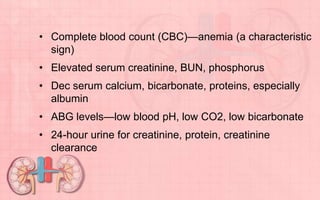
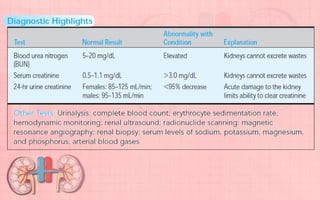
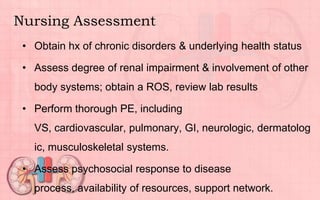
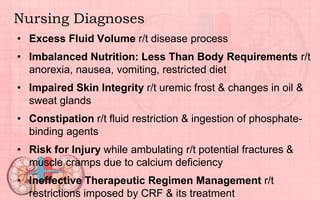
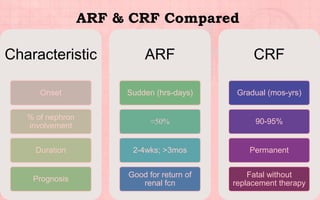
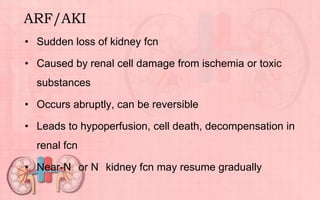
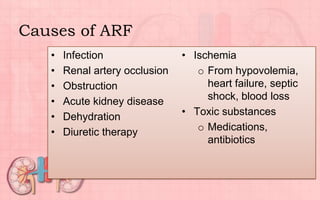
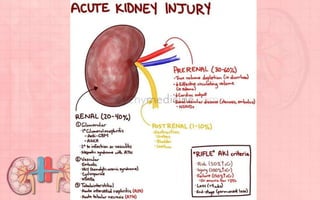
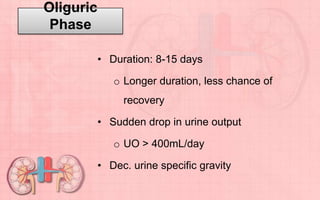
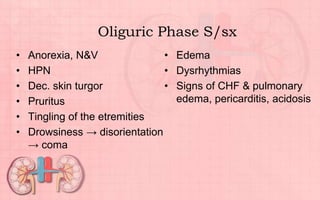
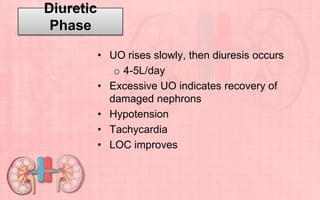
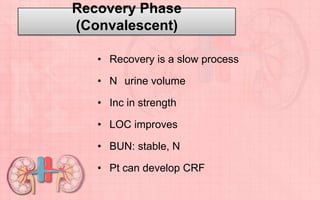
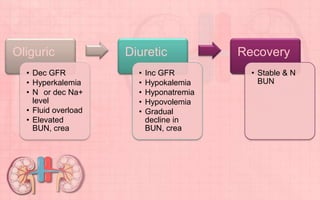
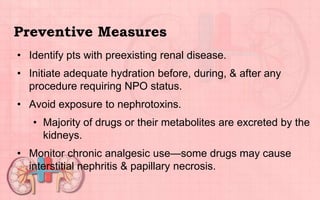
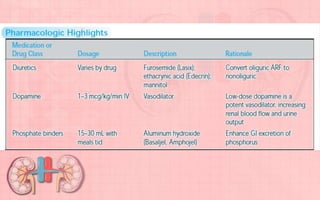
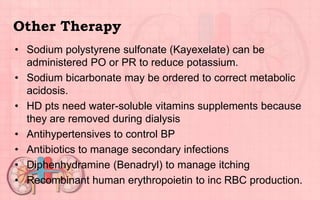
Acute renal failure (ARF) is a sudden loss of kidney function that can be reversible. It is caused by renal cell damage from ischemia or toxic substances. ARF progresses through oliguric, diuretic, and recovery phases. Nursing management focuses on fluid and electrolyte balance, preventing infections, maintaining nutrition, and preserving neurologic function. Dialysis may be needed to correct electrolyte imbalances or other complications of ARF.



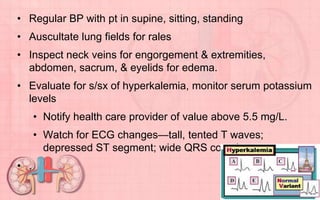
![• Administer sodium bicarbonate or glucose & insulin to shift
potassium into the cells.
• Administer cation exchange resin (sodium polystyrene
sulfonate [Kayexalate]) PO/PR to provide more prolonged
correction of elevated potassium.
• Watch for cardiac arrhythmia & heart failure from
hyperkalemia, electrolyte imbalance, or fluid overload.
• Resuscitation equipment on hand in case of cardiac arrest.
• Instruct on importance of following prescribed diet; avoid
foods high in potassium.](https://image.slidesharecdn.com/understandingrenalfailure-130814021027-phpapp02/85/Understanding-renal-failure-37-320.jpg)