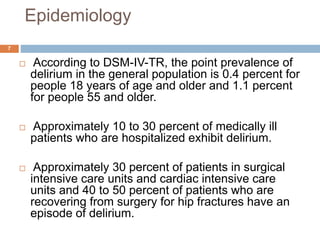
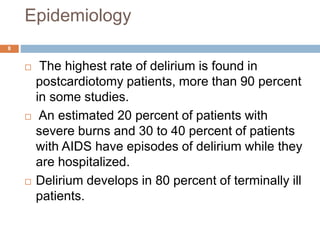
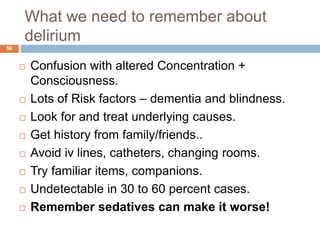
This document provides an overview of delirium, including its definition, history, characteristics, epidemiology, risk factors, causes, pathophysiology, clinical features, diagnosis, differential diagnosis, course and prognosis, and treatment. Some key points covered include:
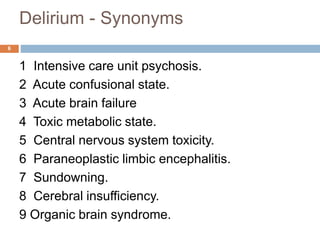
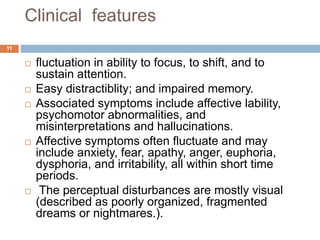
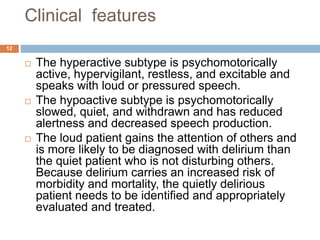
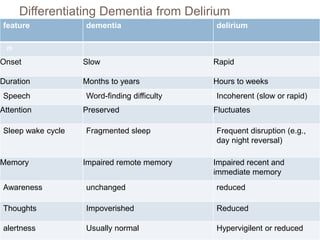
- Delirium is defined as an acute impairment of attention, consciousness, and cognition that fluctuates in severity.
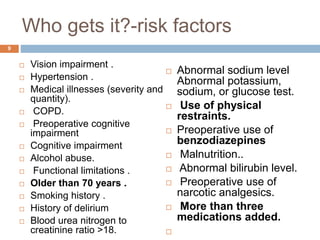
- Risk factors include older age, medical illnesses, cognitive impairment, and polypharmacy.
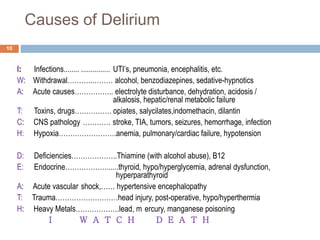
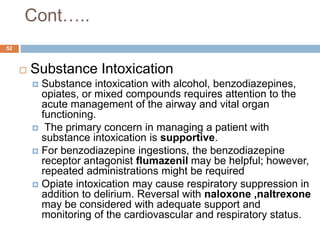
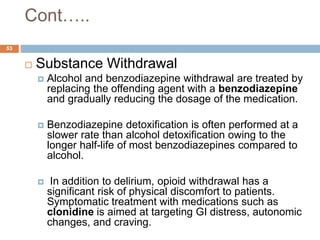
- Causes include infections, withdrawal, toxins/drugs, hypoxia, and metabolic disturbances.
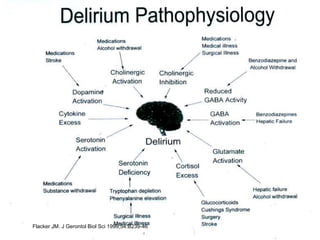
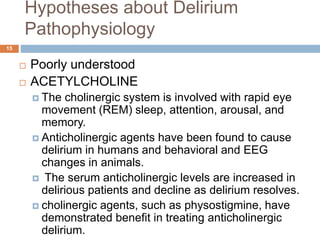
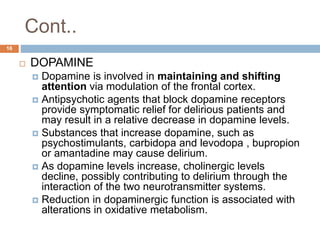
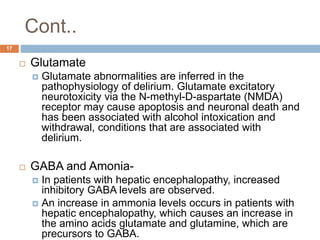
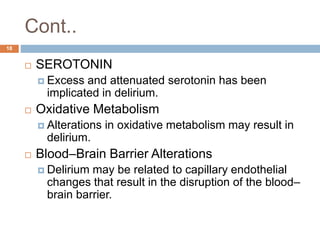
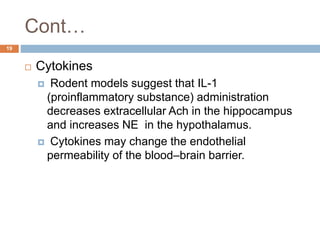
- The pathophysiology is not fully understood but may involve neurotransmitter imbalances and blood-brain barrier disruption.
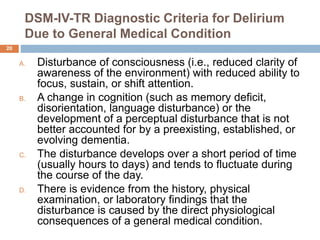
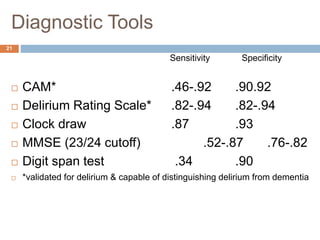
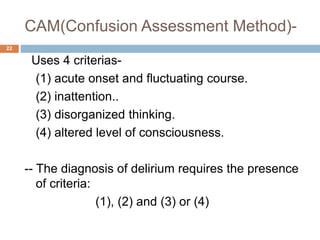
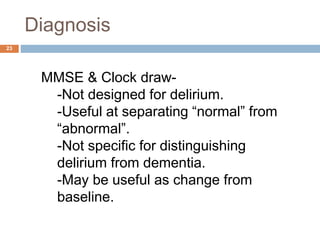
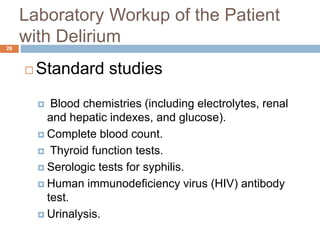
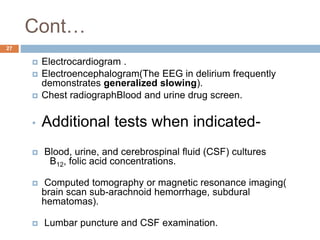
- Diagnosis involves