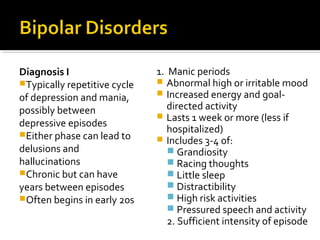
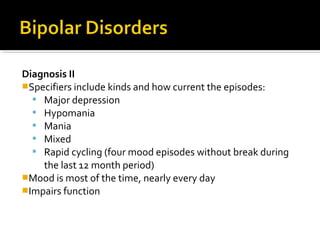
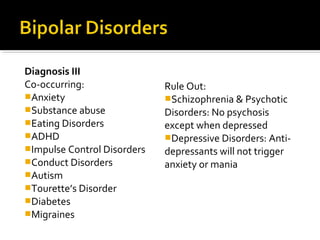
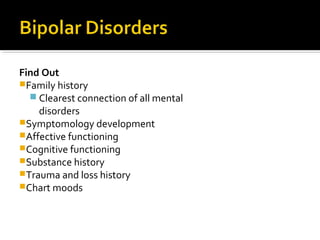
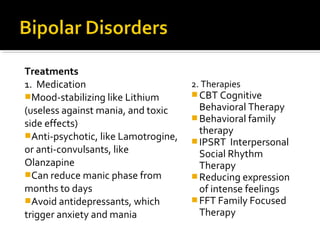
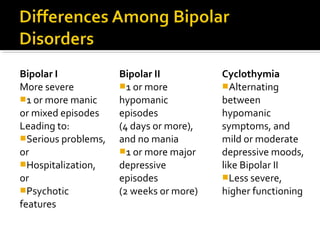
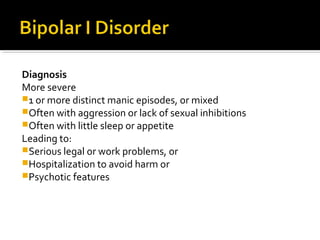
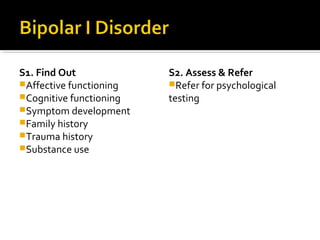
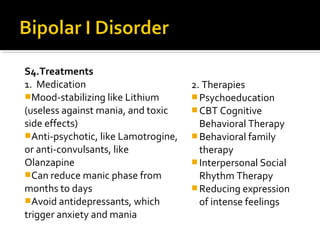
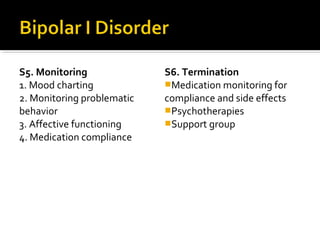
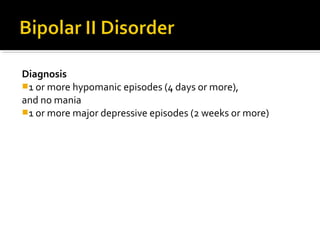
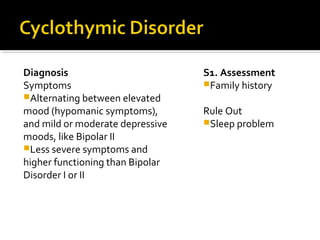
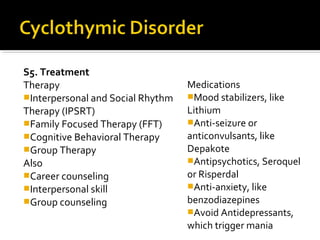
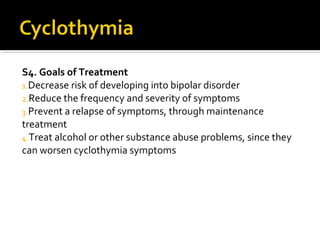
The document provides an overview of various DSM-5 mental disorders relevant for the NCMHCE study, focusing on bipolar disorders, including Bipolar I, Bipolar II, and cyclothymic disorder. It details symptoms, diagnostic criteria, co-occurring conditions, treatment options such as medications and therapy, and monitoring strategies. The document emphasizes the importance of family history and assessment in treatment planning and aims to decrease risks and improve patient outcomes.