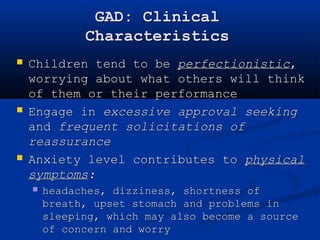
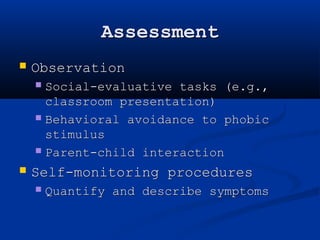
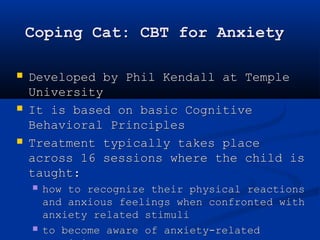
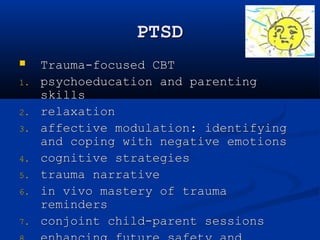
The document discusses childhood anxiety disorders, highlighting characteristics such as excessive and debilitating anxiety, developmental considerations, and symptoms that manifest differently in children compared to adults. It categorizes various forms of anxiety, including separation anxiety disorder, social phobia, generalized anxiety disorder, and obsessive-compulsive disorder, providing DSM criteria and case examples for each. Additionally, it explores the prevalence, etiology, and assessment methods for these anxiety disorders in children.