The document discusses HIV infection and encephalitis. Some key points:
- HIV is a retrovirus that causes AIDS and can affect the nervous system directly or indirectly through opportunistic infections.
- Neurological features develop in 80% of infected individuals, manifesting as effects of HIV or infections/tumors due to immunodeficiency.
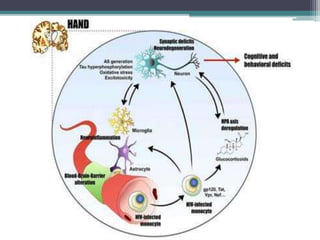
- HIV encephalitis refers to cognitive impairment from cerebral HIV infection and does not include opportunistic infections from immunodeficiency.
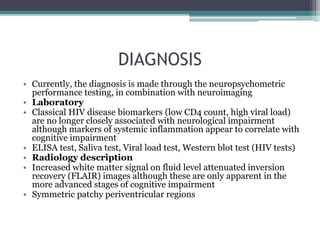
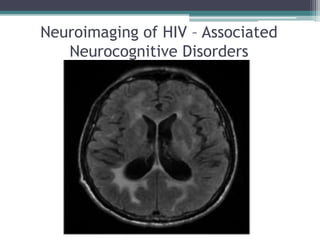
- Symptoms of HIV encephalitis include decreased cognition, psychomotor slowing, and motor symptoms like gait instability. Diagnosis involves neuropsychological testing and neuroimaging. Treatment includes antiretroviral therapy and