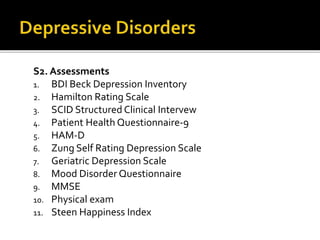
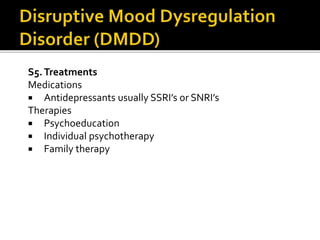
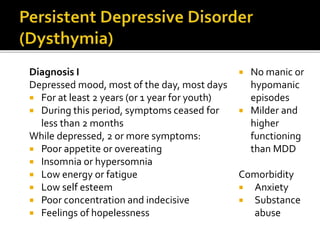
The document provides a comprehensive review of various mental disorders as classified in DSM-5, including types of depressive disorders and disruptive mood conditions. It details assessment tools, pharmacological treatments like SSRIs and therapies such as cognitive behavioral therapy, as well as diagnostic criteria for these disorders. Additional information on comorbidities, treatment evaluations, and specific symptoms for conditions like premenstrual dysphoric disorder and substance-induced depression is also included.