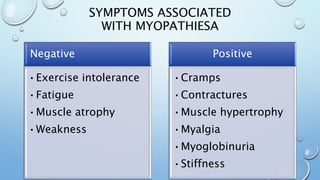
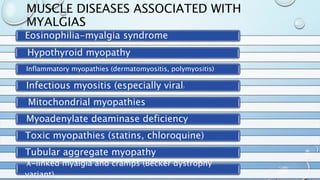
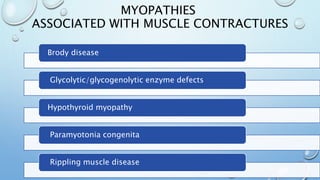
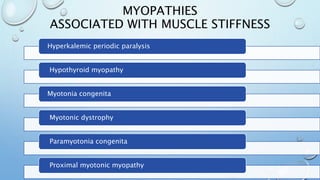
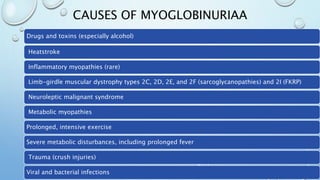
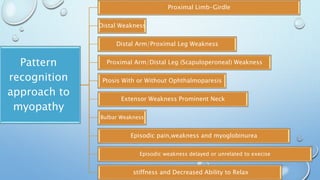
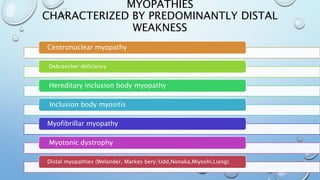
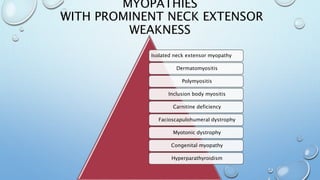
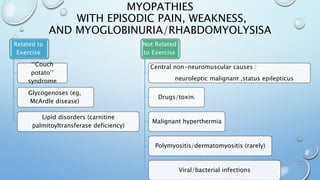
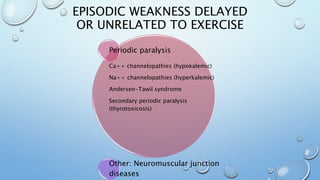
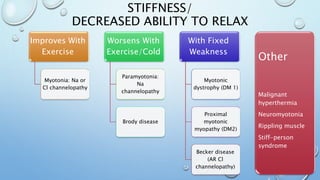
This document discusses the diagnostic approach to myopathies. It emphasizes that obtaining a comprehensive medical history is very important for diagnosis. The history should clarify the patient's symptoms, any family history of muscle disorders, precipitating factors, associated conditions, and distribution of weakness. Different myopathies are characterized by features like muscle pain, stiffness, weakness, or damage shown by myoglobinuria. Specific myopathies can be suggested based on the pattern of muscle involvement, such as proximal or distal weakness. The document provides tables matching myopathies to various clinical features to guide diagnosis.