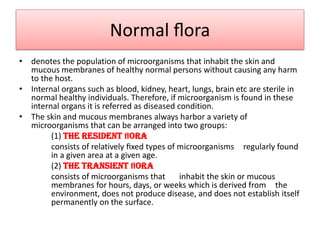
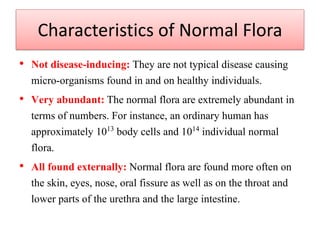
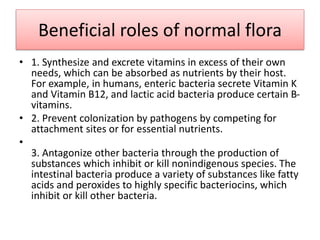
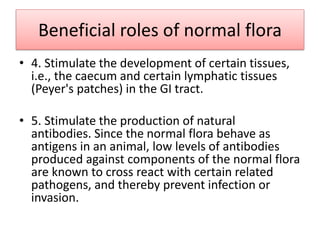
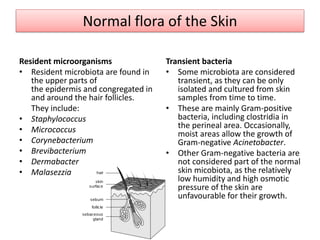
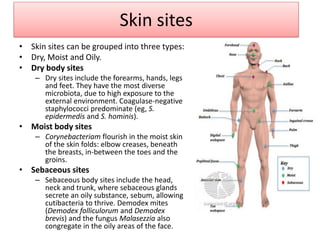
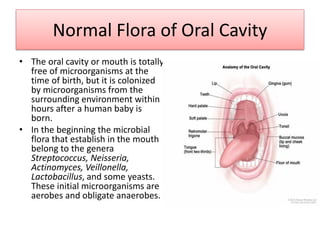
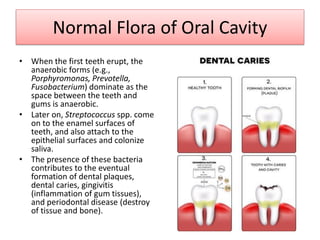
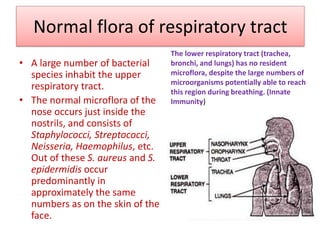
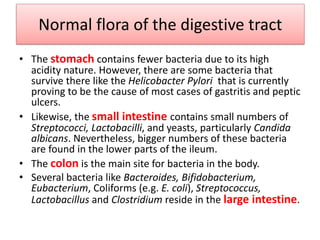
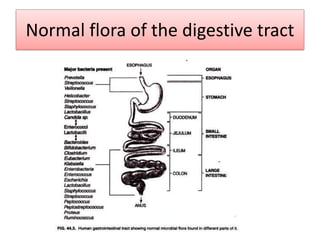
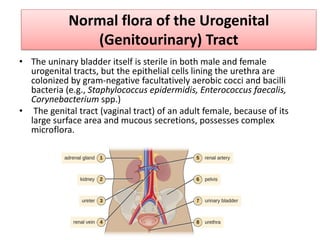
The document discusses normal flora, which are microorganisms that inhabit healthy humans without causing harm. Normal flora are found on skin and mucous membranes but not inside organs. The skin and mucous membranes harbor both resident and transient flora. The document then describes characteristics, types, roles, and locations of normal flora in different parts of the body including skin, oral cavity, respiratory tract, digestive tract, and urogenital tract. Common genera of normal flora are discussed for each location.