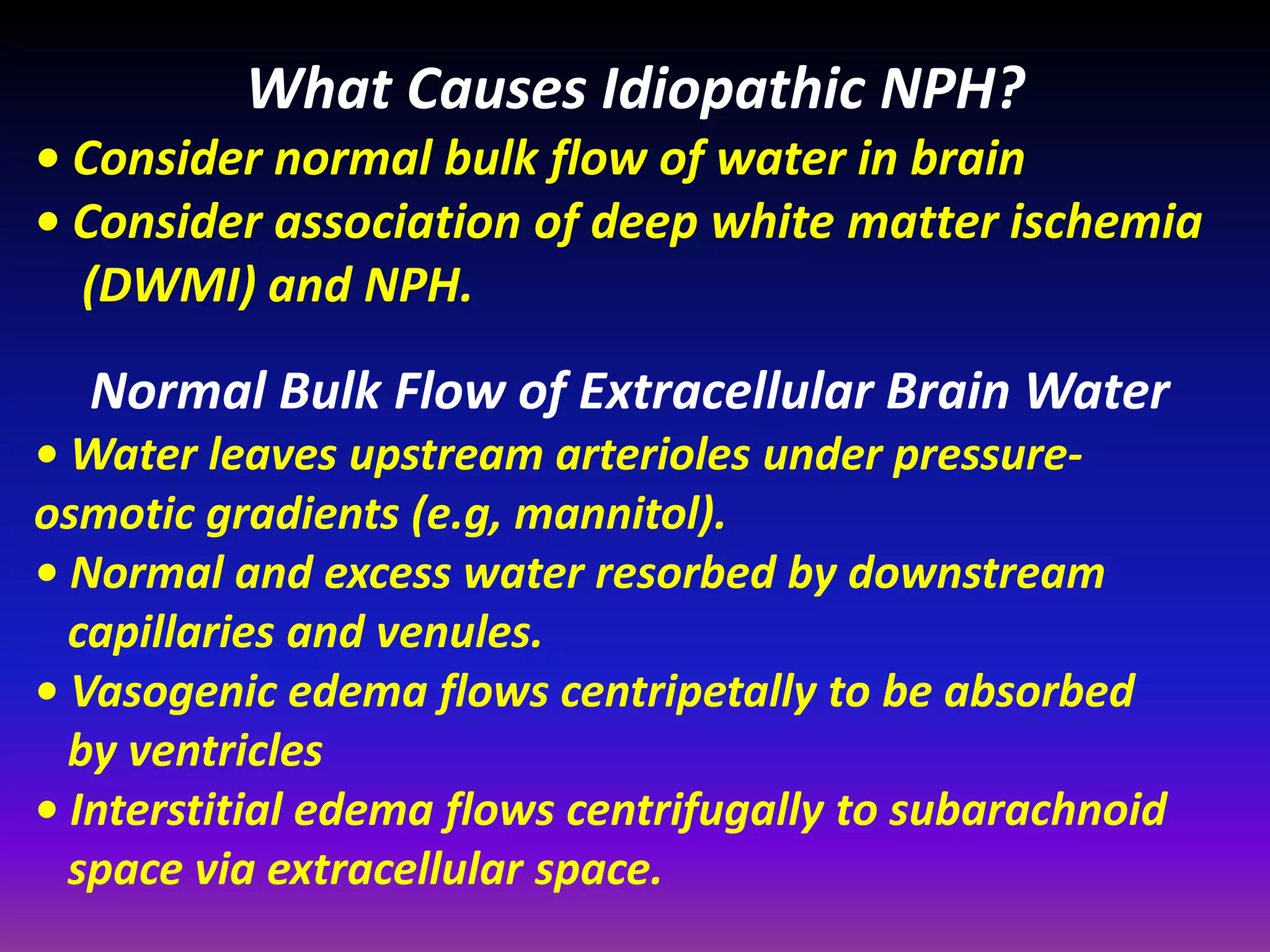
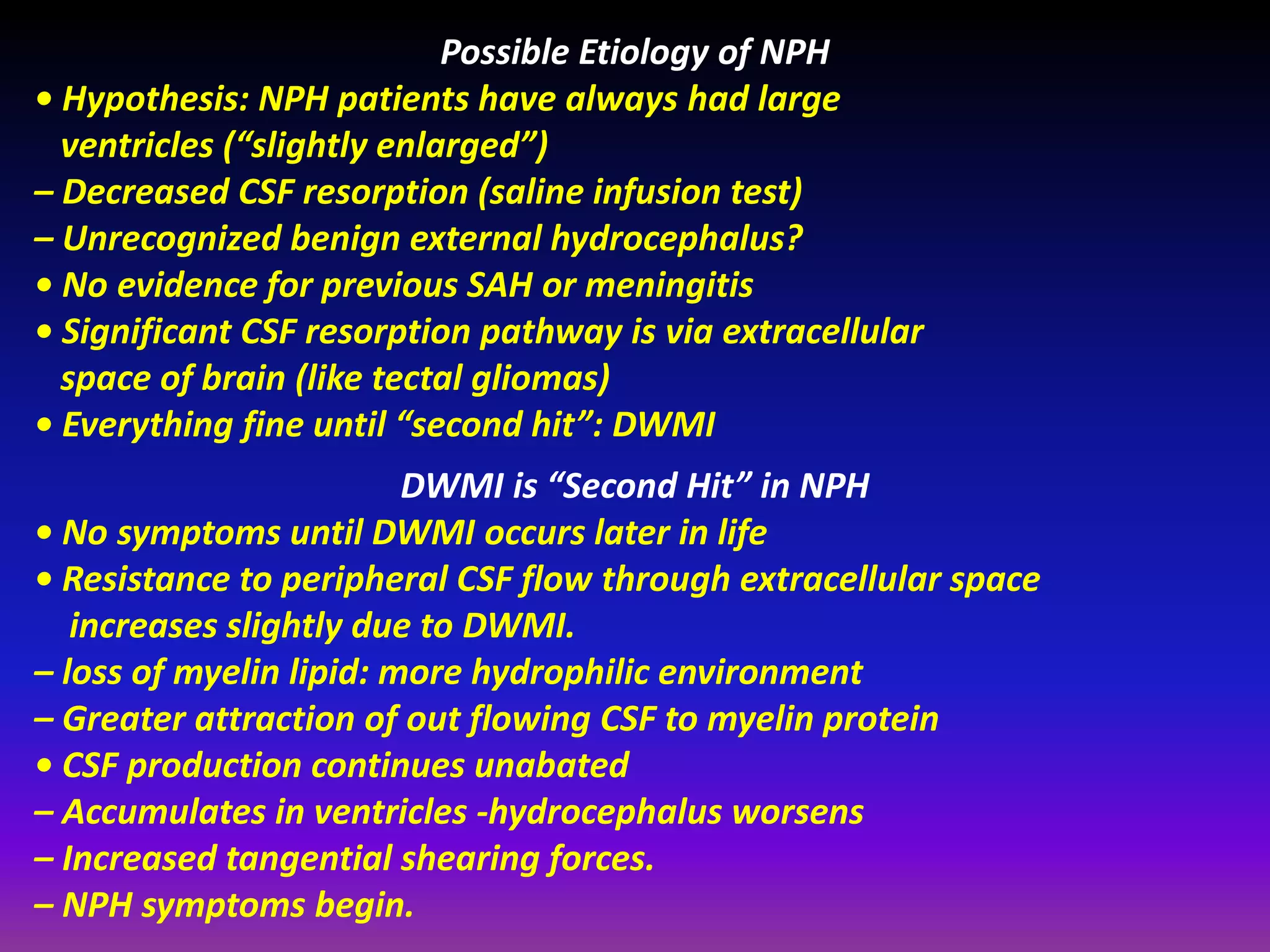
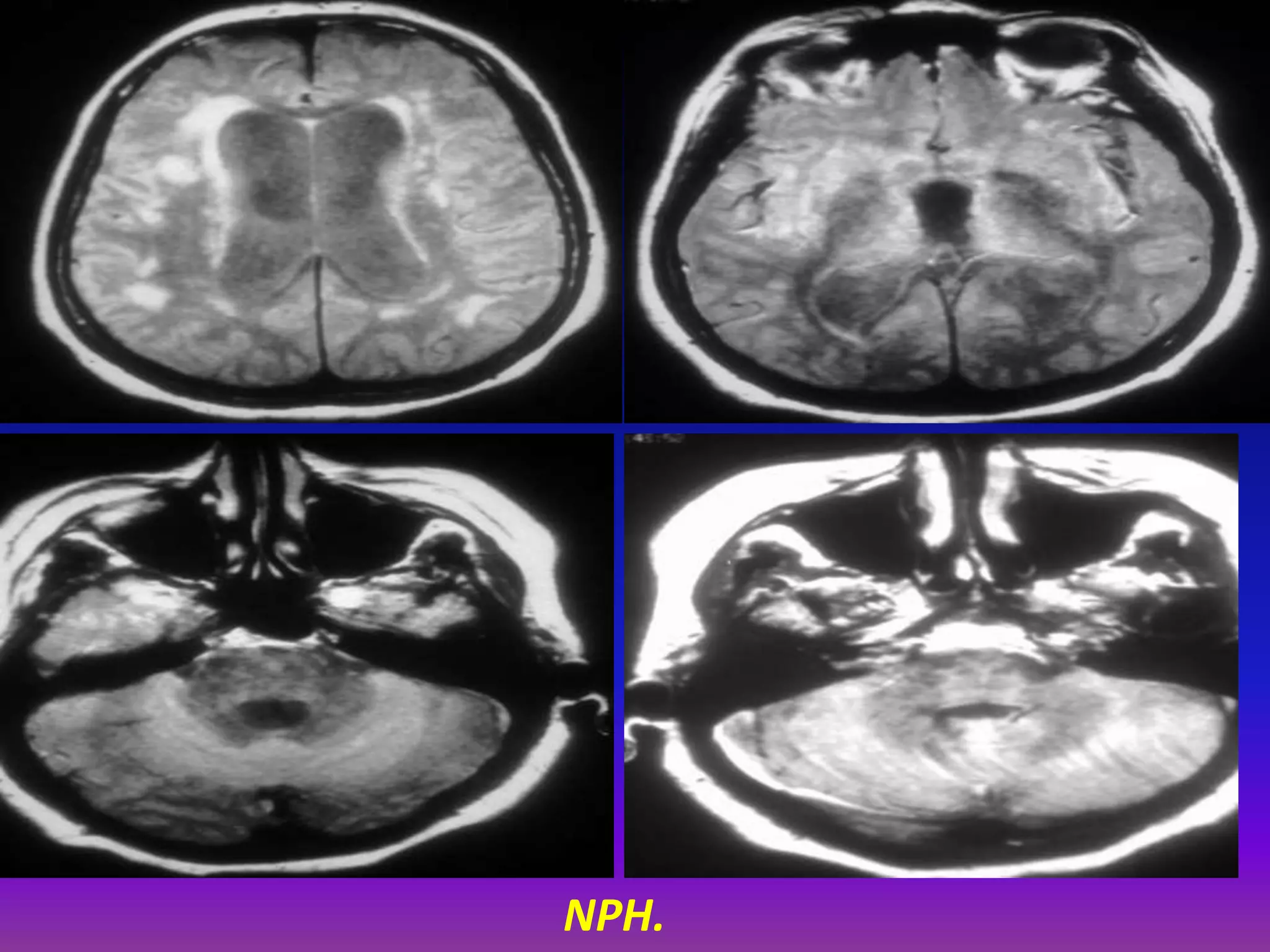
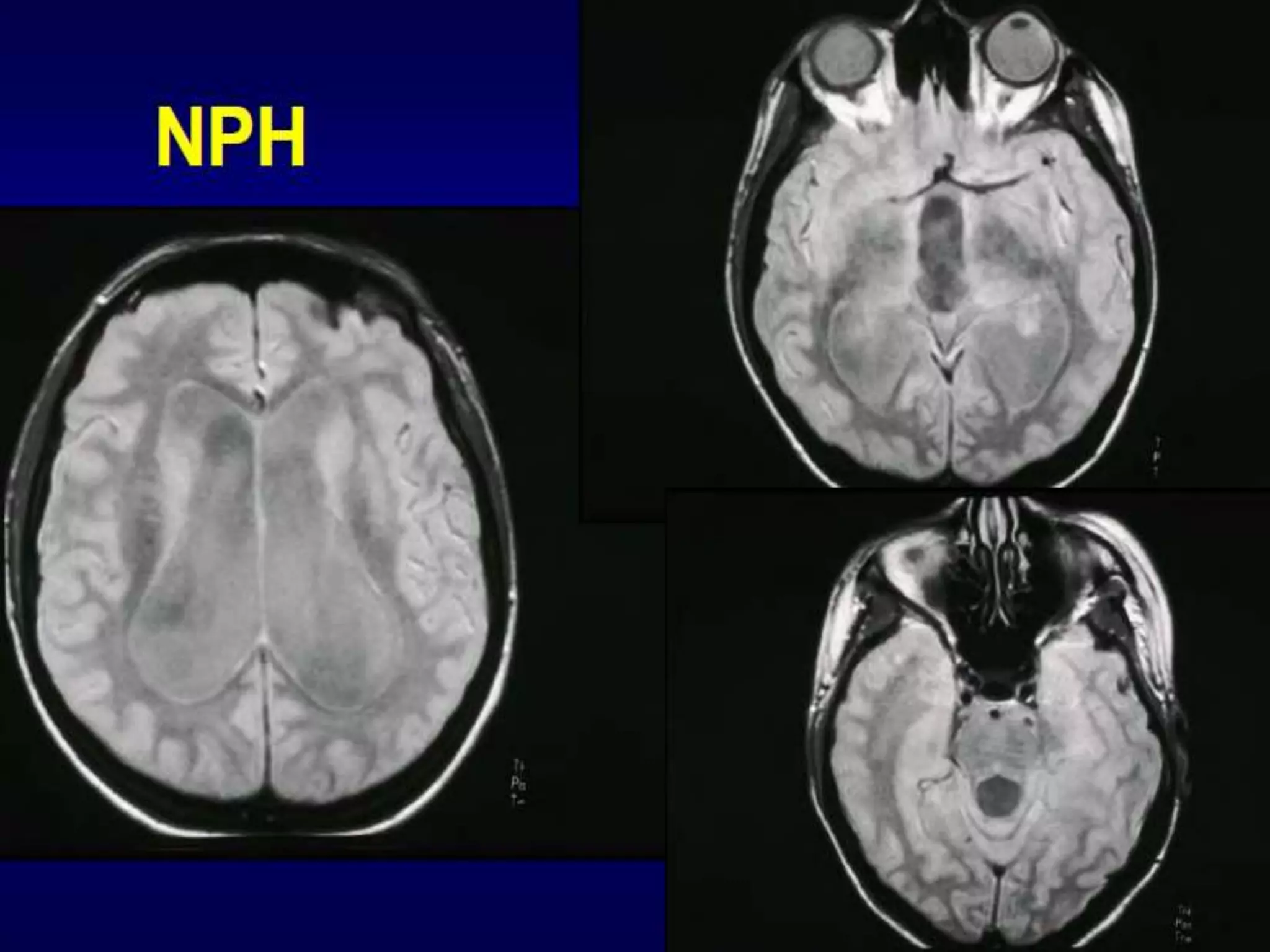
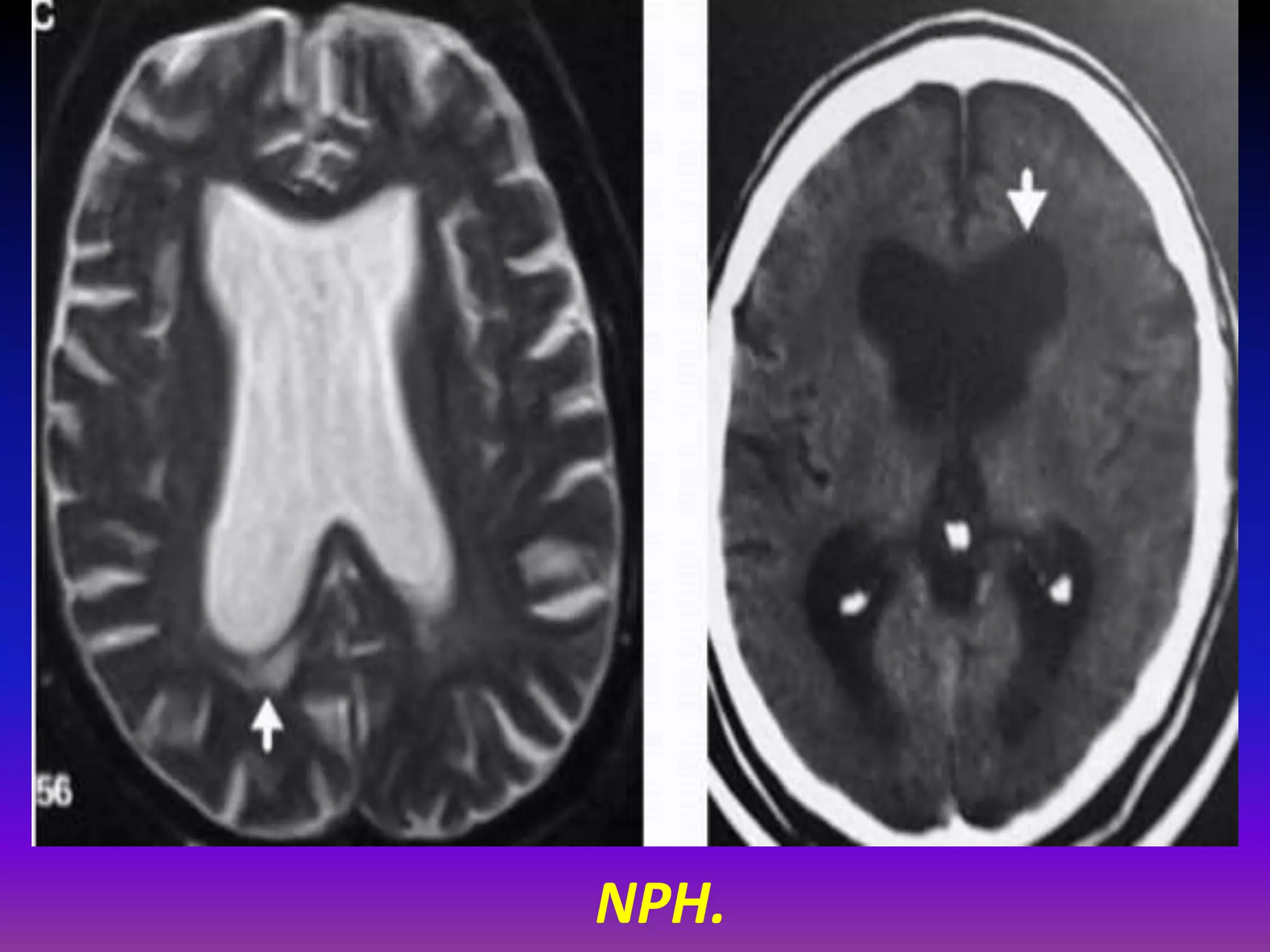
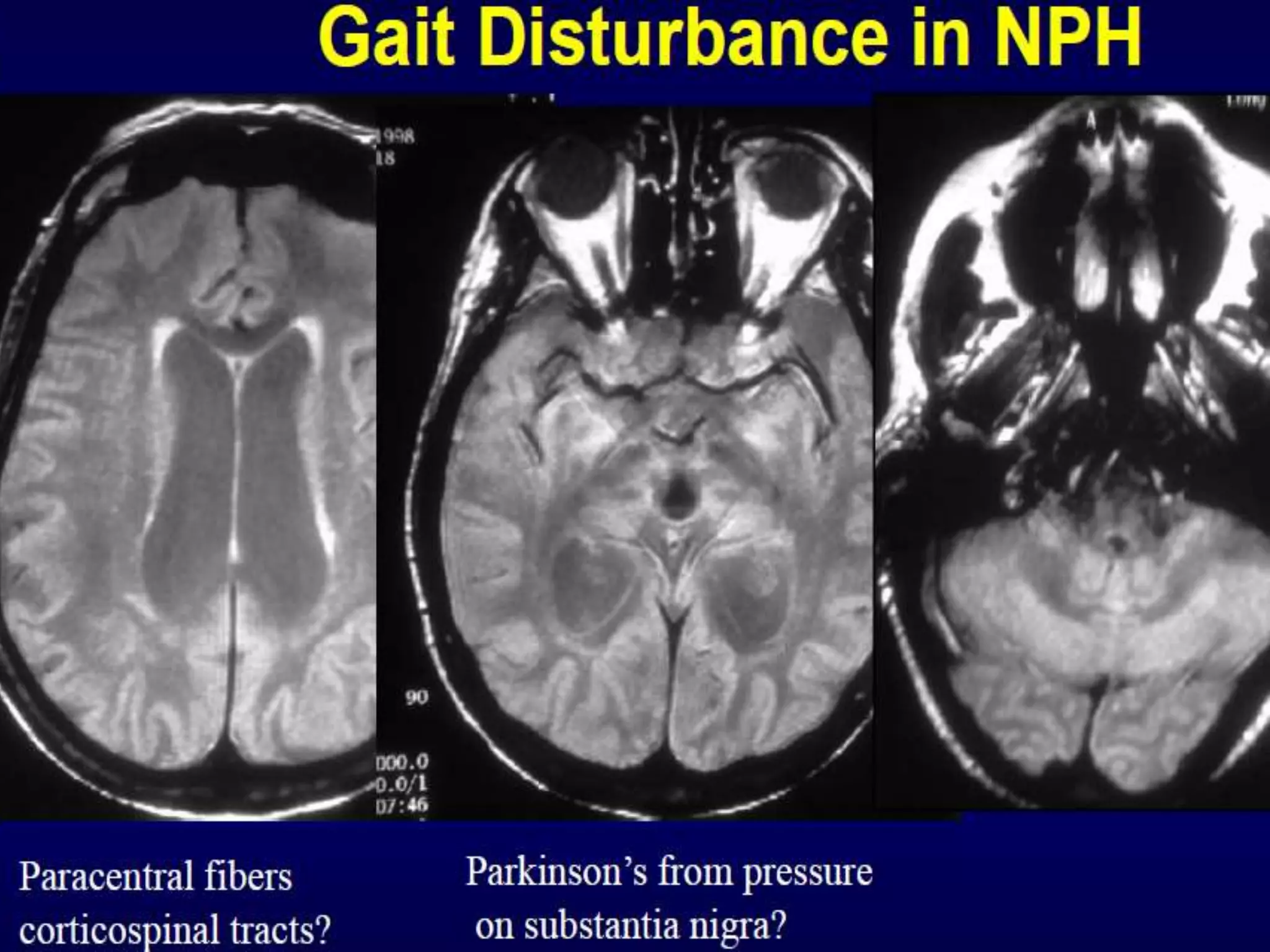
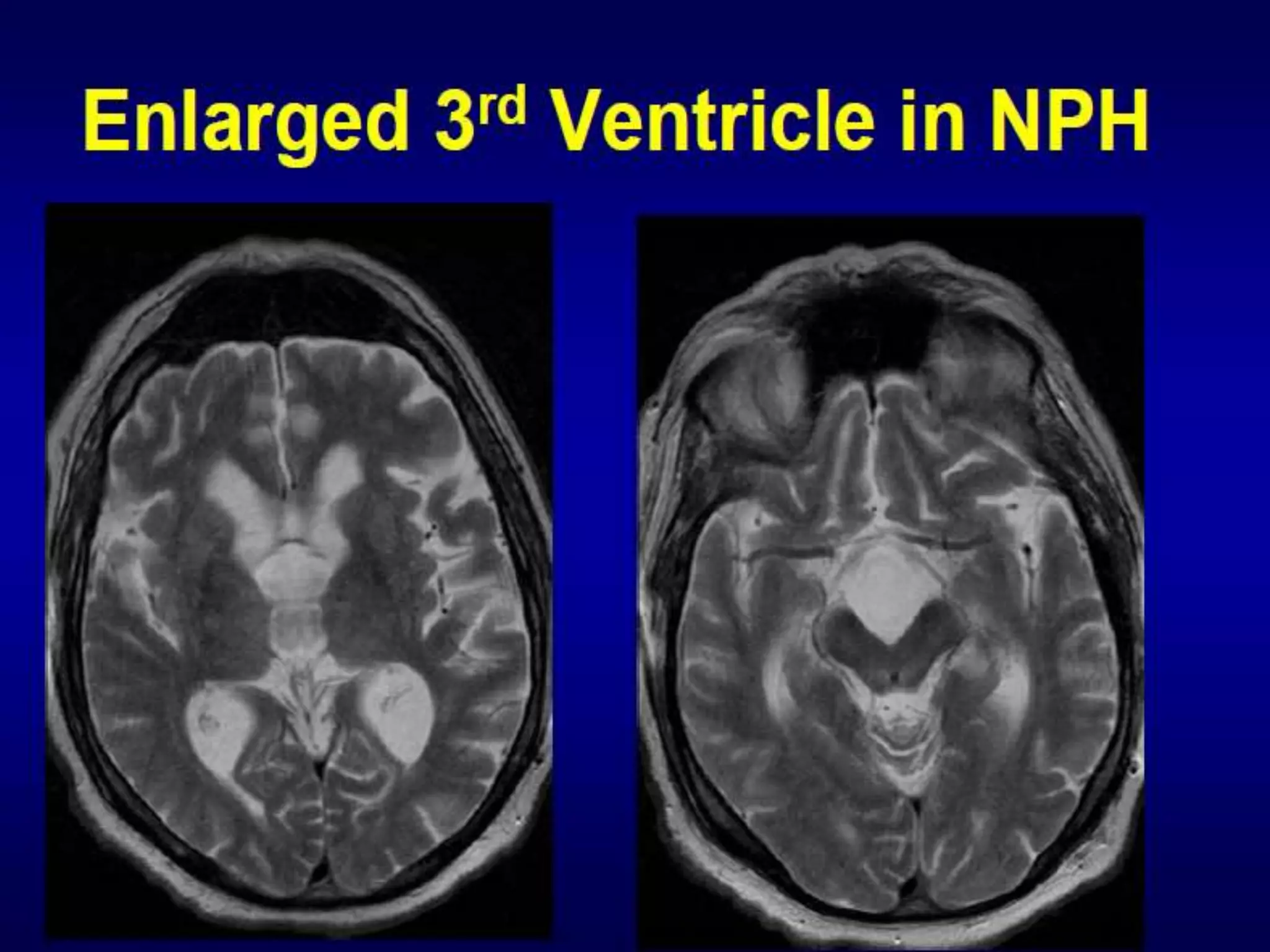
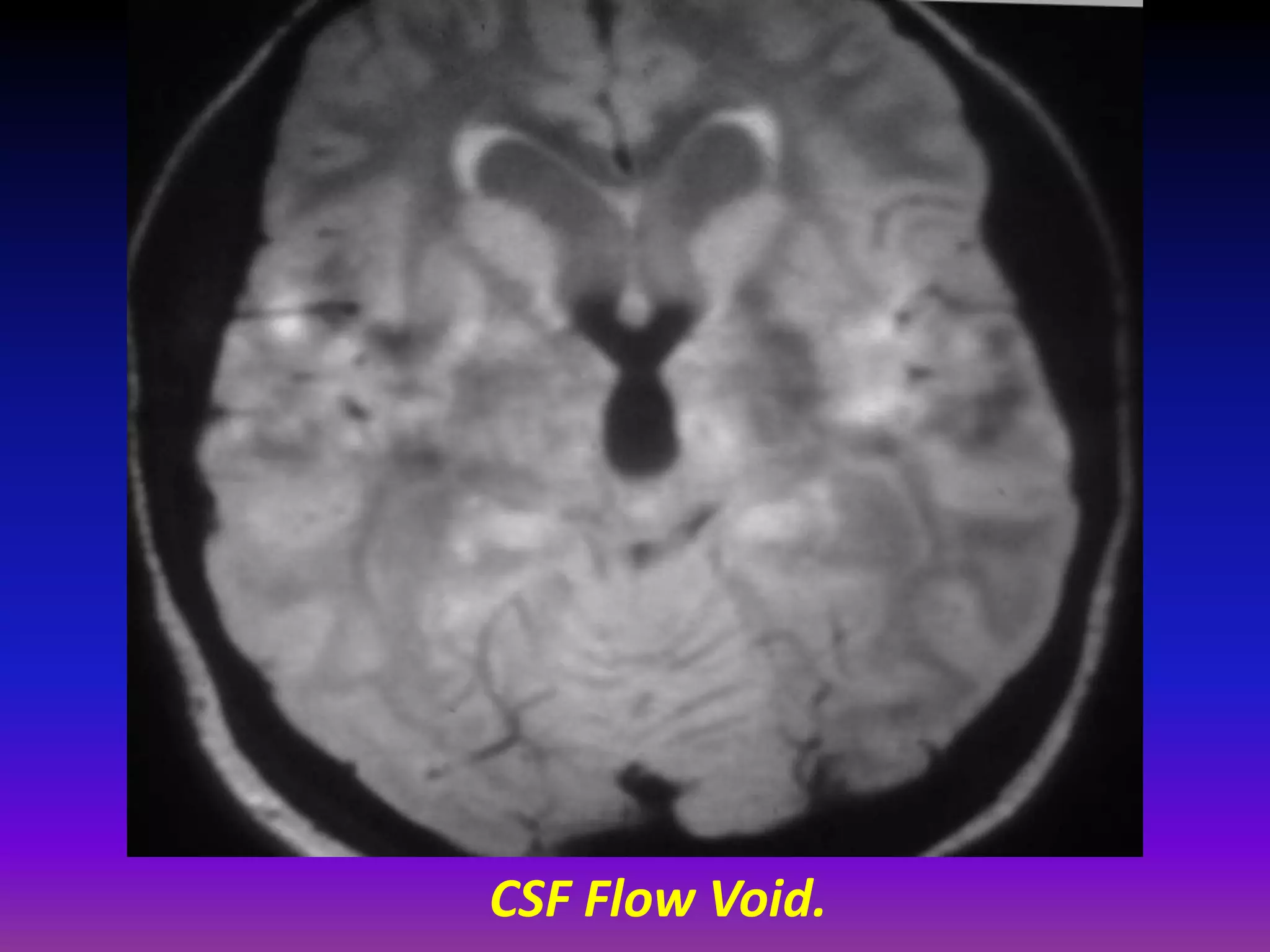
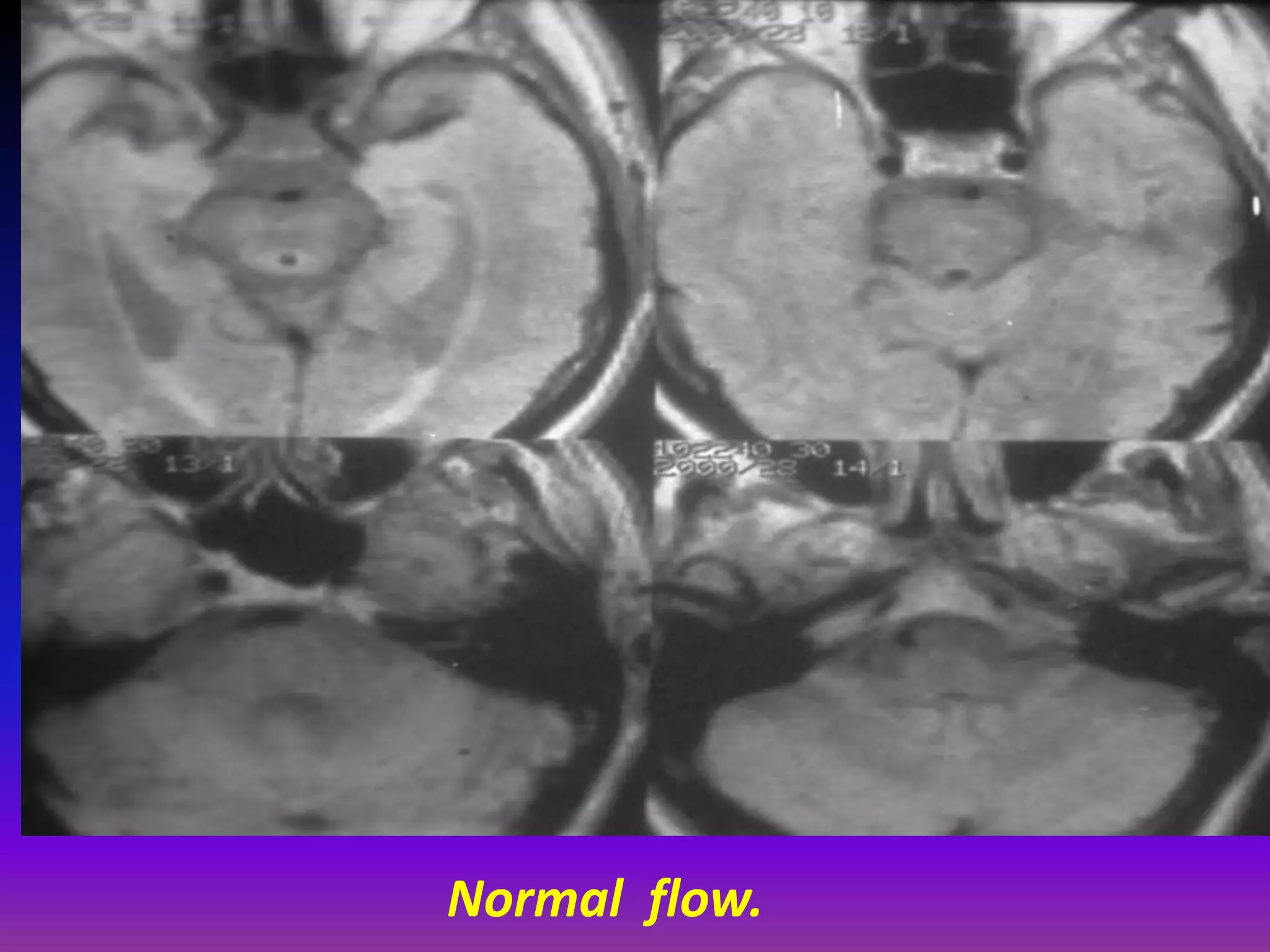
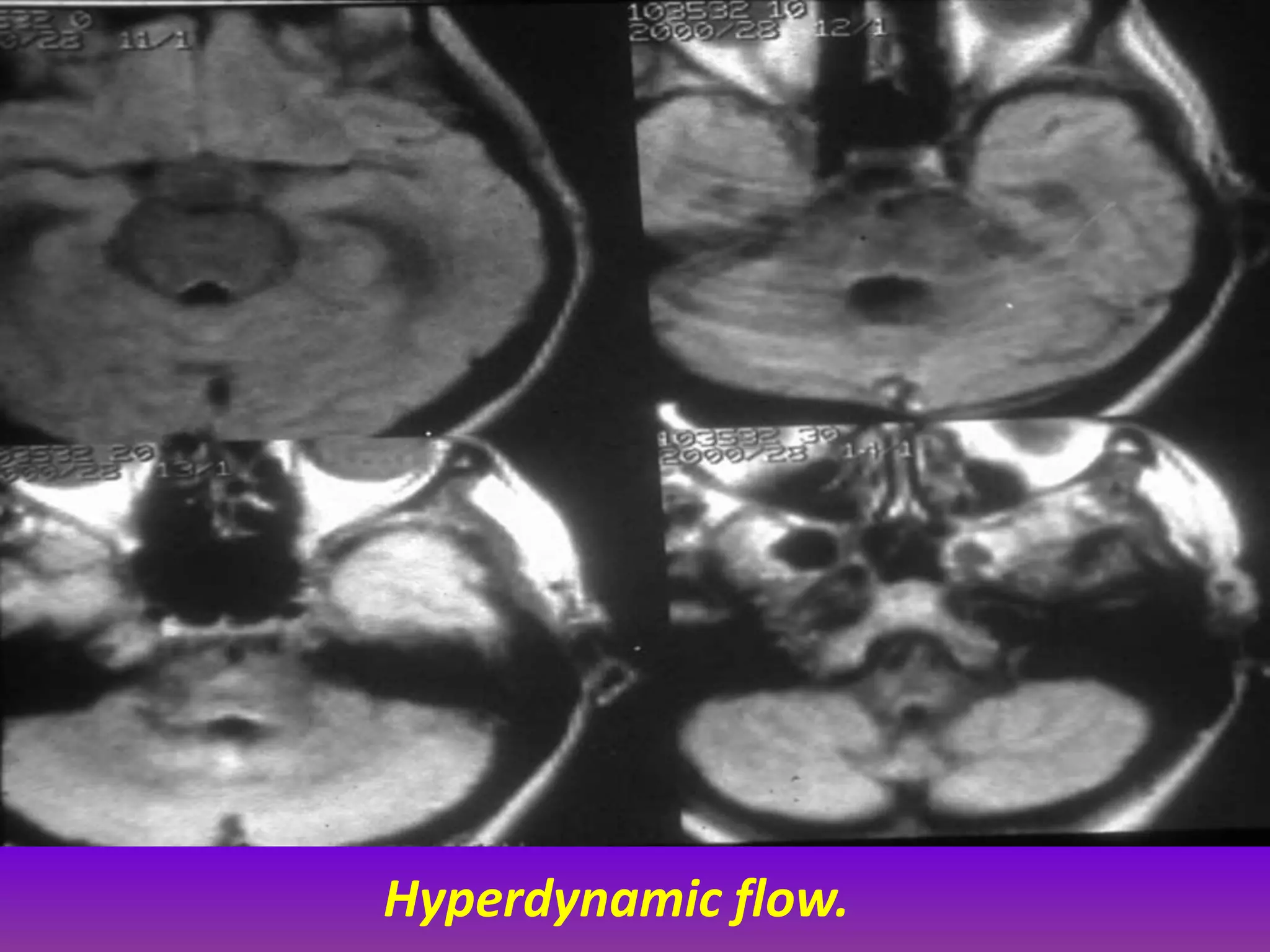
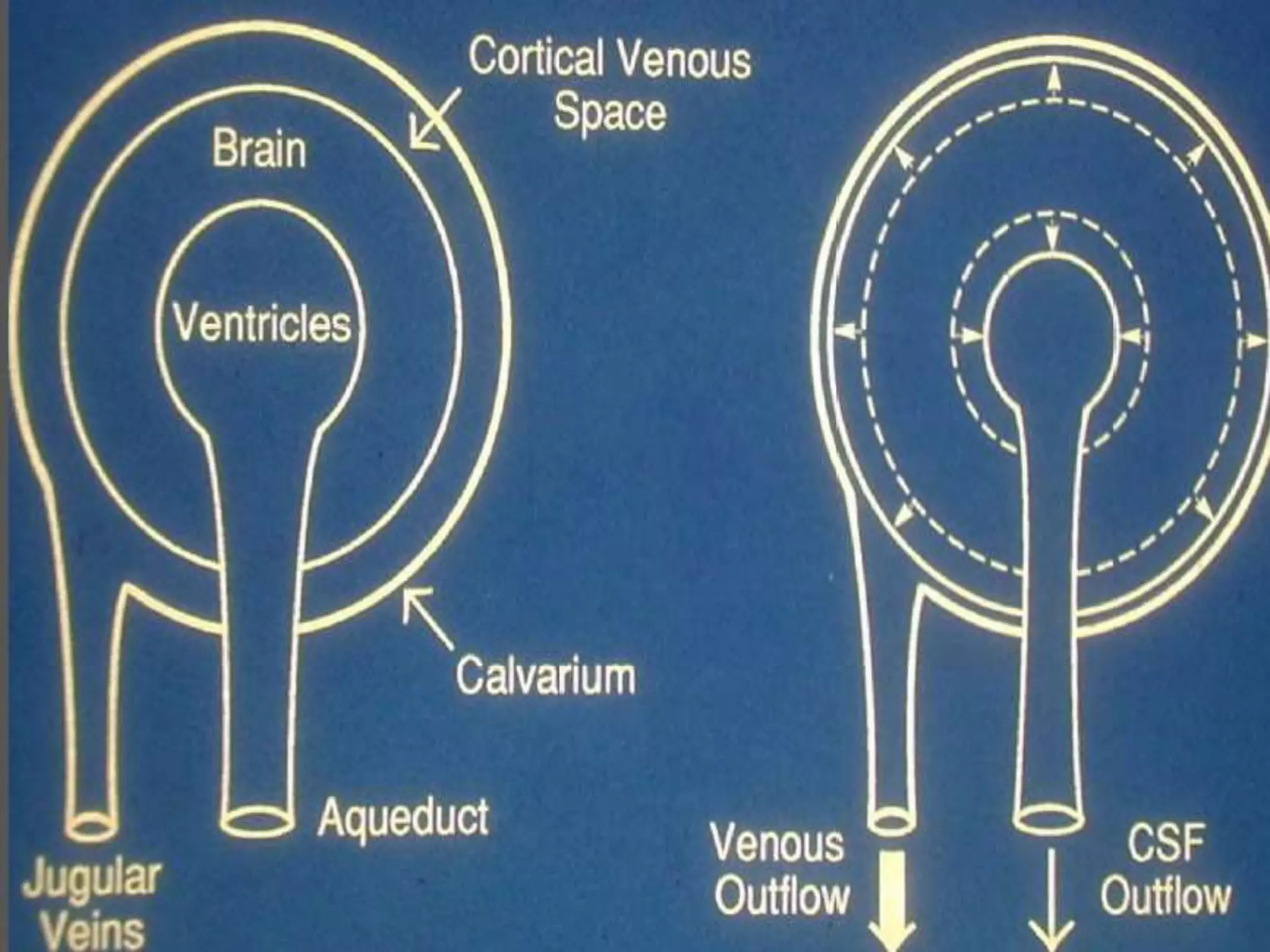
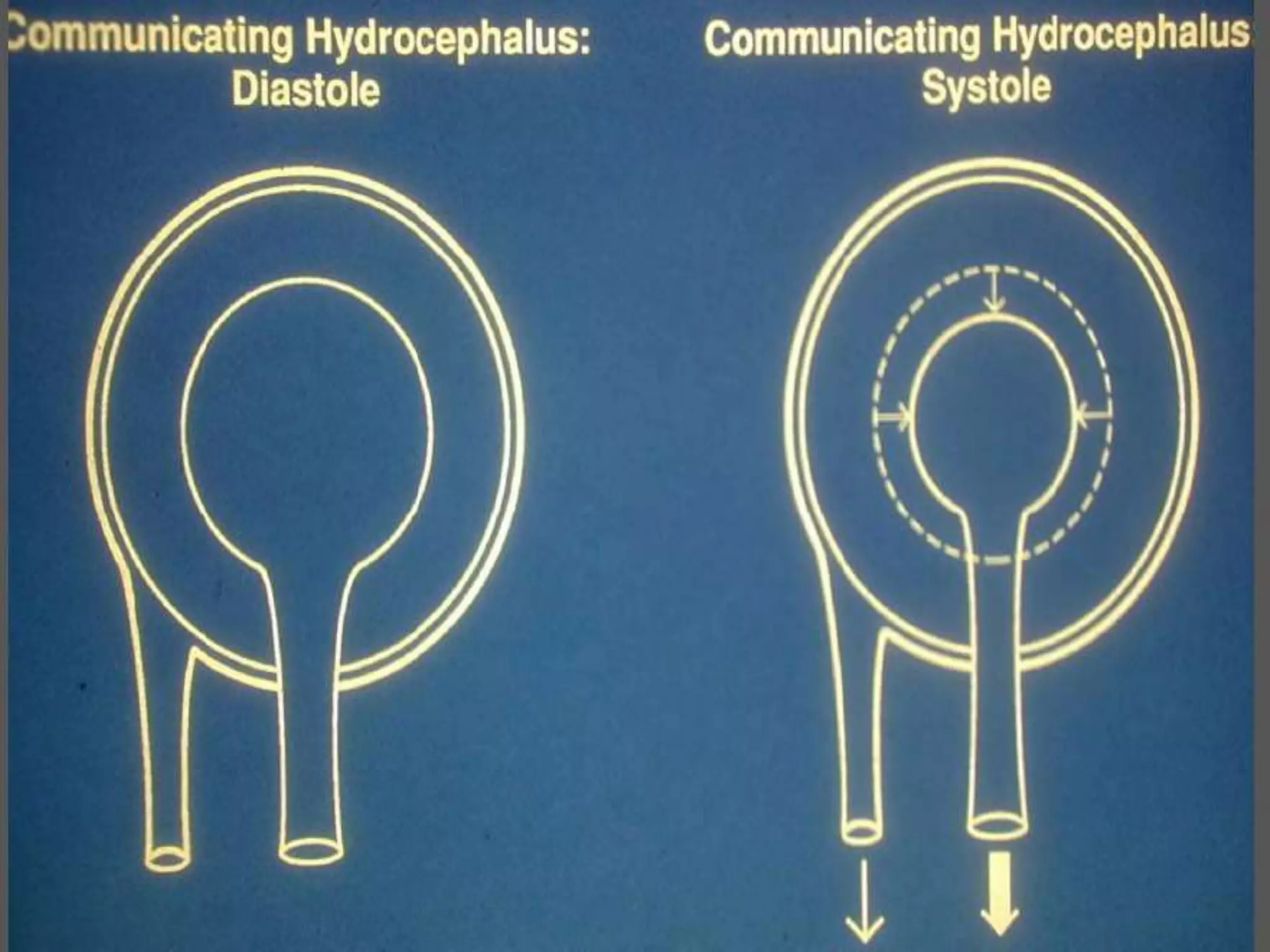
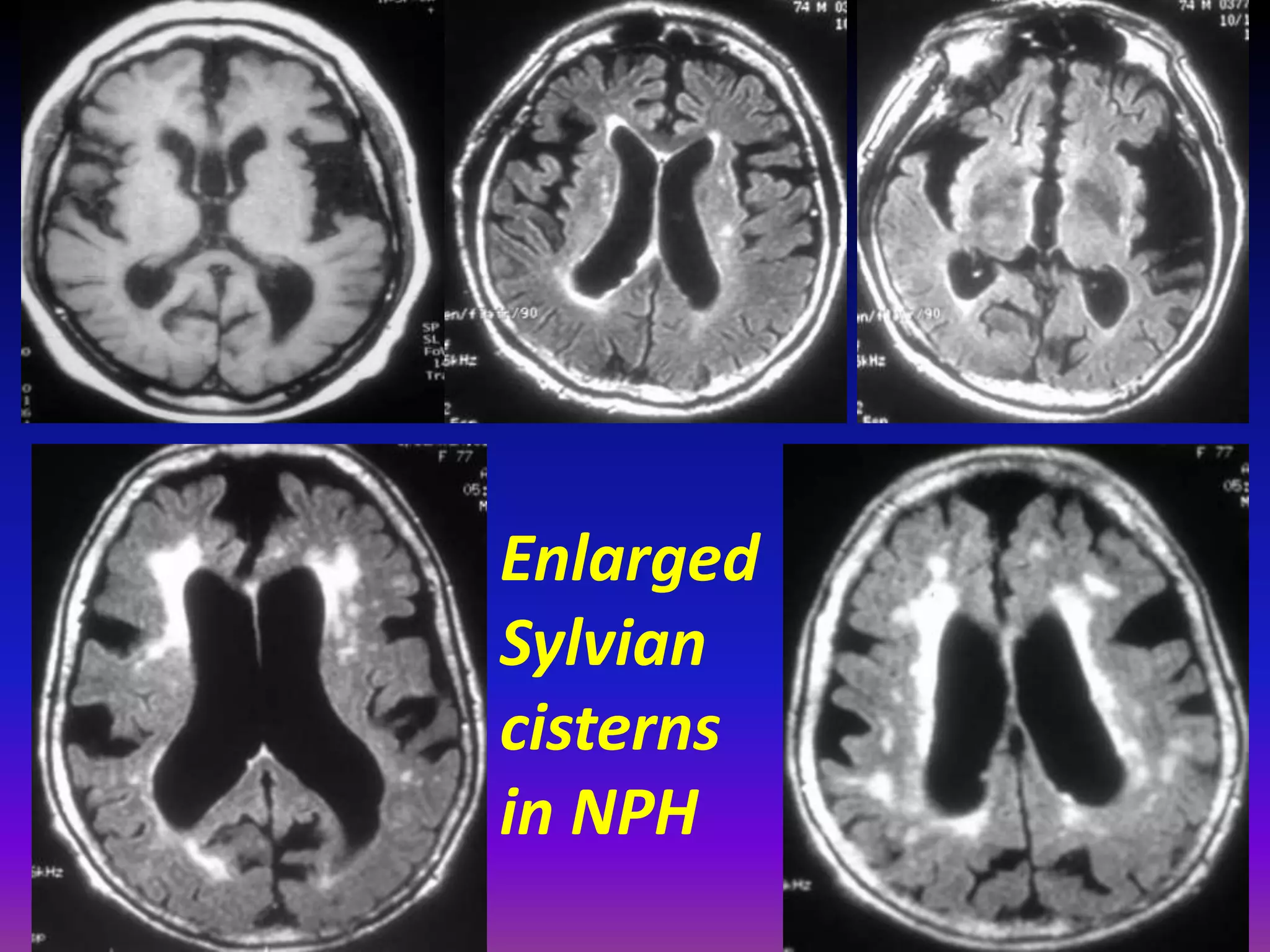
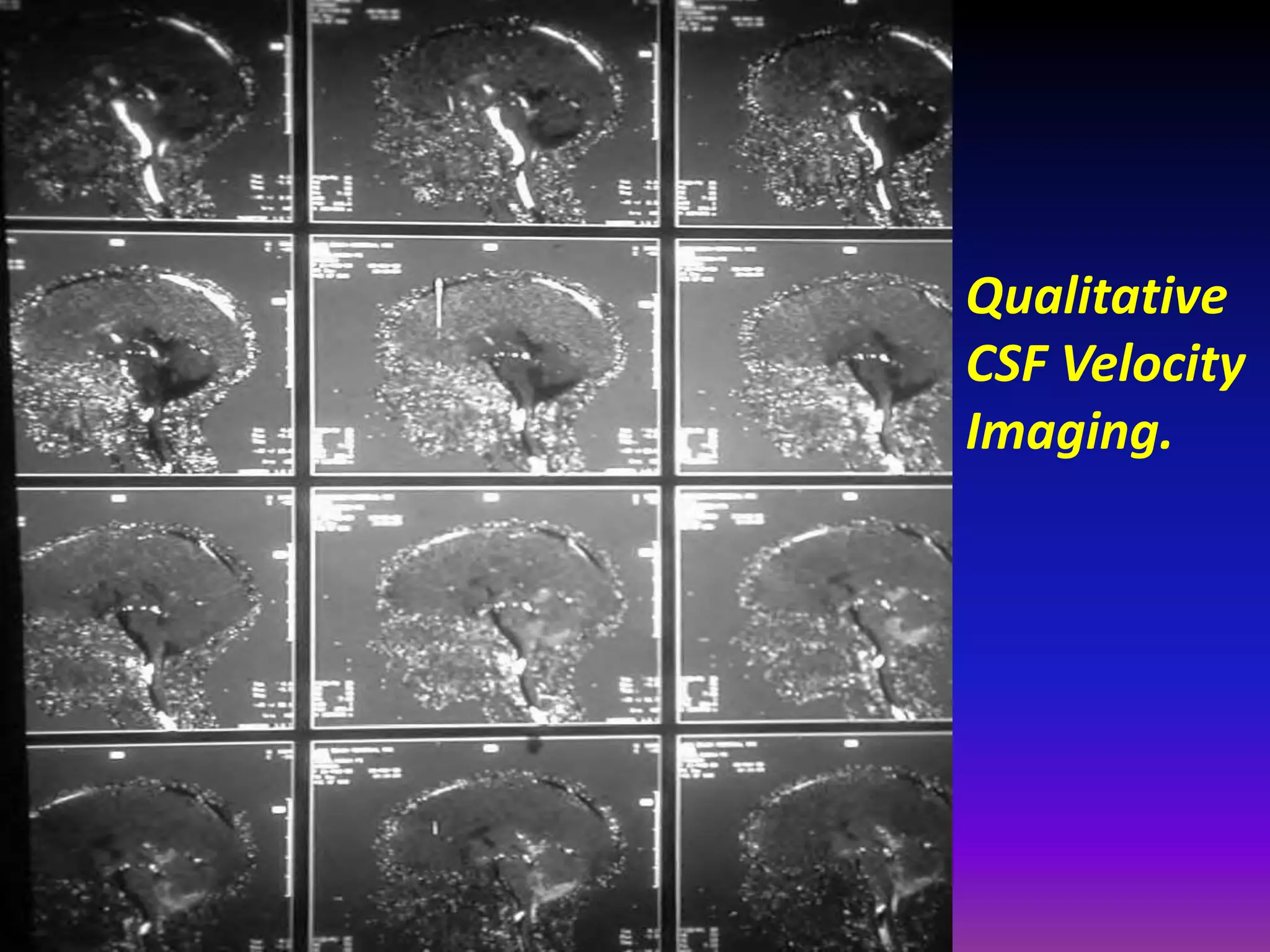
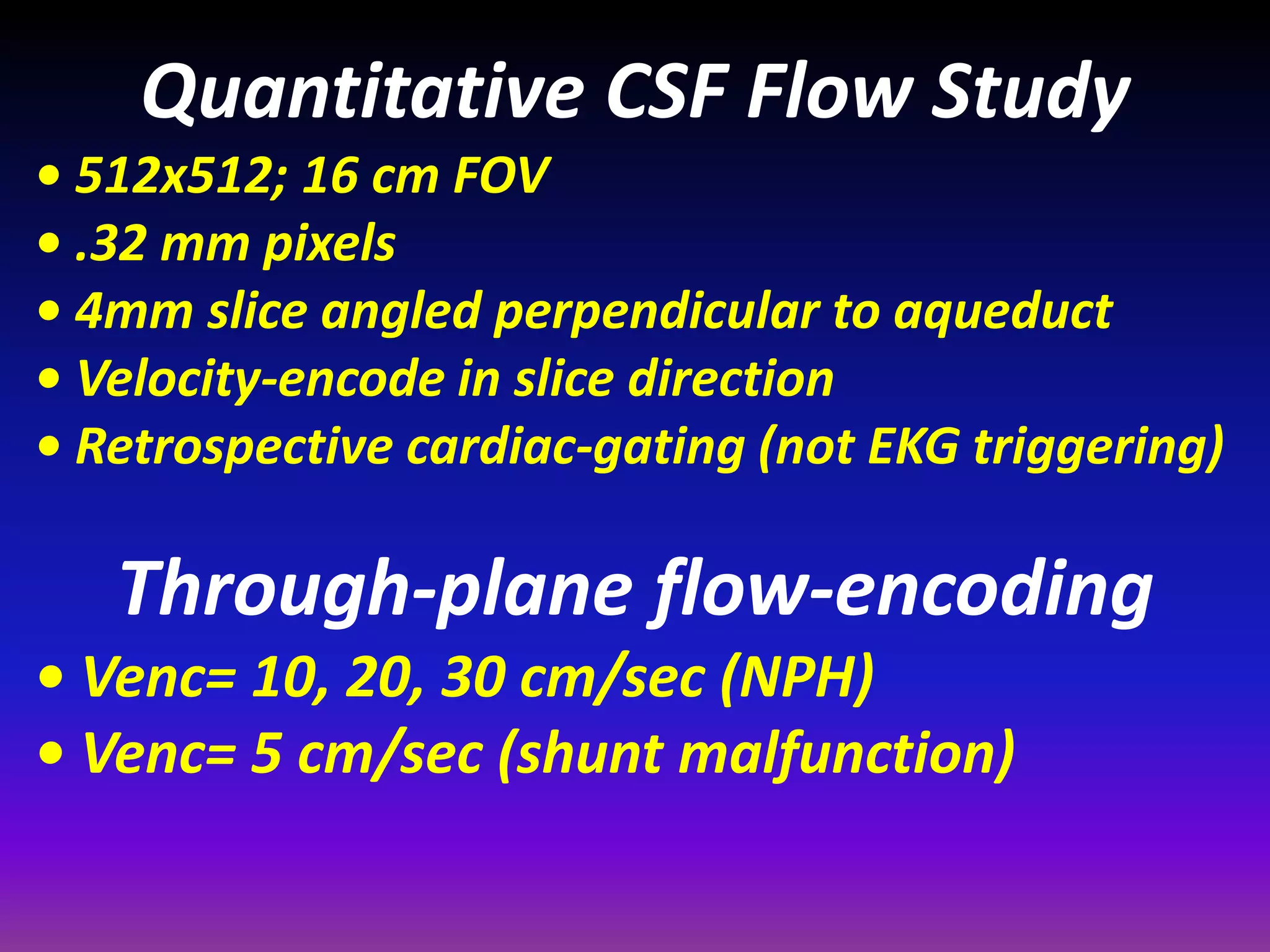
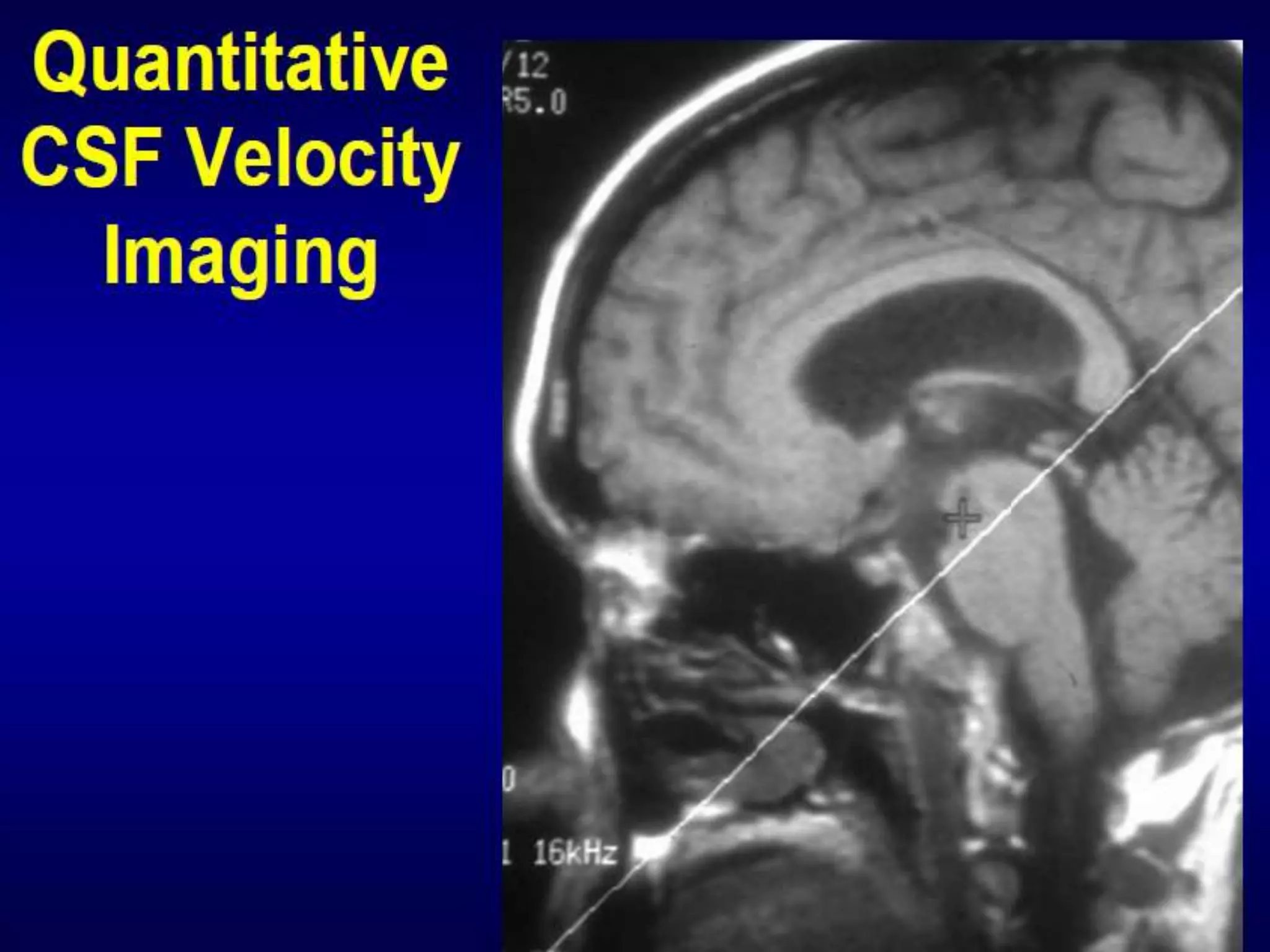
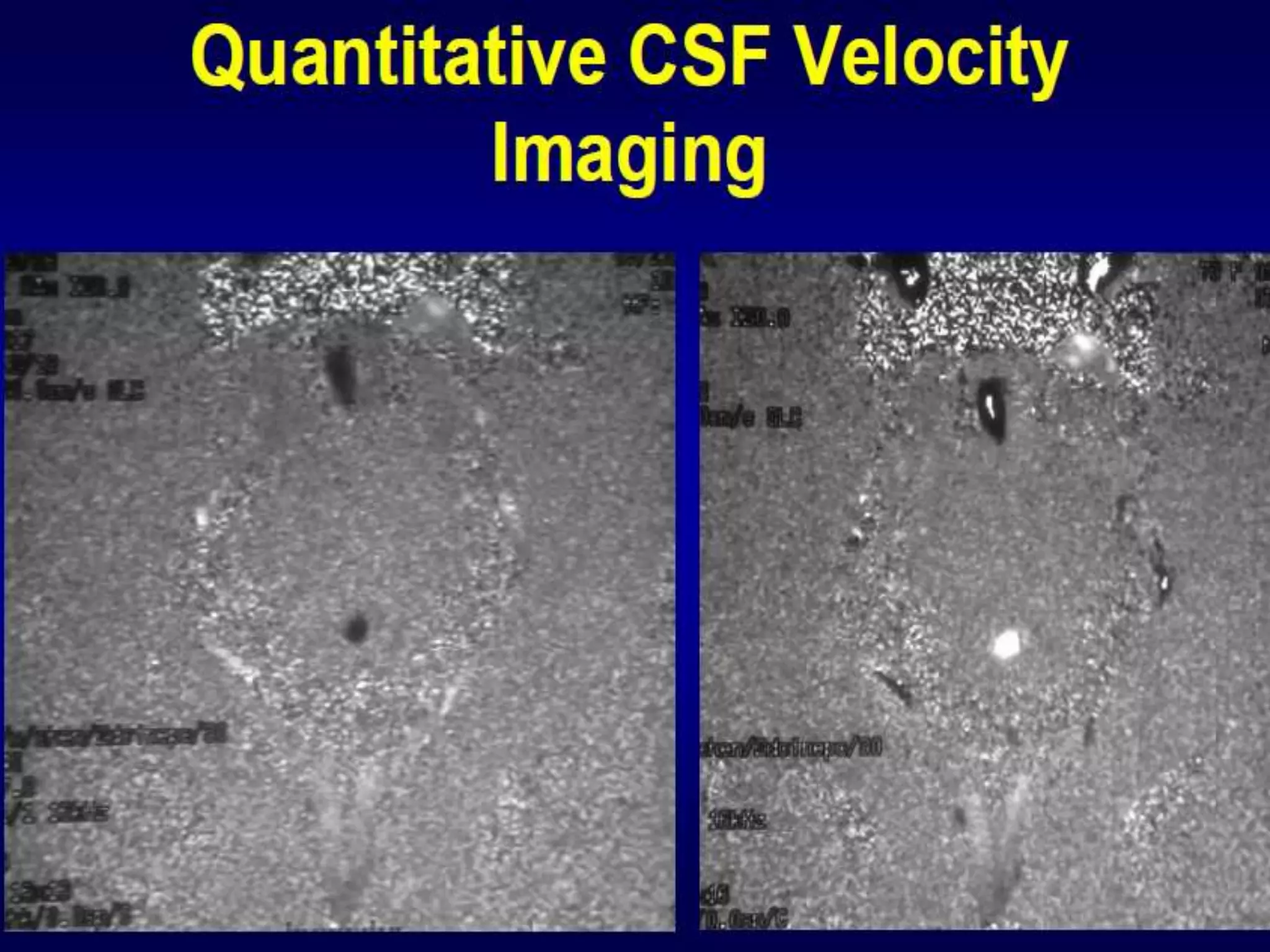
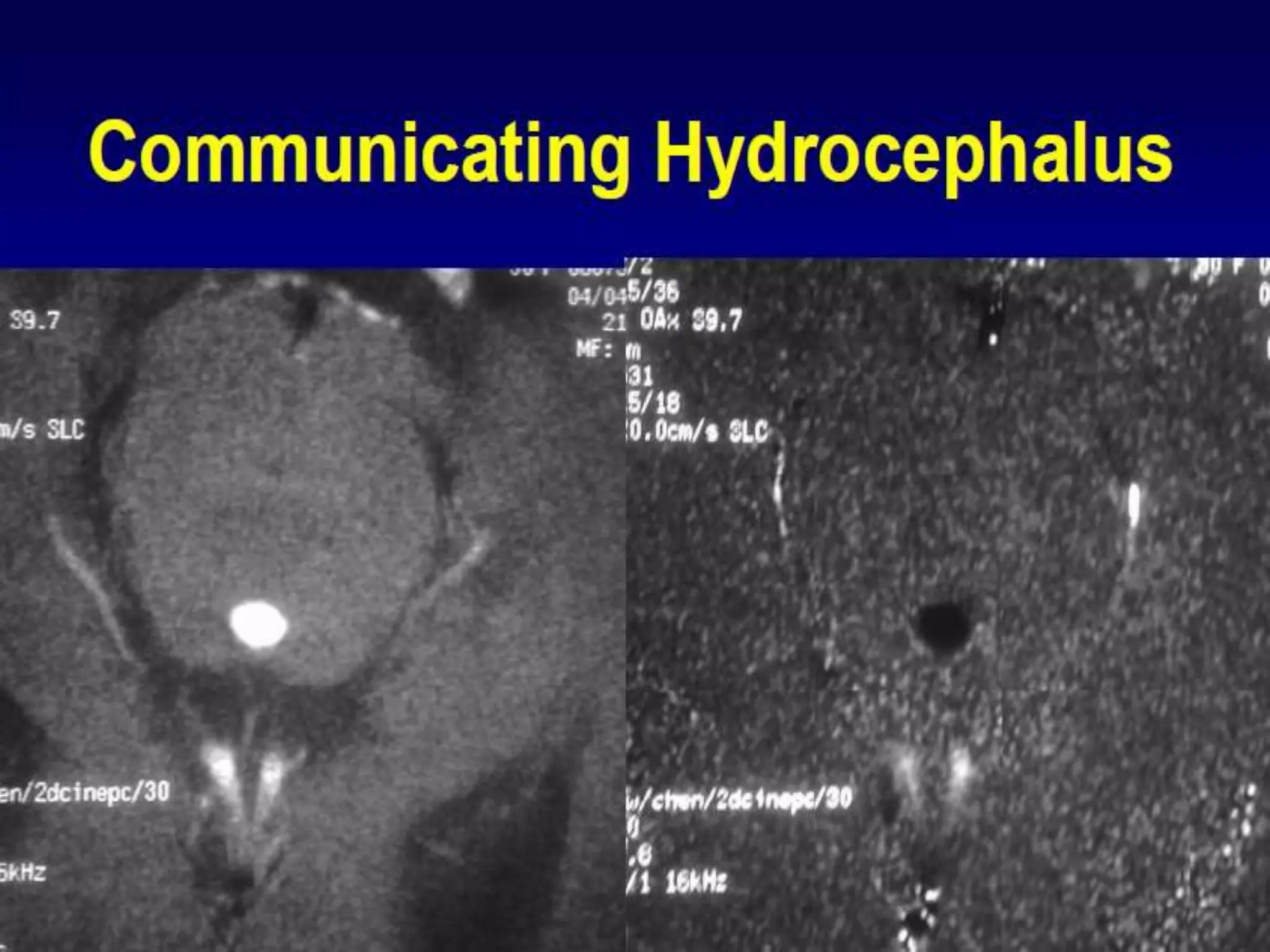
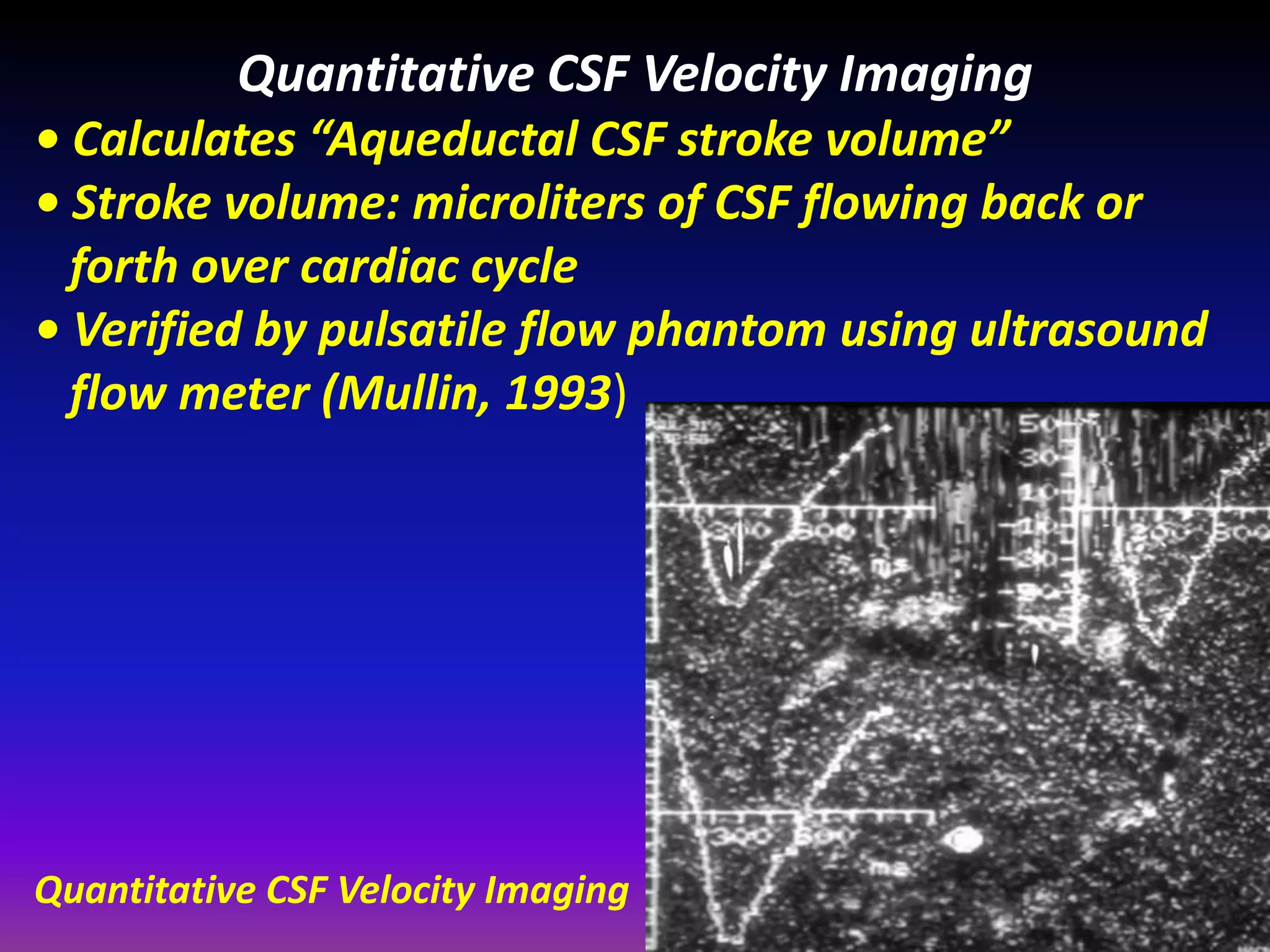
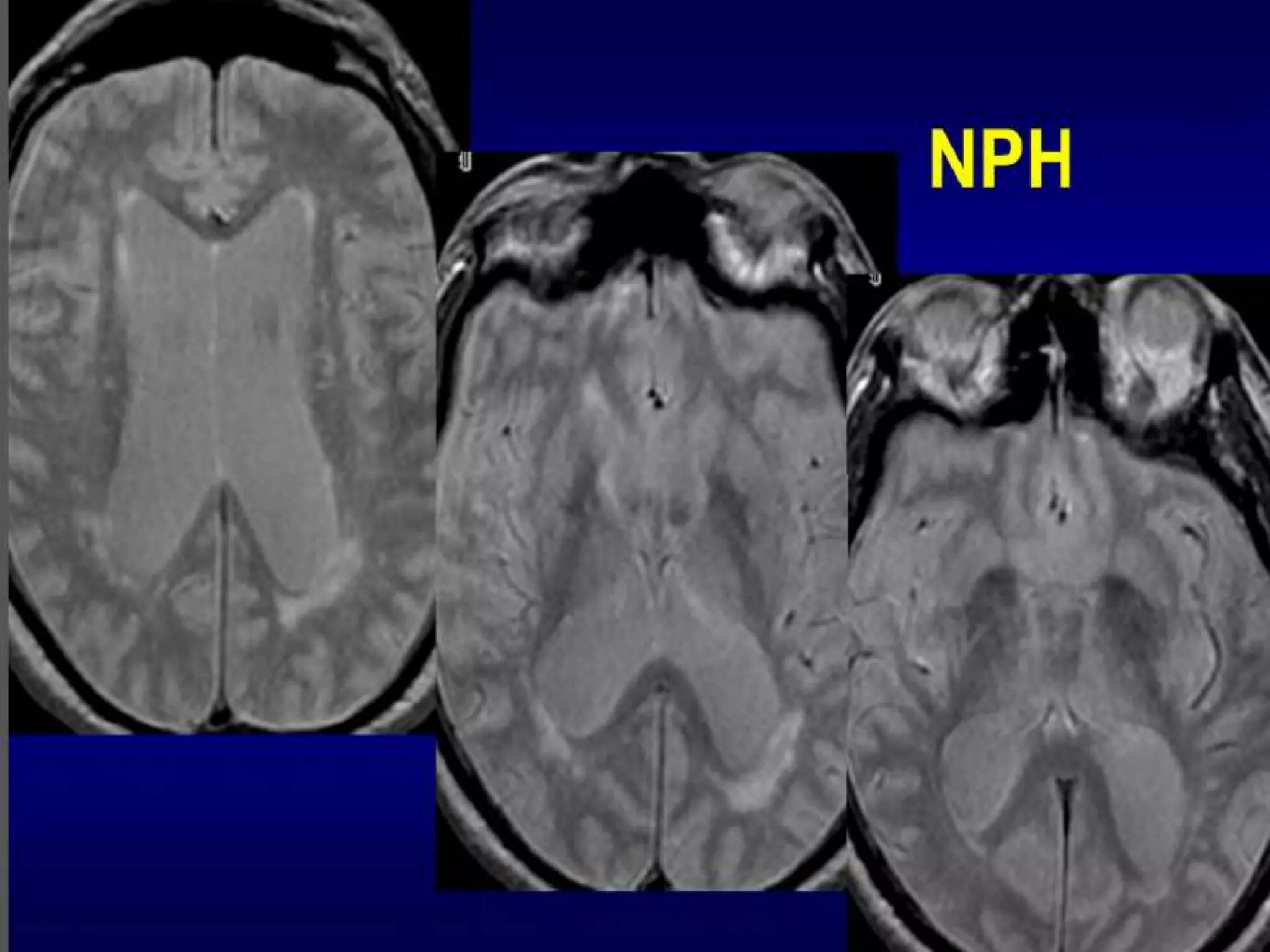
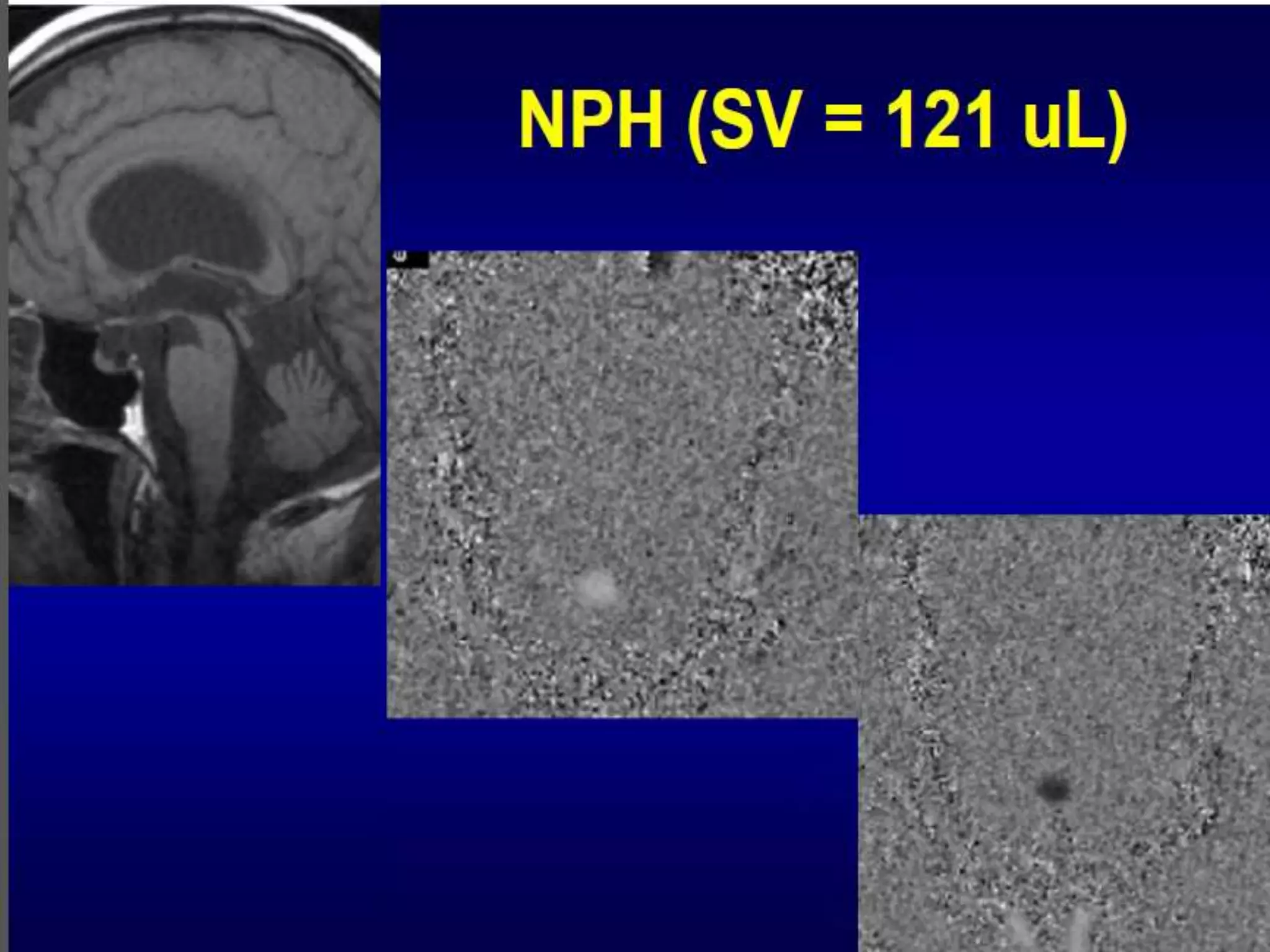
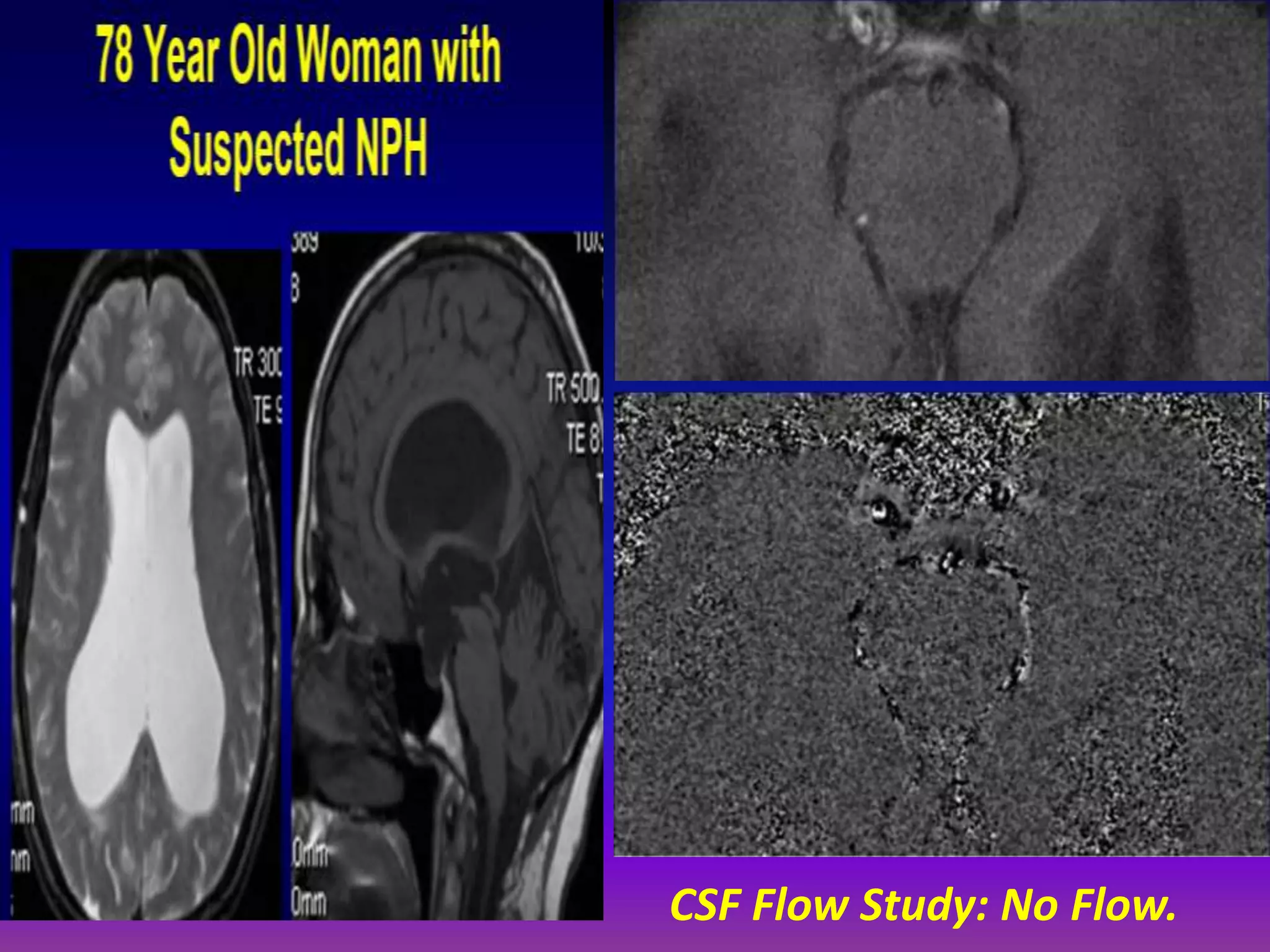
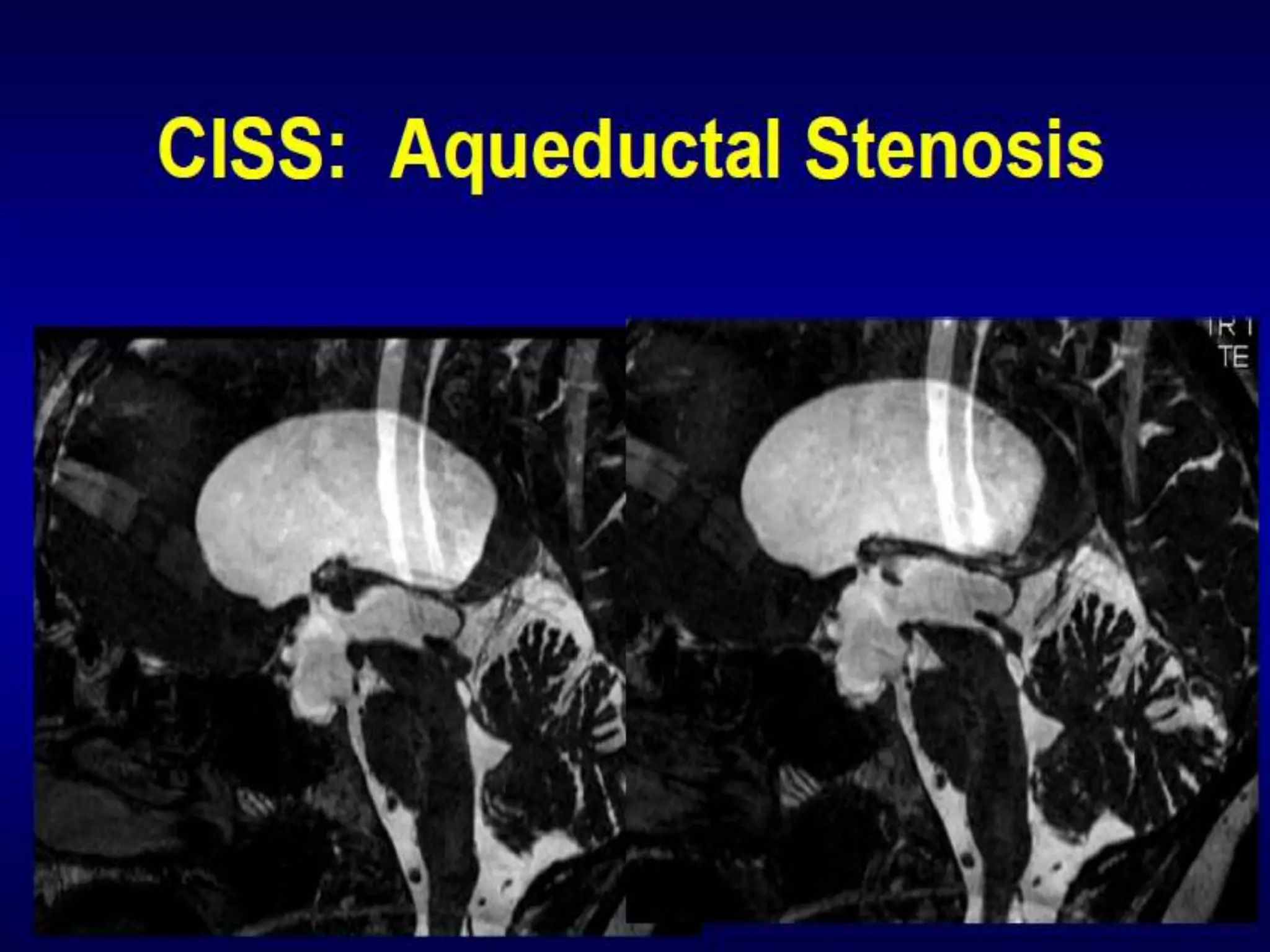
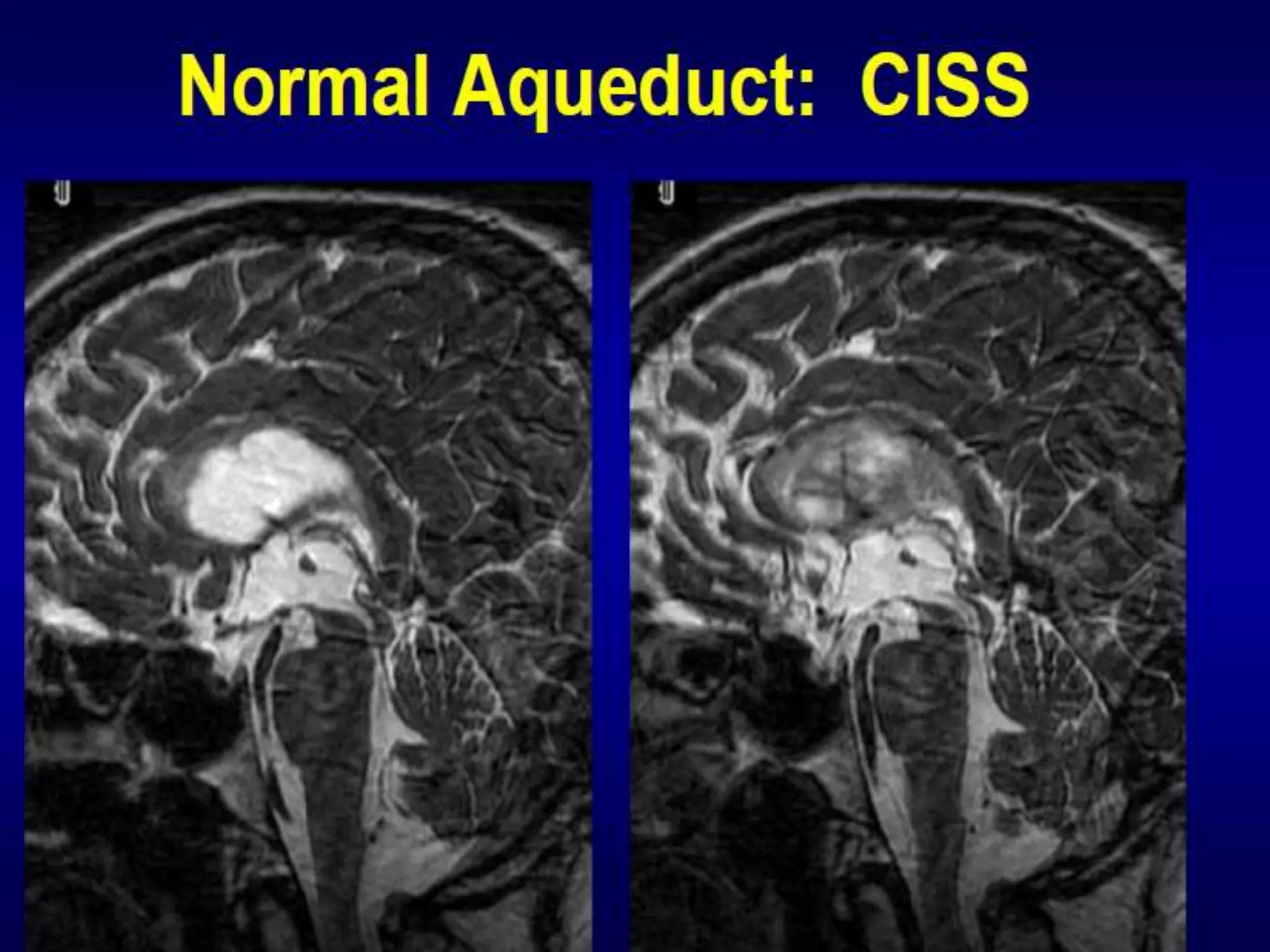
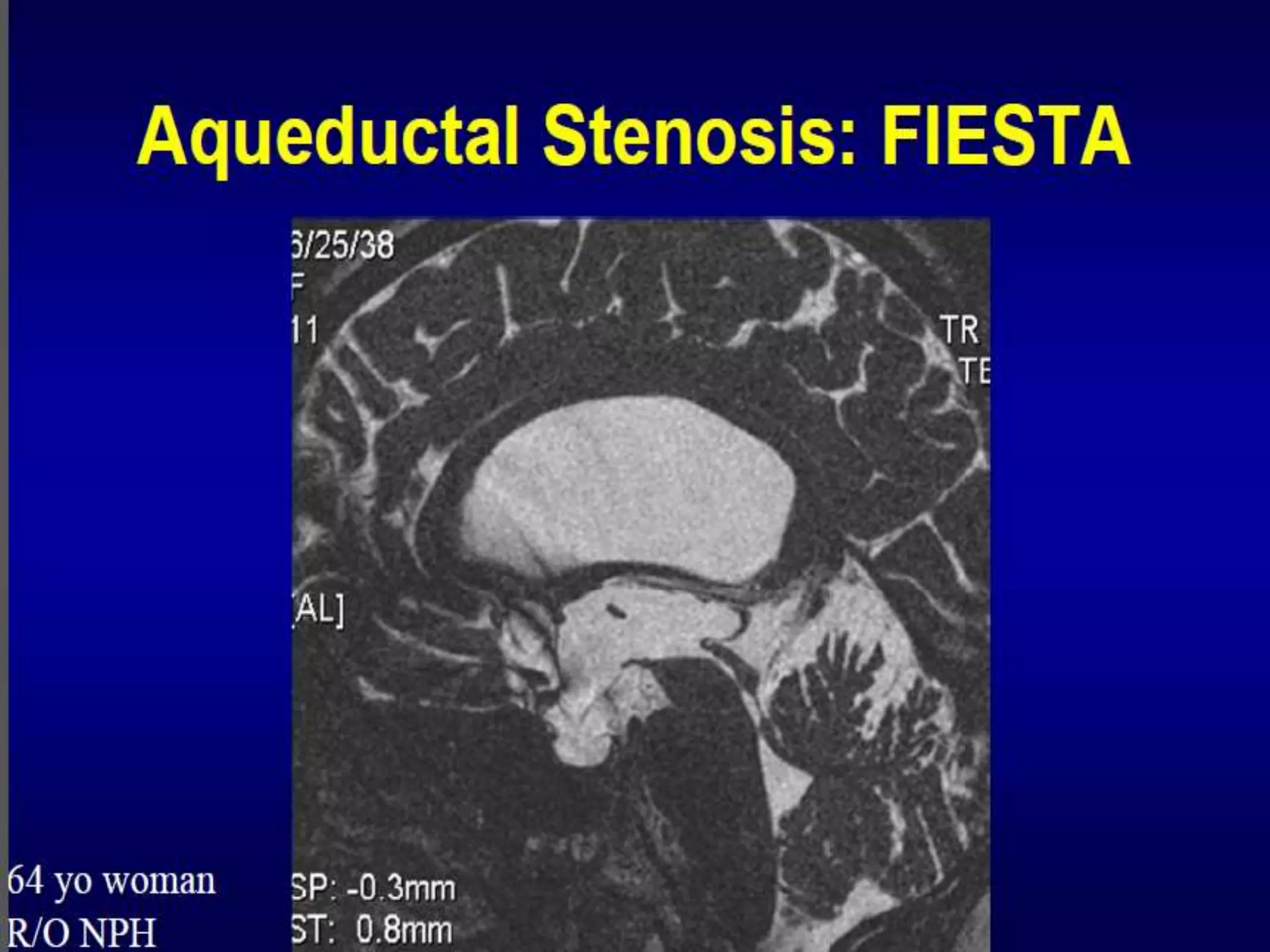
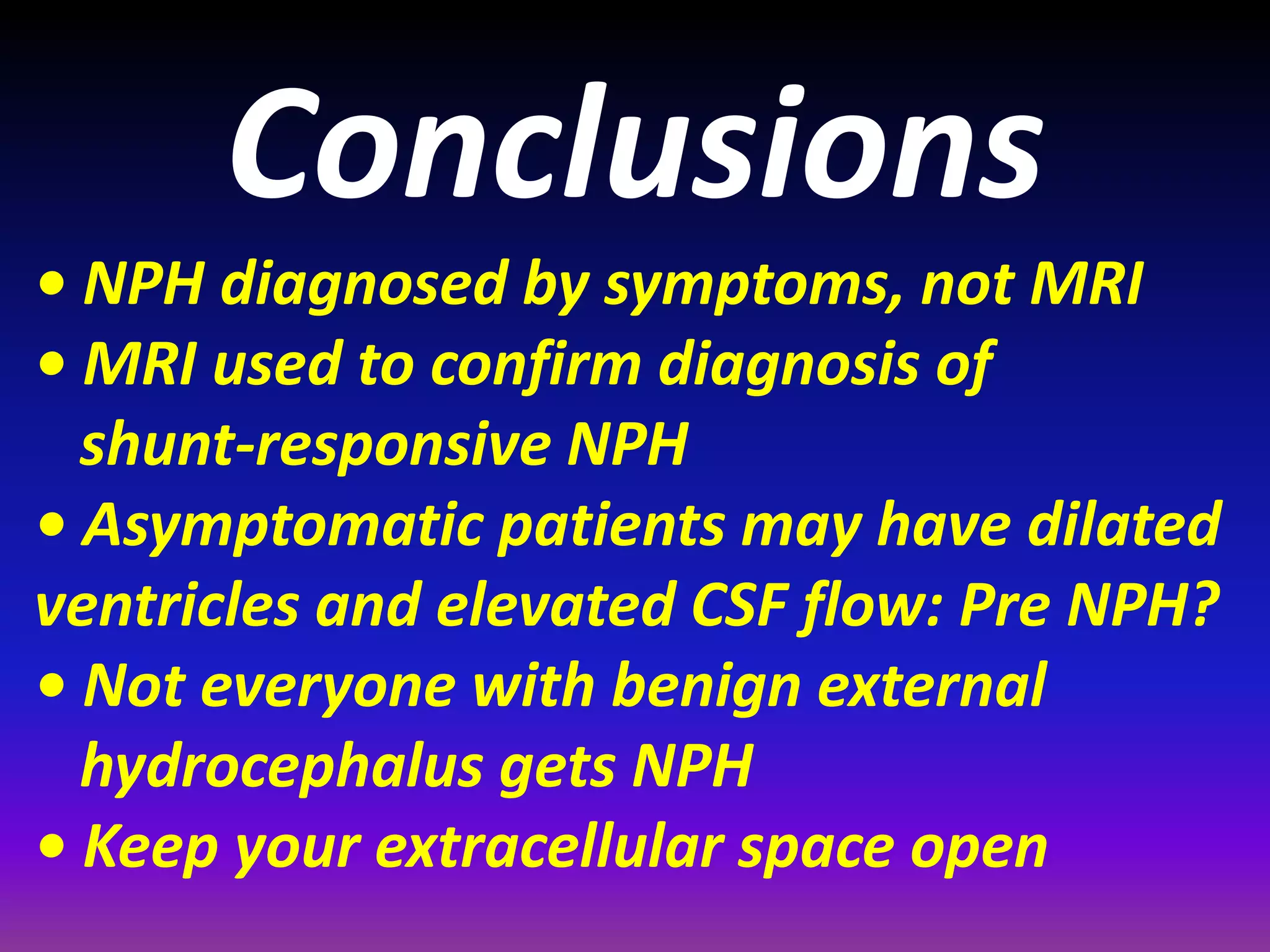
This document discusses radiological imaging techniques for evaluating hydrocephalus. It describes various imaging findings in different types of hydrocephalus like congenital hydrocephalus and hydrocephalus secondary to tumors. It focuses on techniques for evaluating normal pressure hydrocephalus (NPH), including phase contrast MRI to quantify cerebrospinal fluid flow. It hypothesizes that NPH may be caused by a combination of naturally enlarged ventricles and later deep white matter ischemia restricting CSF flow, leading to symptomatic hydrocephalus. Quantitative CSF flow studies can help diagnose shunt-responsive NPH.