This document provides an overview of burn injuries including:
1. The pathophysiology of burns including fluid shifts, systemic changes, and the hypermetabolic response.
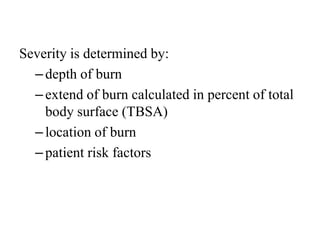
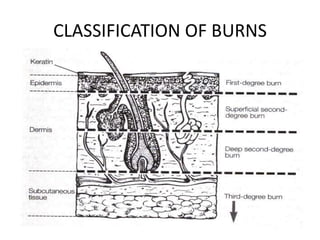
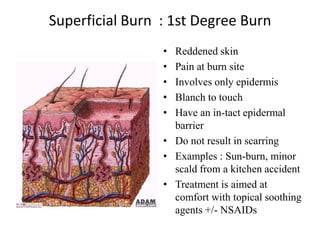
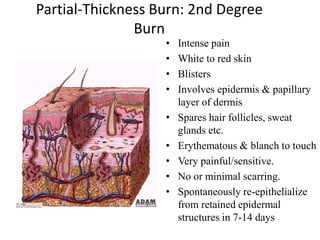
2. Classification of burns by depth and severity. Thermal burns can cause damage from coagulation to hyperemia.
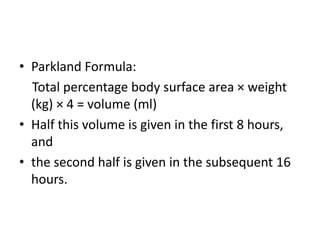
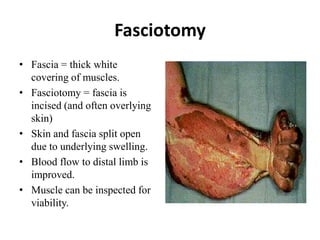
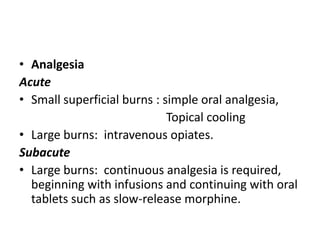
3. Management of burns focuses on airway control, fluid resuscitation using formulas like Parkland, and wound care including escharotomy, fasciotomy, and debridement.