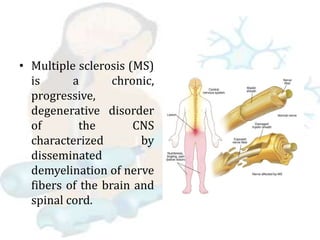
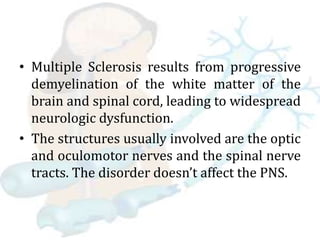
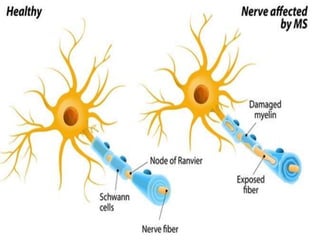
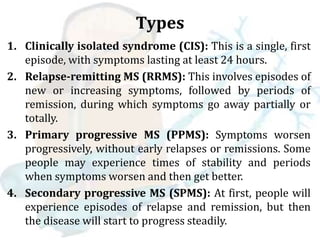
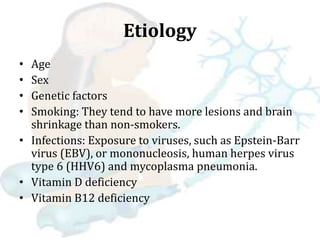
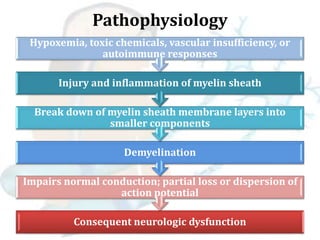
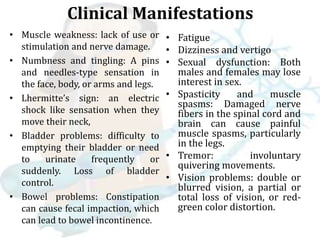
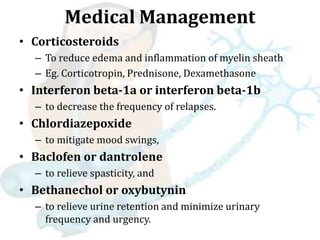
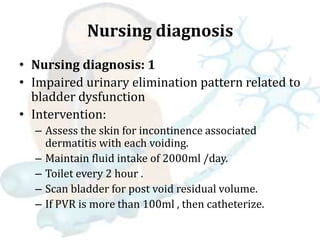
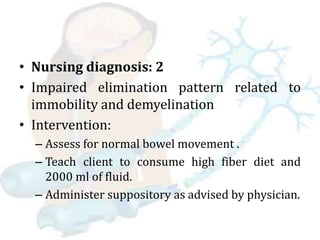
Multiple sclerosis is a chronic disease that causes demyelination of nerve fibers in the brain and spinal cord. It results in widespread neurological dysfunction. There are four main types of MS including clinically isolated syndrome, relapse-remitting MS, primary progressive MS, and secondary progressive MS. Risk factors include age, sex, genetics, smoking, and certain viral infections. Symptoms vary depending on the affected areas of the nervous system and can include issues with mobility, vision, sensation, and bladder/bowel function among others. Diagnosis involves MRI, spinal fluid analysis, and evoked potential tests. Treatment focuses on reducing inflammation, managing relapses, and alleviating symptoms. Nursing care centers around addressing impairments in mobility,