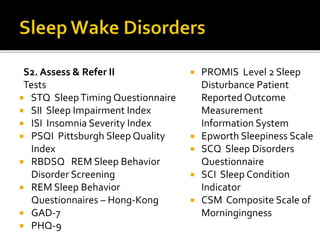
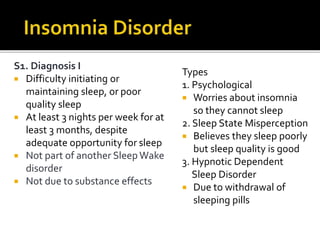
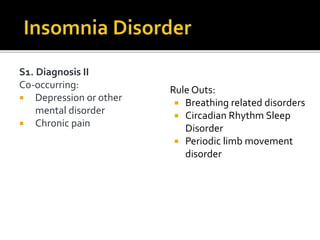
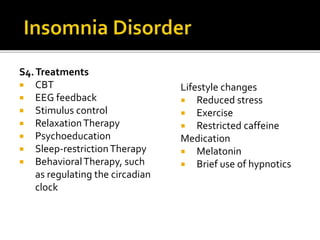
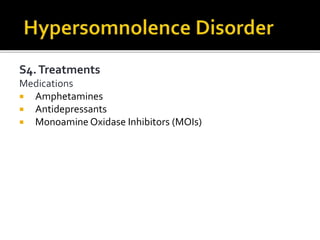
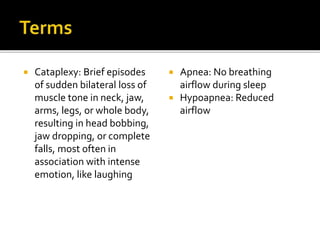
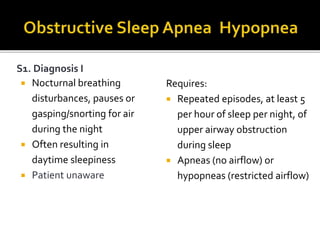
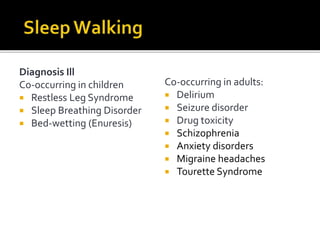
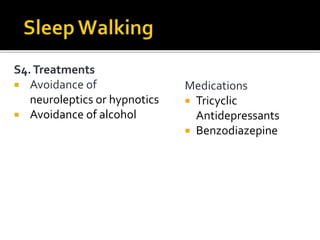
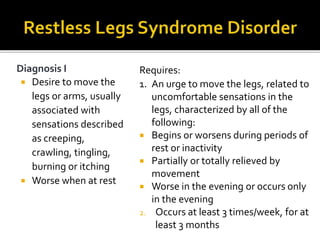
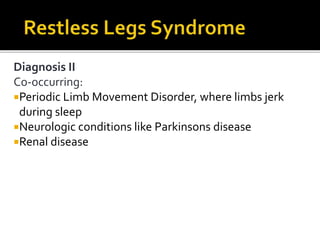
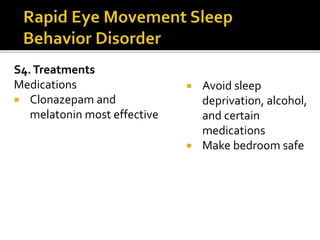
The document reviews several sleep disorders according to the DSM-5 including insomnia disorder, hypersomnolence disorder, narcolepsy, breathing-related sleep disorders, circadian rhythm sleep-wake disorders, non-REM sleep arousal disorders, parasomnias, nightmare disorder, and restless legs syndrome. It discusses the diagnostic criteria, comorbidities, assessments, and treatment options for each disorder in detail across several sections.