This document discusses various muscle disorders including:
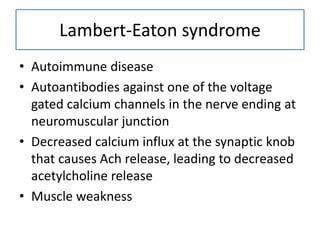
1) Diseases affecting the neuromuscular junction such as myasthenia gravis and Lambert-Eaton syndrome.
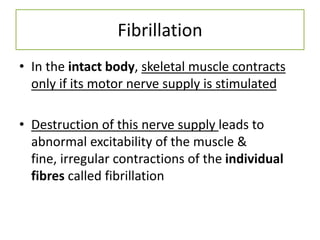
2) Effects of denervation of muscle including fibrillation, fasciculation, muscle atrophy, and denervation hypersensitivity.
3) Muscle dystrophies which are degenerative diseases that cause progressive muscle weakness. The most common type is Duchenne muscular dystrophy which is often fatal by age 30.