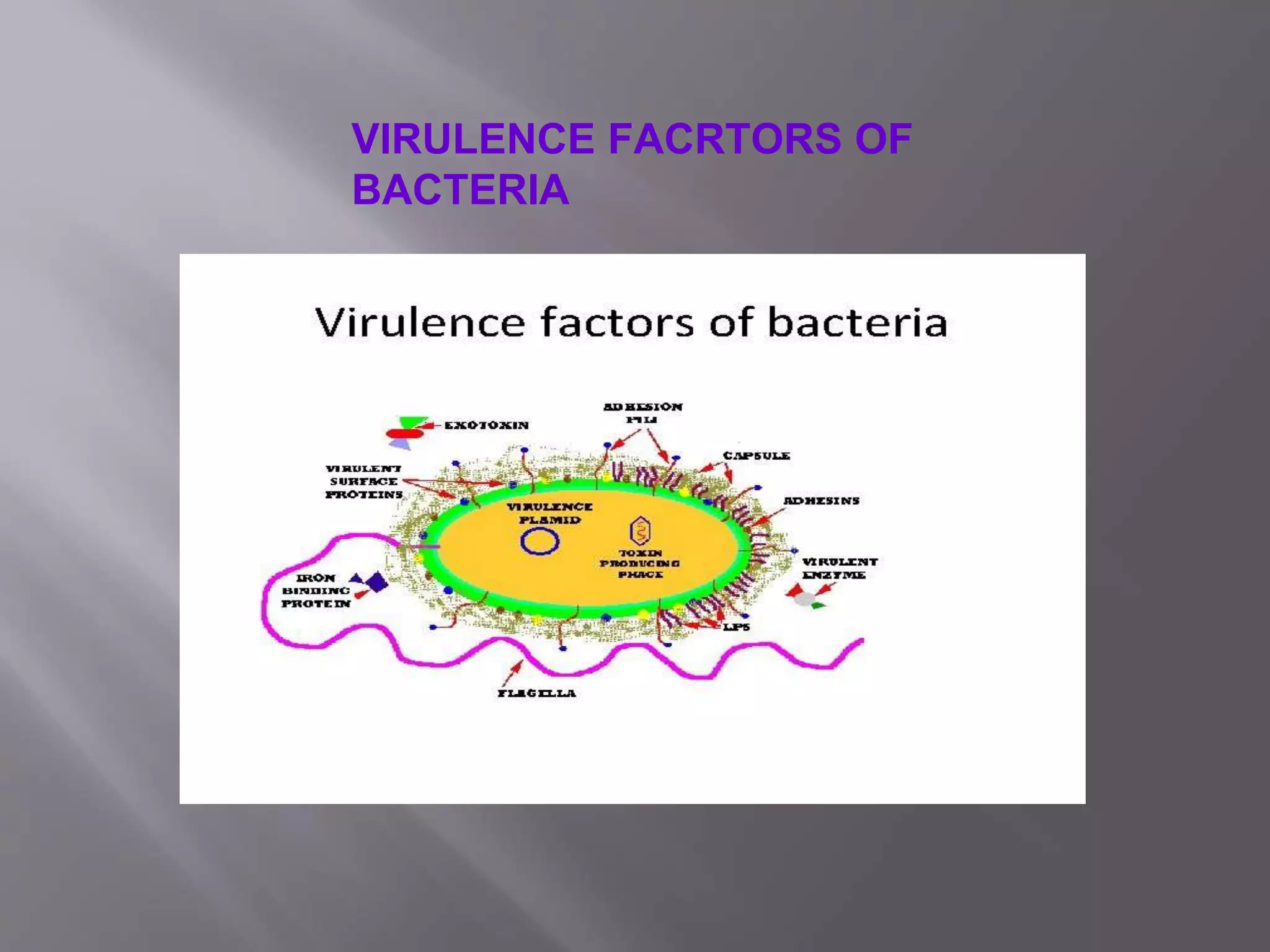
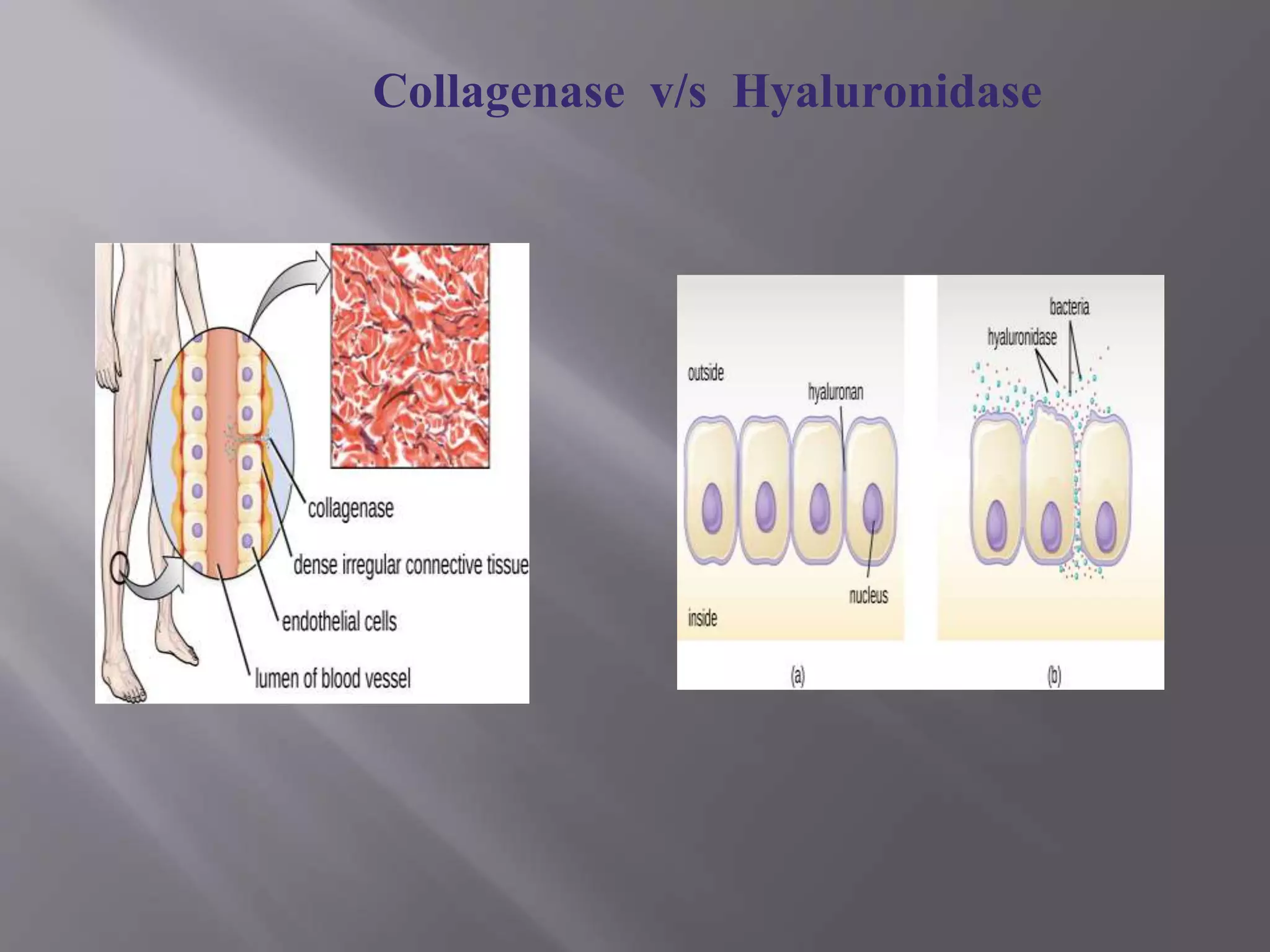
This document outlines the objectives, introduction, and conclusion of a student paper on virulence factors of bacteria. It discusses how virulence factors help bacteria colonize hosts, evade the immune system, and cause damage. The objectives are to understand how virulence factors promote colonization and damage, differentiate between endotoxins and exotoxins, and identify factors that induce autoimmune disease. Key virulence factors and their mechanisms are briefly mentioned.