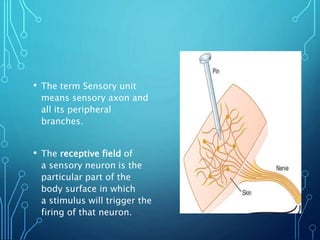
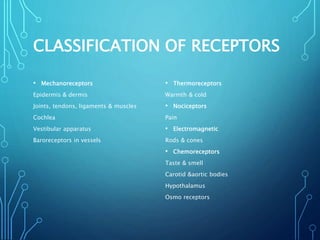
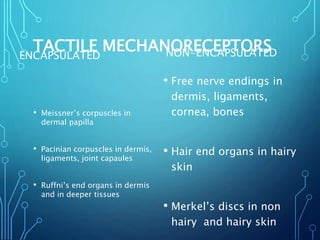
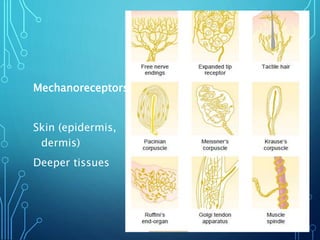
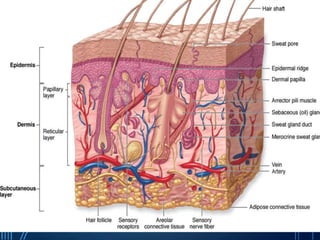
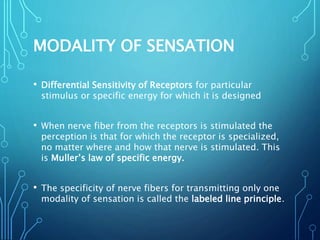
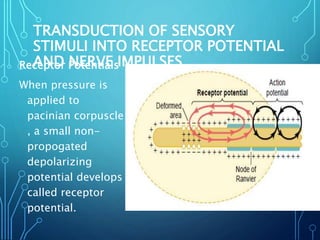
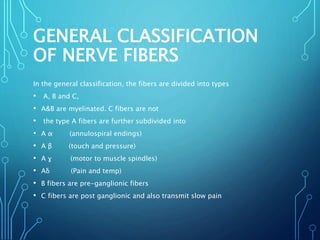
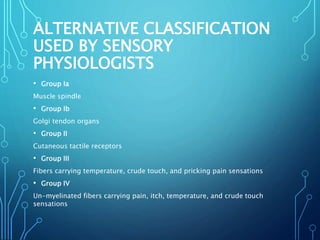
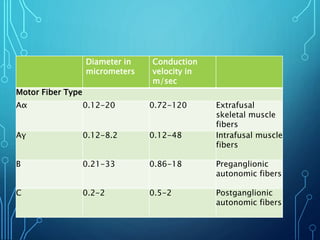
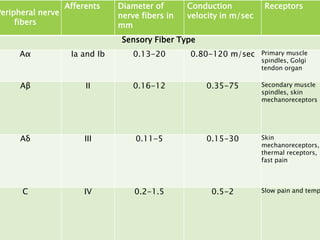
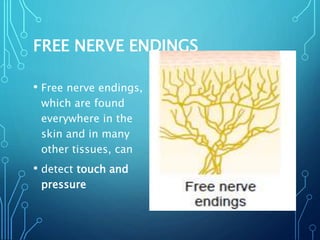
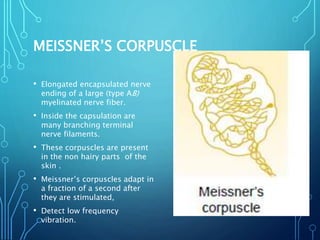
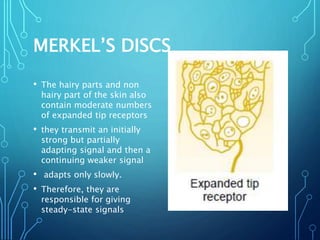
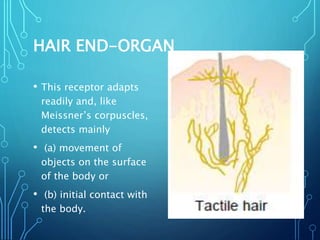
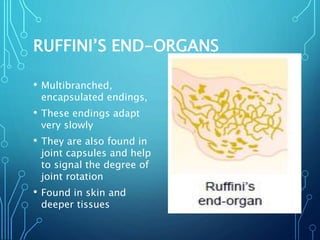
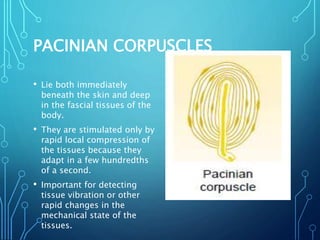
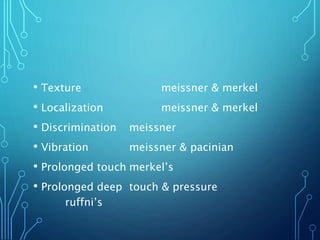
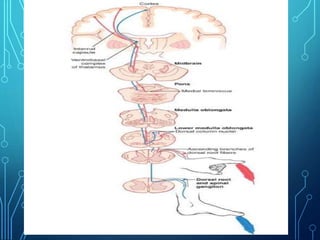
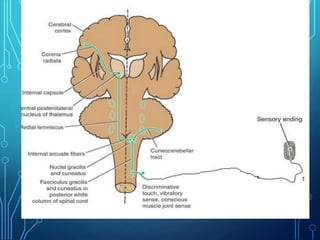
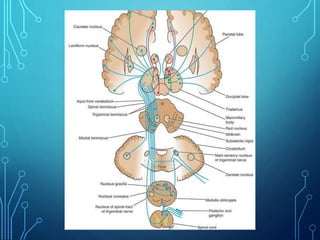
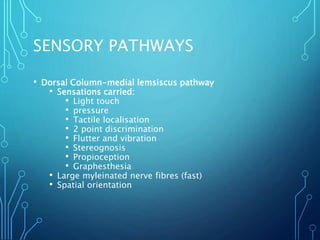
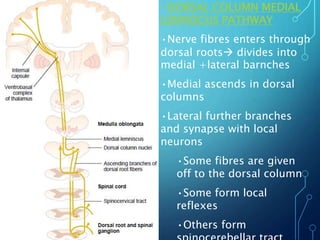
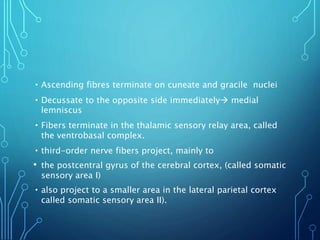
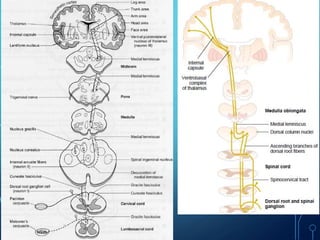
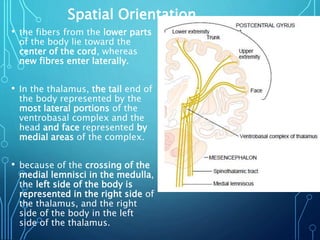
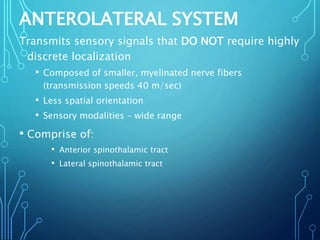
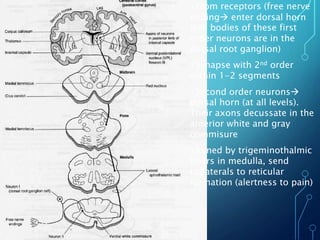
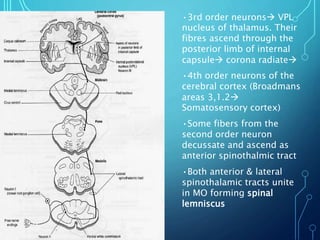
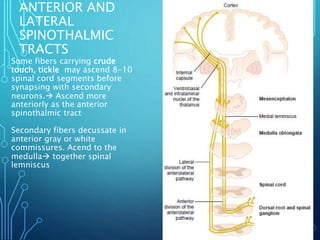
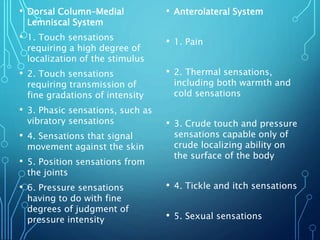
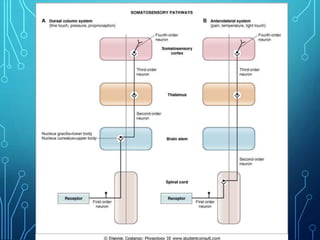
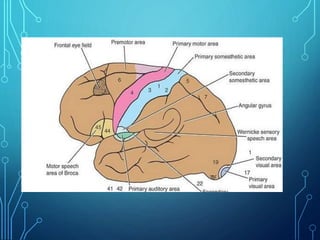
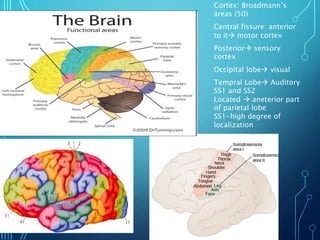
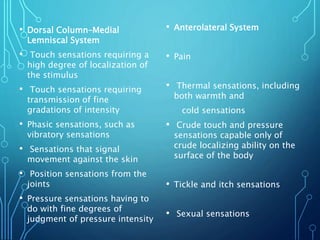
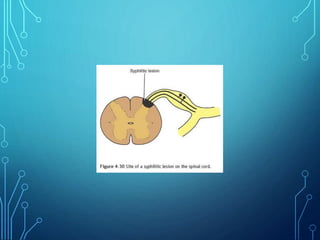
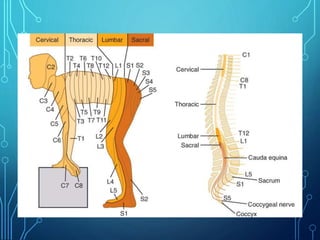
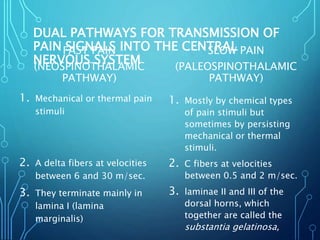
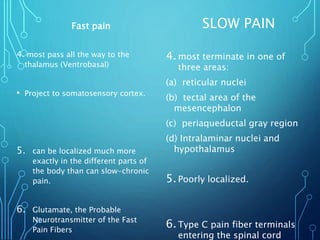
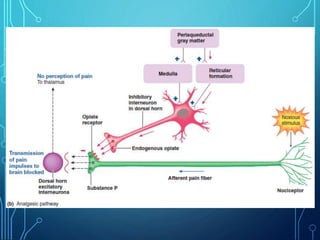
Sensory receptors detect stimuli from the internal and external environment and transmit this information to the central nervous system via sensory neurons. There are several types of sensory receptors that detect different modalities like touch, pressure, vibration, temperature, and pain. Mechanoreceptors include receptors that detect touch and pressure like free nerve endings, Meissner's corpuscles, Merkel's discs, hair receptors, Ruffini endings, and Pacinian corpuscles. Tactile signals are transmitted via myelinated A-beta fibers while pain and itch signals use small diameter C fibers. The dorsal column medial lemniscus pathway transmits tactile, proprioceptive, and vibratory signals from the periphery to the thalamus and som