1. There are many types of neurological gait disorders that can arise from damage or dysfunction in different parts of the brain or nervous system.
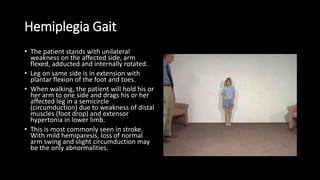
2. Hemiplegic gait results from weakness on one side of the body, like after a stroke, causing the affected leg to drag and circumduct during walking.
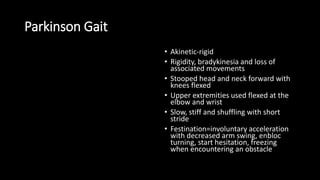
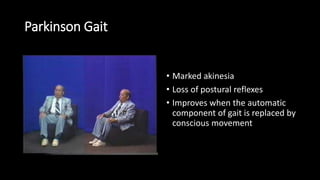
3. Parkinsonian gait is slow, stiff, and shuffling, with loss of arm swing and difficulty initiating movement.