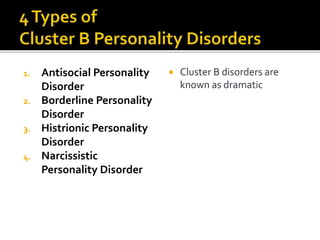
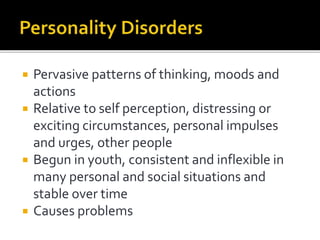
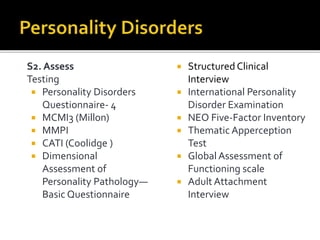
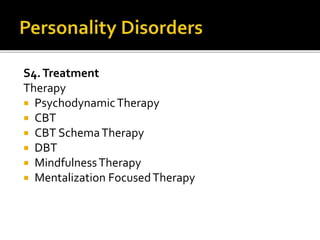
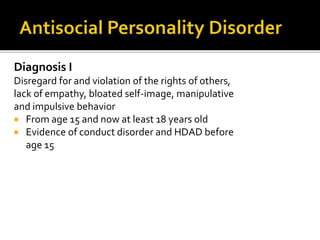
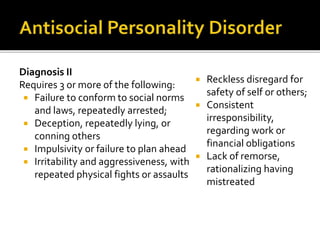
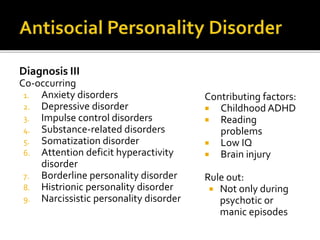
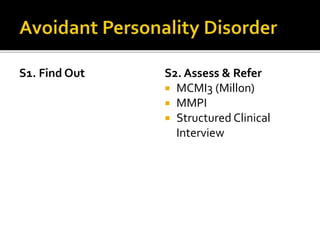
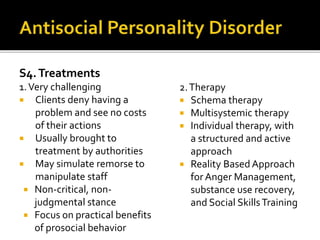
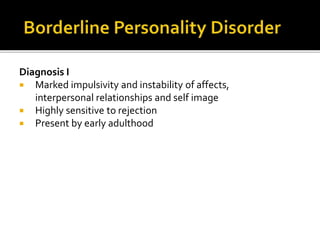
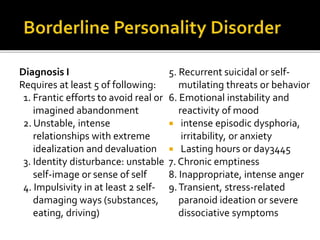
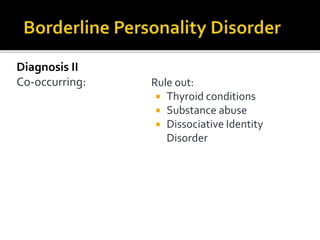
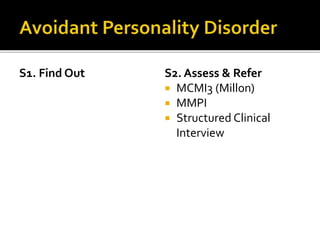
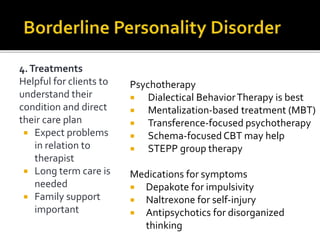
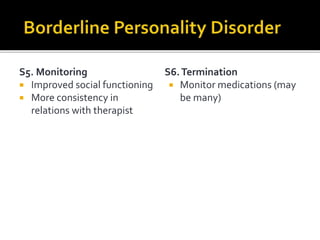
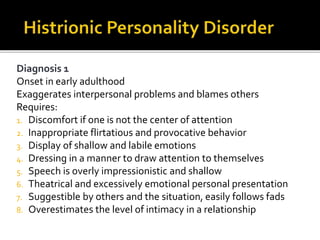
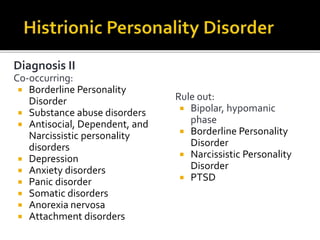
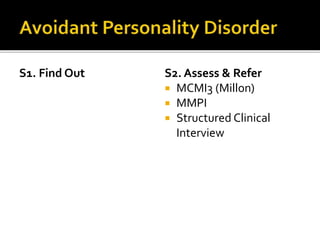
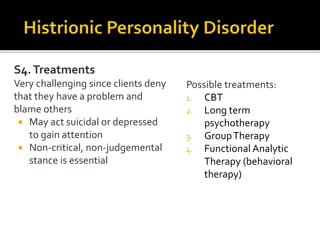
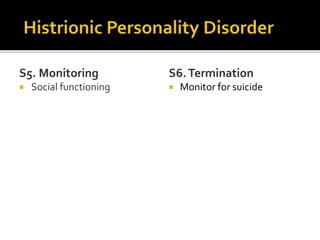
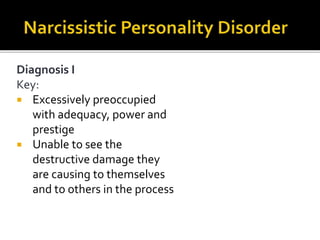
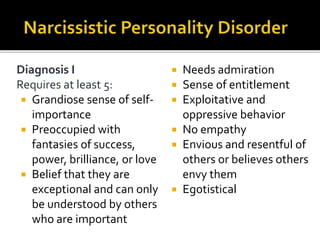
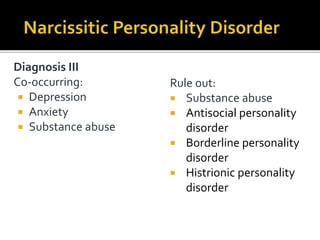
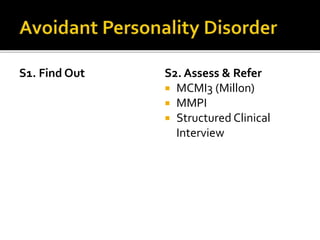
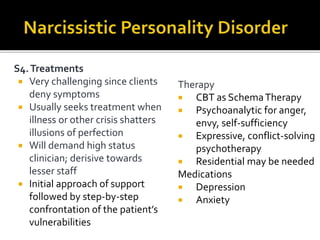
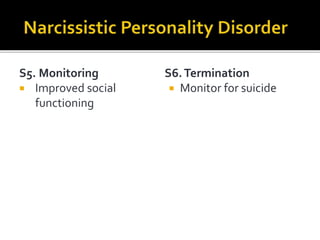
The document provides a comprehensive review of various personality disorders from the DSM-5, focusing on cluster B disorders such as antisocial, borderline, histrionic, and narcissistic personality disorders. It outlines diagnostic criteria, co-occurring disorders, contributing factors, assessment methods, and treatments including psychotherapies and medications for managing symptoms. The text emphasizes the challenges in treating these disorders due to patient denial of problems and manipulative behaviors, highlighting the importance of personalized therapeutic approaches.