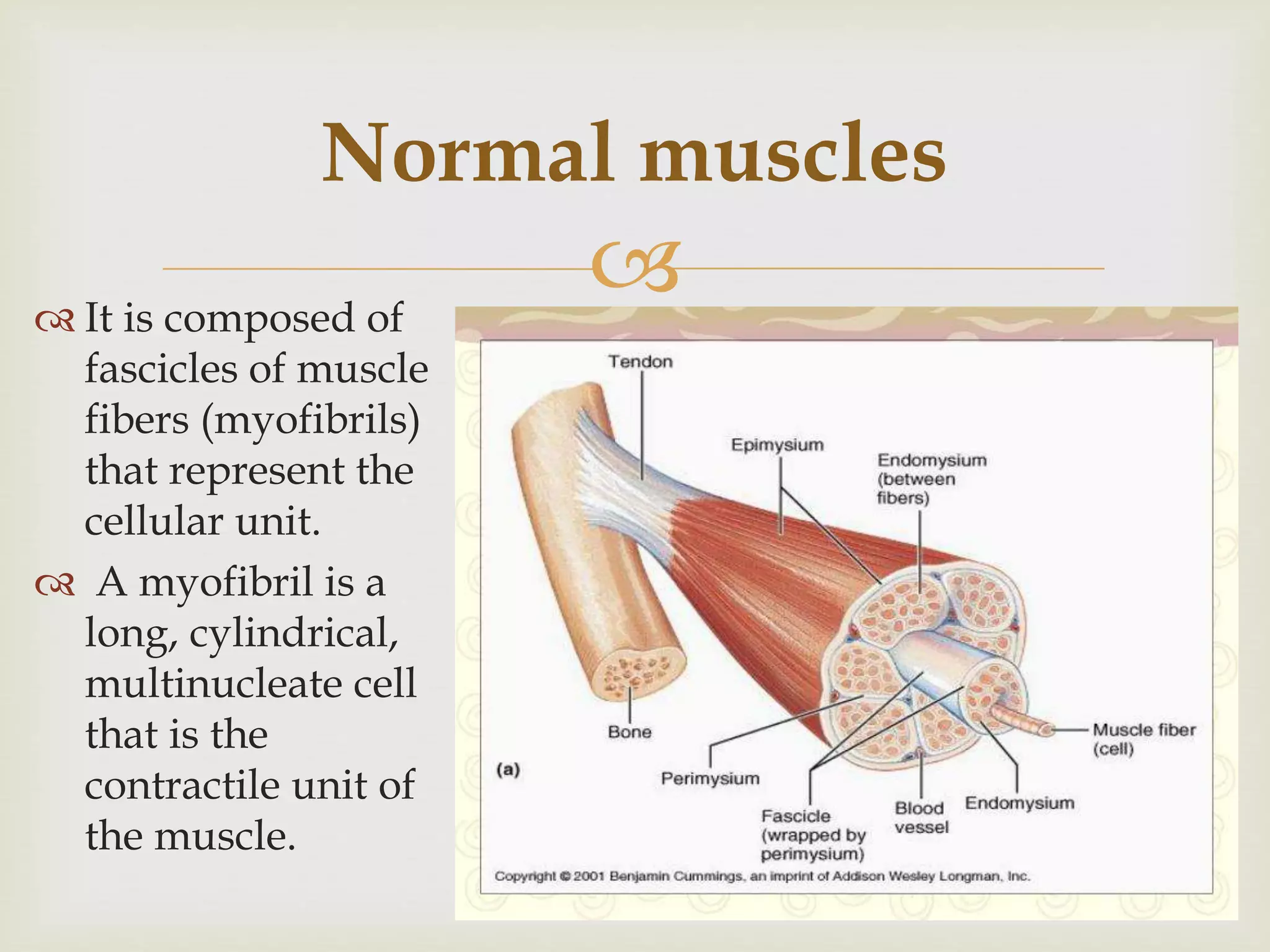
The document discusses various muscle disorders, including myopathies, muscular atrophy, muscular dystrophy, and myositis, explaining their causes, symptoms, and diagnostic approaches. It highlights Duchenne muscular dystrophy as a common childhood condition and describes the autoimmune nature of myasthenia gravis, a disorder characterized by muscle weakness due to neuromuscular transmission failure. Diagnostic methods and treatment options for these conditions are also outlined.