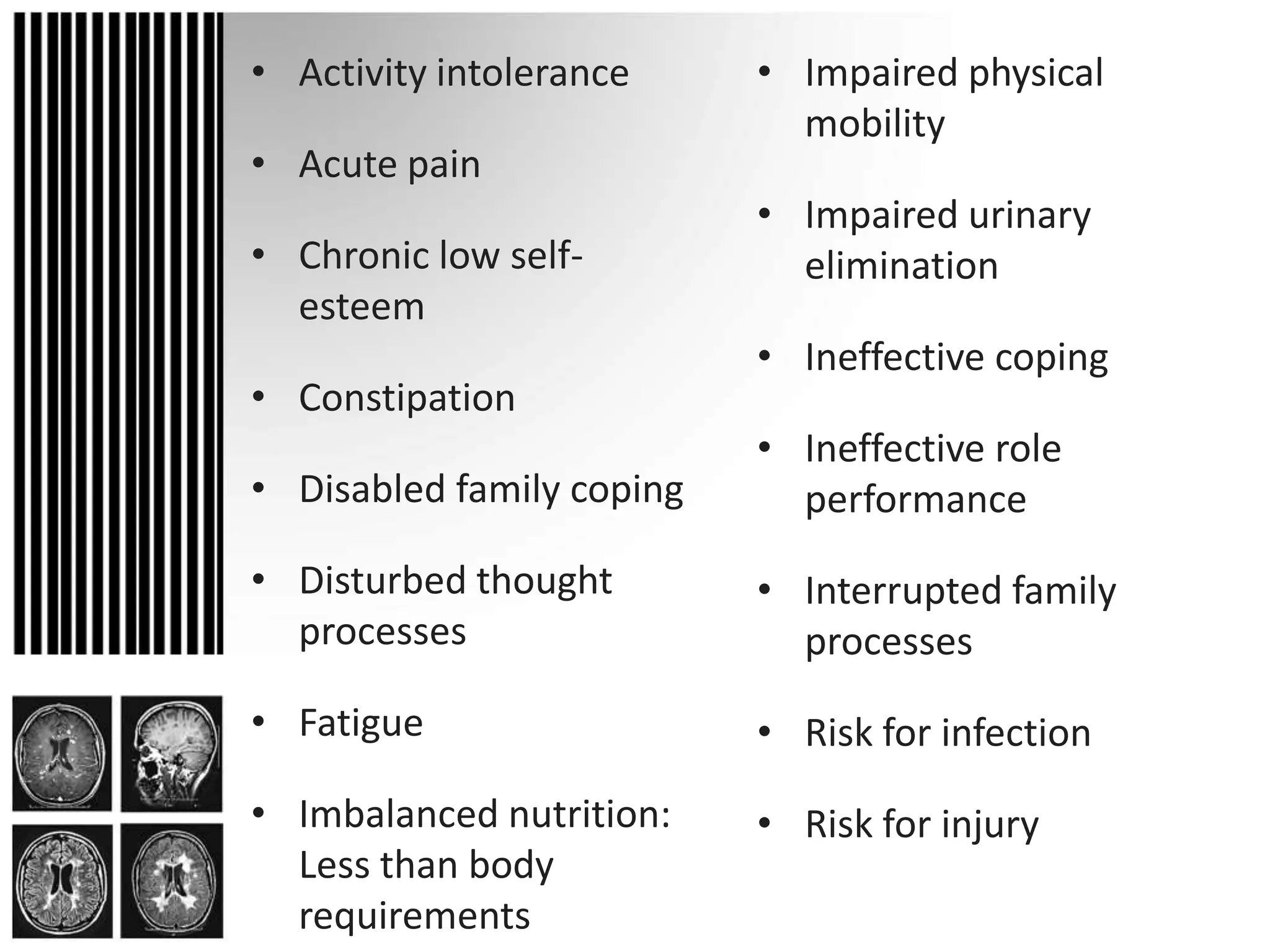
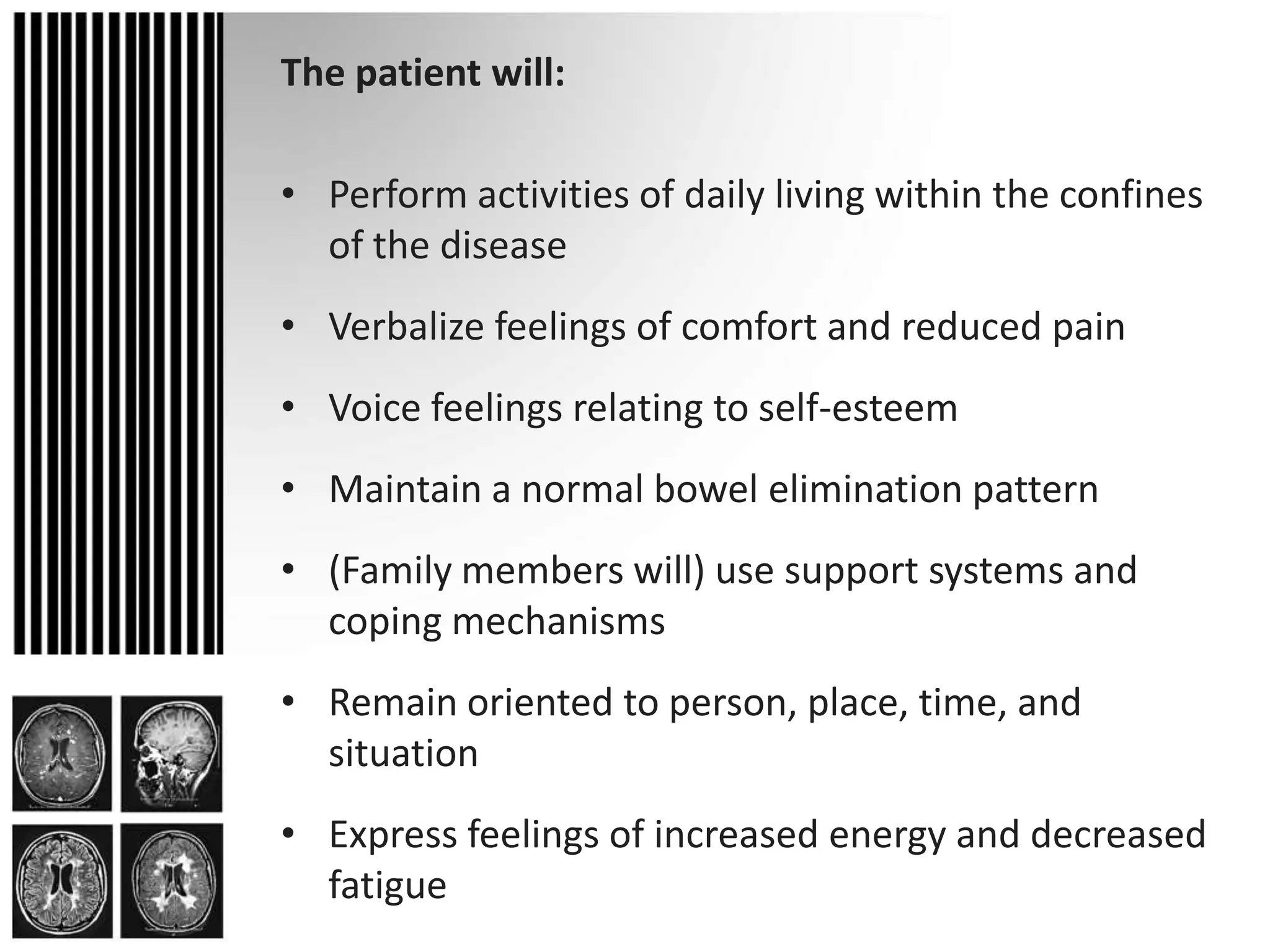
Multiple sclerosis (MS) is a chronic, progressive neurological disease involving demyelination of the central nervous system. It is characterized by exacerbations and remissions of symptoms that vary depending on the location of lesions in the brain and spinal cord. Common clinical manifestations include fatigue, weakness, sensory disturbances, and impaired coordination. While the exact cause is unknown, it is thought to involve an autoimmune response. Treatment focuses on managing relapses, reducing disease progression, and alleviating symptoms. Nursing care emphasizes education, rehabilitation, and supportive measures to help patients maintain optimal functioning.