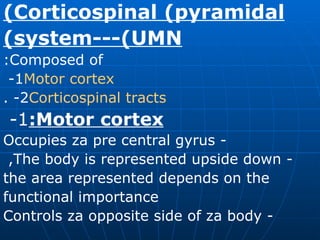
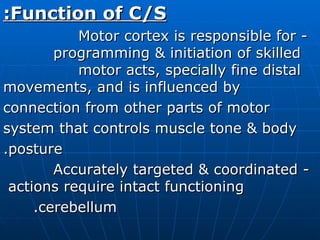
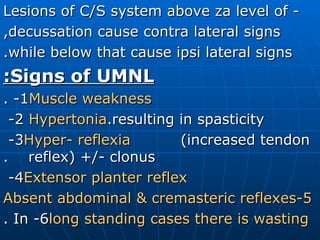
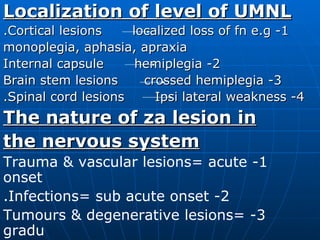
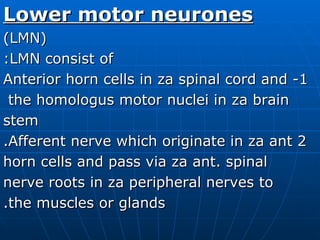
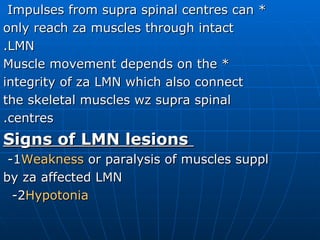
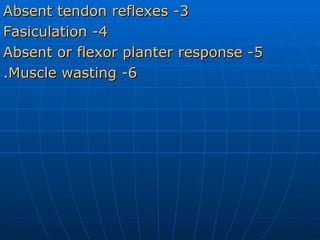
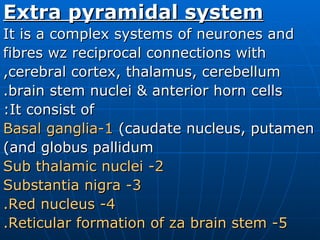
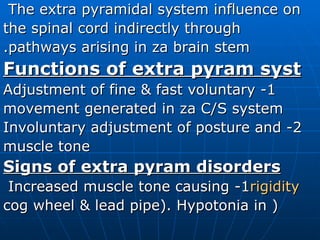
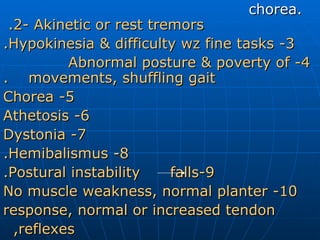
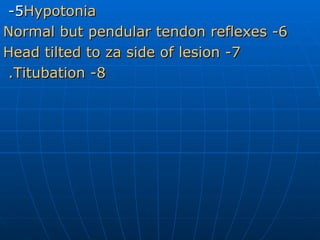
The document summarizes key aspects of neurophysiology, including the motor system, corticospinal system, lower motor neurons, extrapyramidal system, cerebellum, sensory system, reflex activities, and control of micturition. It describes the components and functions of these systems, as well as signs associated with lesions in different parts of the nervous system.