Myopathies are primary muscle diseases that cause chronic muscle weakness. There are three broad groups: hereditary myopathies like muscular dystrophies, inflammatory myopathies such as polymyositis and dermatomyositis, and toxic myopathies caused by things like drugs and thyroid disorders.
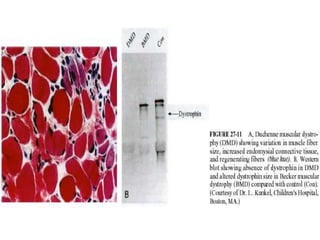
Duchenne muscular dystrophy is the most common and serious hereditary myopathy. It is an X-linked recessive disorder caused by a lack of the dystrophin protein, leading to muscle degeneration. Boys experience progressive muscle weakness starting in early childhood and death usually occurs in late teens.
Polymyositis and dermatomyositis are inflammatory myopathies characterized by muscle pain, weakness