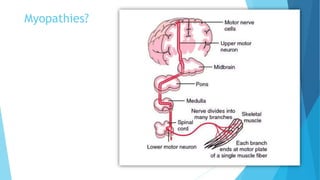
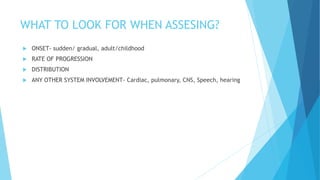
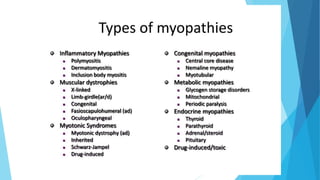
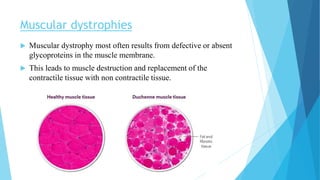
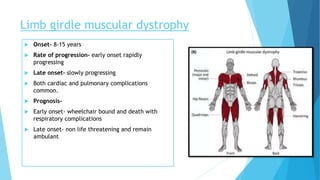
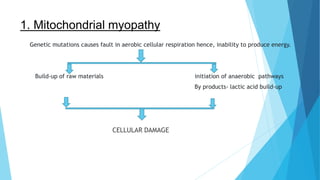
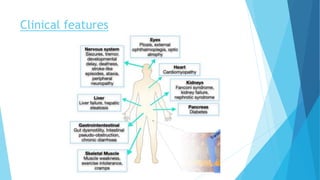
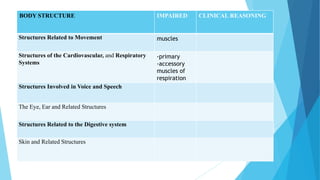
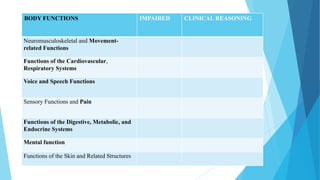
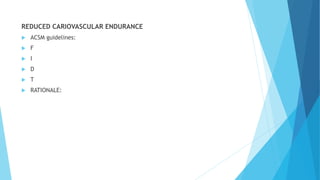
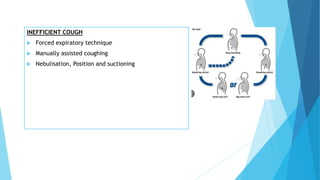
The document discusses myopathies, including their classification, clinical features, and management strategies. It outlines types such as muscular dystrophies and metabolic myopathies, detailing onset, progression, prognosis, and common complications. Management emphasizes exercise, mobility aids, dietary changes, and respiratory support to address associated challenges.