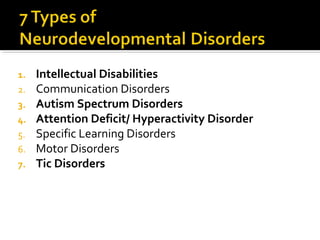
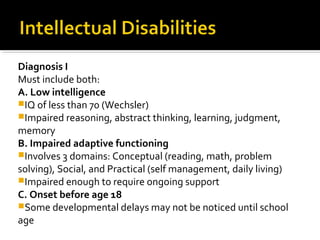
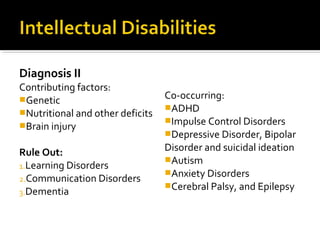
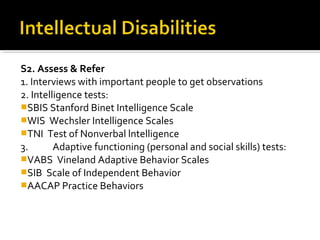
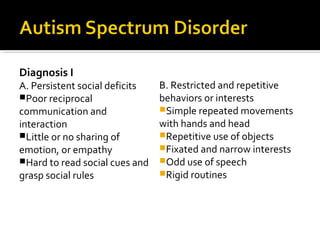
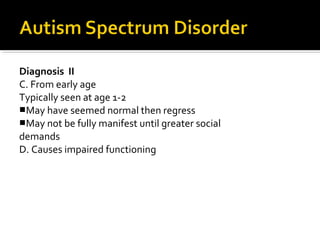
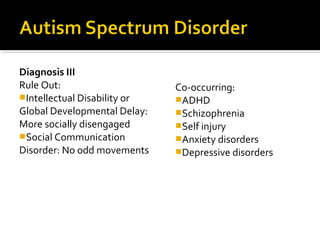
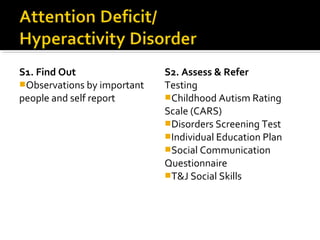
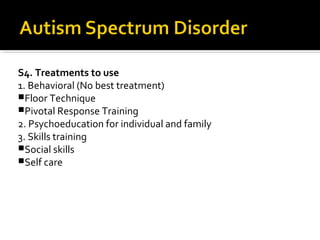
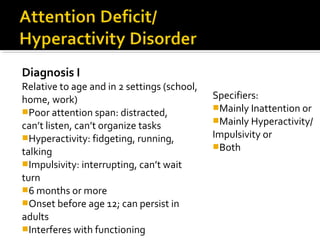
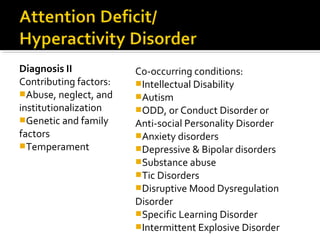
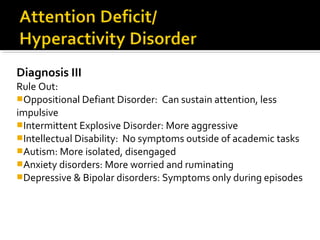
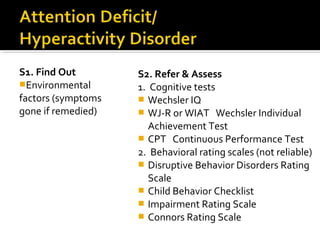
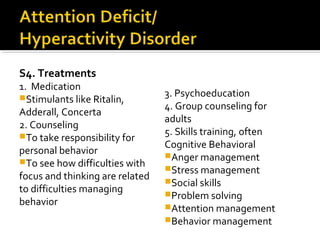
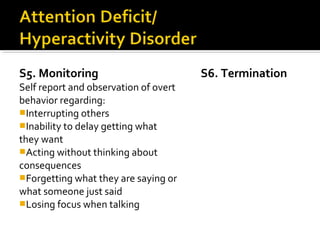
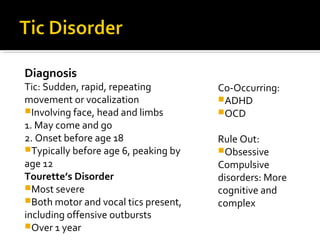
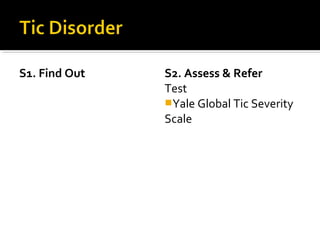
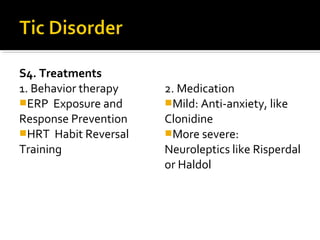
The document provides a comprehensive review of various mental disorders according to the DSM-5, including intellectual disabilities, communication disorders, autism spectrum disorders, and ADHD, detailing their diagnosis criteria, contributing factors, and co-occurring conditions. It also outlines assessment methods, referral processes, and treatment strategies for each disorder. Emphasis is placed on the importance of early identification and tailored interventions to support individuals with these mental health challenges.