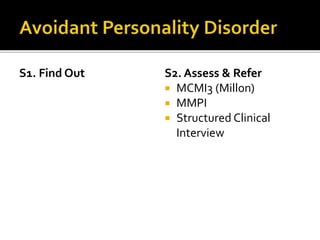
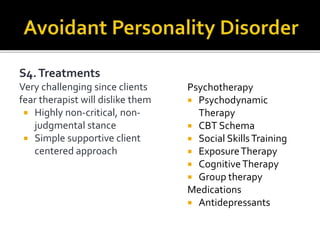
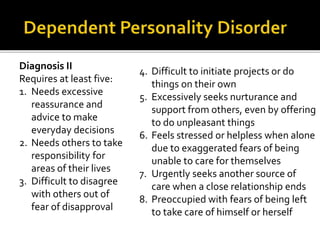
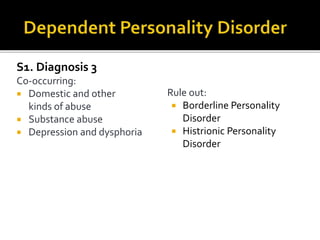
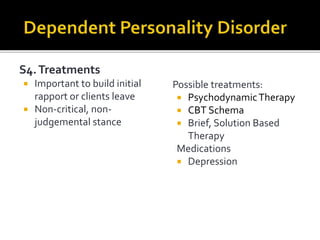
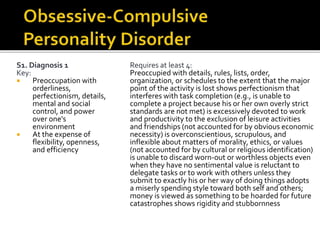
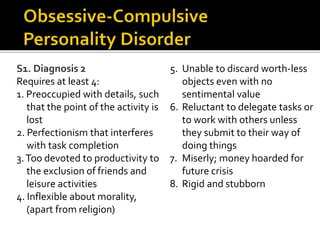
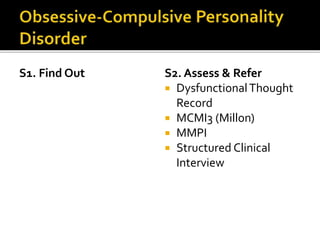
The document reviews three types of personality disorders: avoidant, dependent, and obsessive-compulsive, detailing their diagnostic criteria, assessment methods, and treatment options. It emphasizes the need for a non-judgmental therapeutic approach, highlighting challenges in treatment due to clients' fears of rejection and the significance of monitoring social functioning and autonomy. Specific assessments and treatments, including various psychotherapies and medications, are outlined for each disorder to facilitate effective treatment.