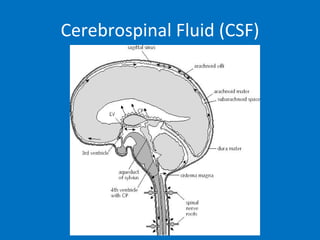
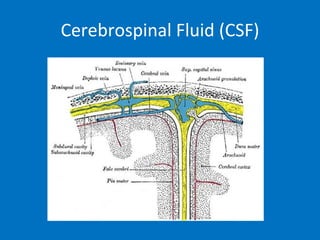
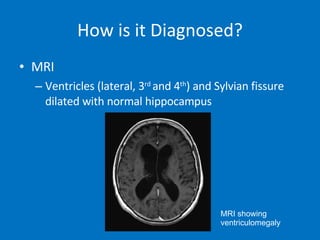
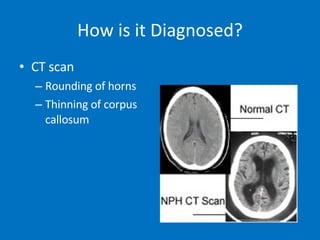
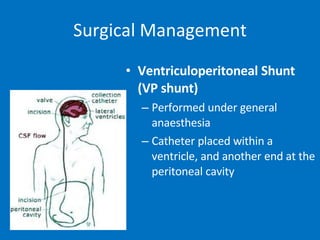
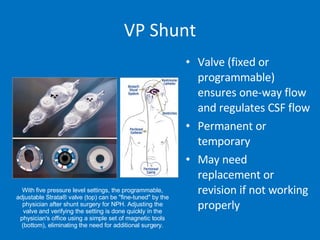
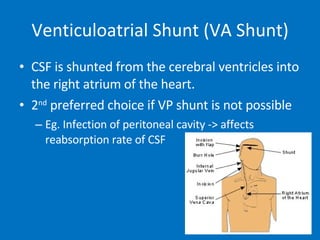
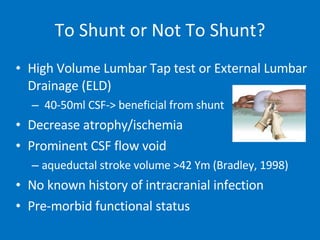
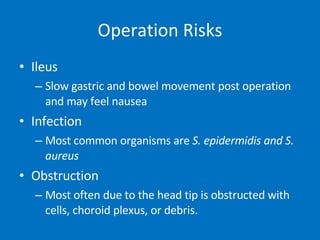
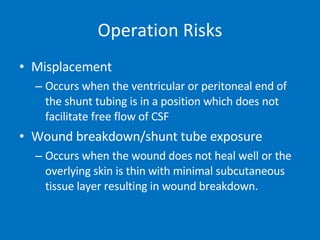
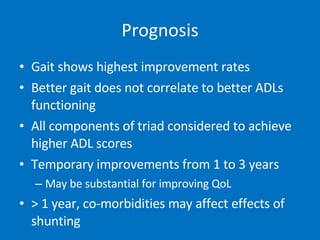
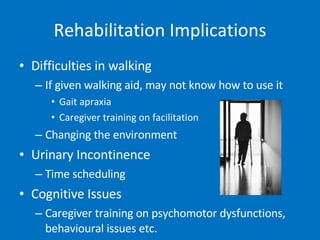
Normal pressure hydrocephalus (NPH) is a condition where cerebrospinal fluid (CSF) absorption is reduced, causing increased pressure in the ventricles of the brain. It typically affects elderly individuals and presents as a triad of symptoms - impaired gait, urinary incontinence, and cognitive impairment. Diagnosis involves MRI or CT scans showing ventricle enlargement. Treatment is usually surgical placement of a shunt to drain CSF from the brain ventricles to the abdominal cavity or heart, which can improve symptoms in many patients. However, shunt surgery also carries risks of complications.