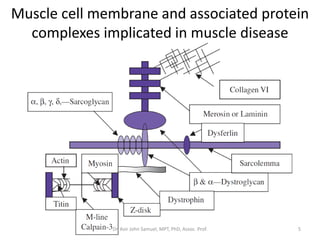
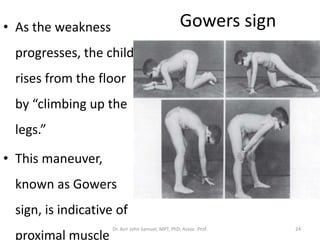
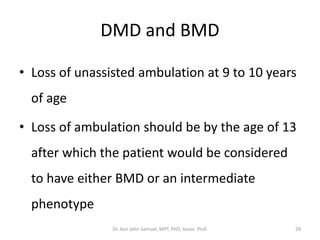
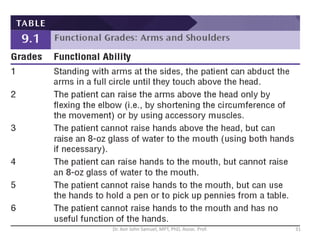
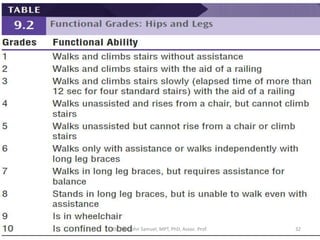
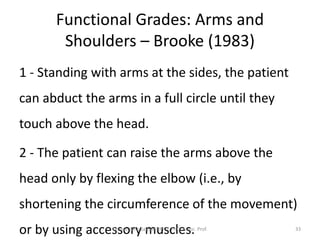
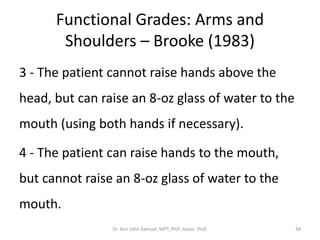
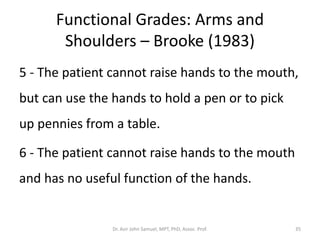
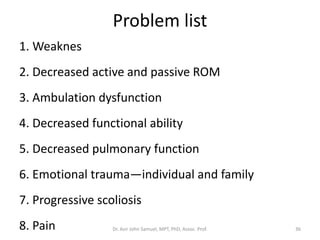
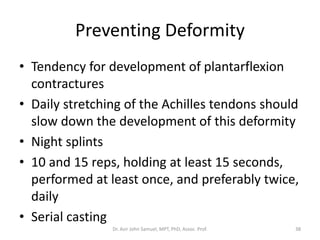
The document discusses muscular dystrophy, focusing on Duchenne muscular dystrophy (DMD), which is a genetically determined muscular disease characterized by progressive muscle degeneration and weakness, primarily impacting males. DMD is associated with the deficiency of dystrophin, leading to a variety of symptoms including muscle weakness, contractures, and decreased pulmonary function. The document also outlines diagnostic approaches, clinical presentations, functional assessments, and the role of physical therapy interventions to manage the disease.