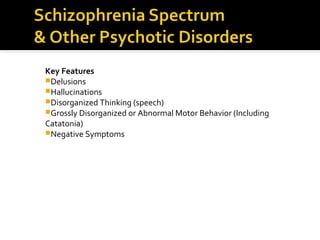
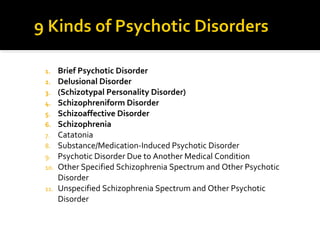
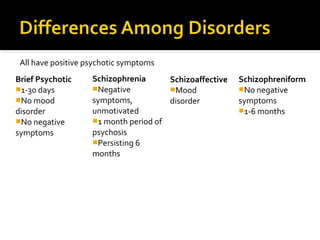
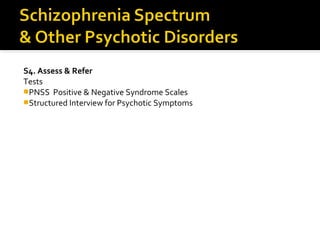
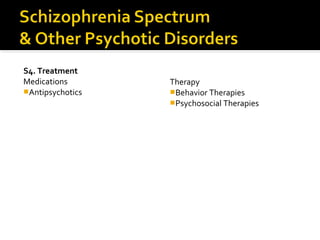
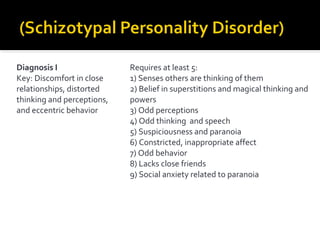
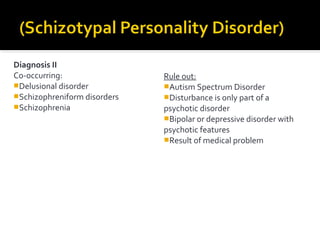
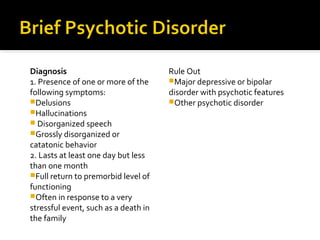
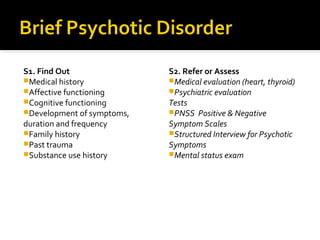
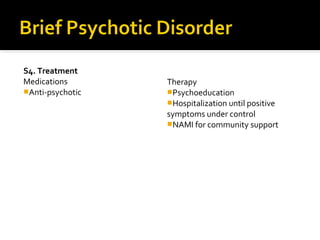
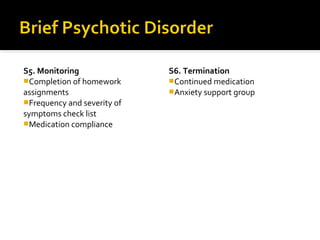
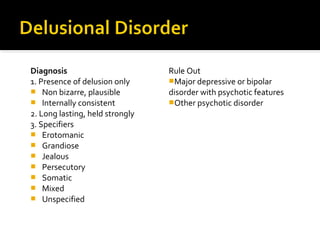
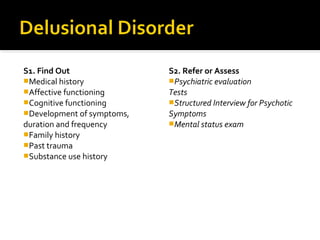
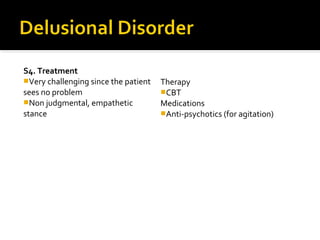
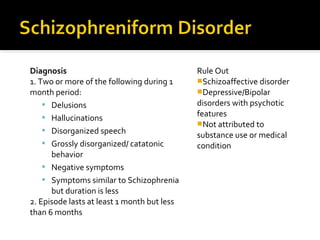
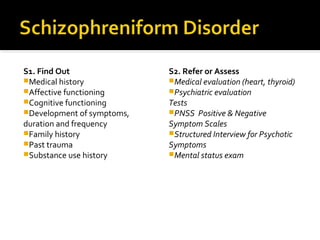
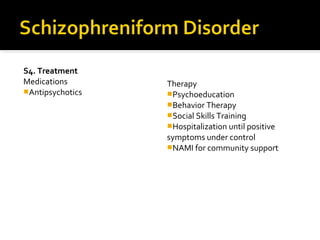
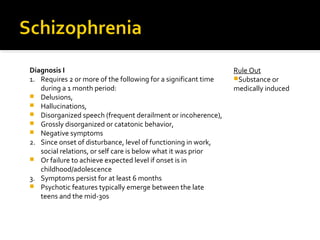
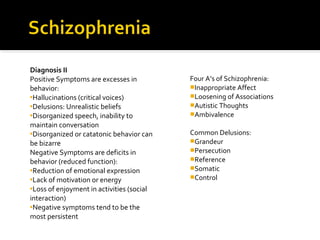
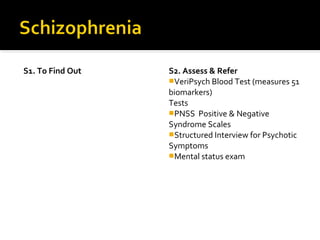
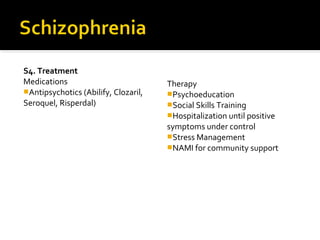
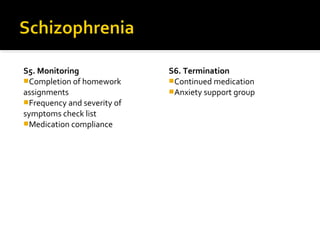
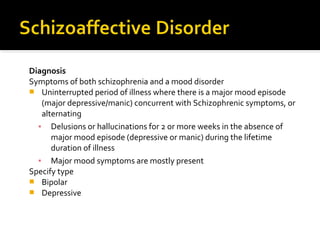
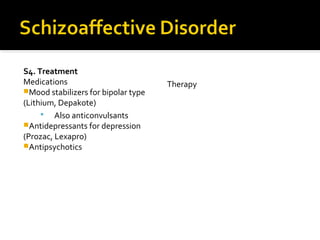
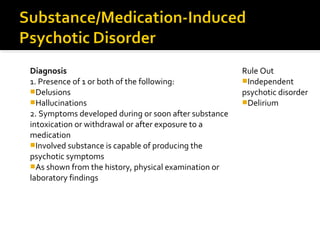
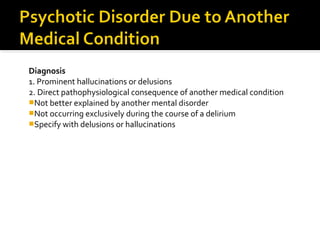
The document provides an overview of schizophrenia spectrum and other psychotic disorders according to the DSM-5. It discusses key features of psychotic disorders including delusions, hallucinations, and disorganized thinking. It then summarizes several psychotic disorders - brief psychotic disorder, delusional disorder, schizophrenia, schizoaffective disorder, substance/medication-induced psychotic disorder, and psychotic disorder due to another medical condition. For each disorder, it outlines diagnostic criteria and treatment approaches including medications, therapy, and monitoring.