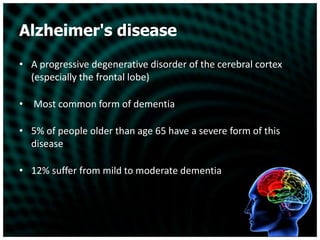
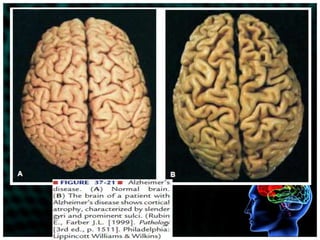
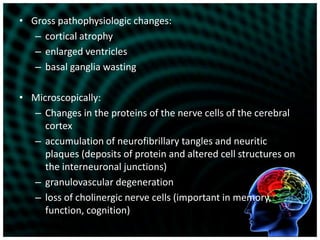
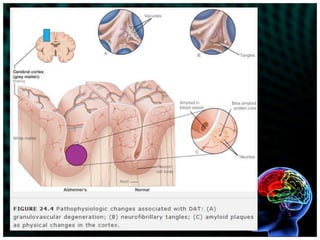
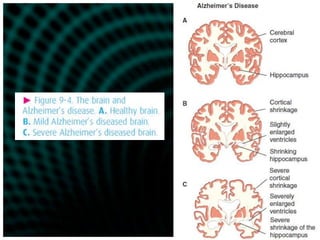
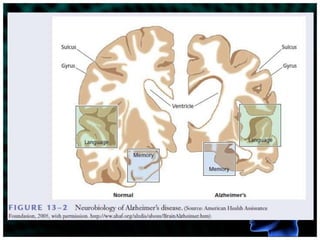
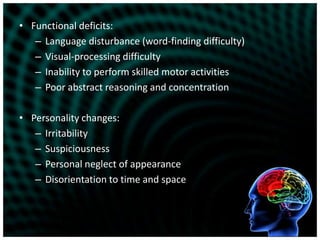
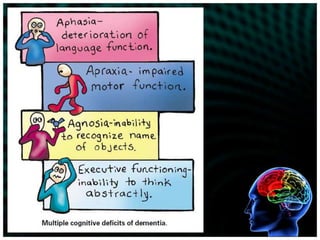
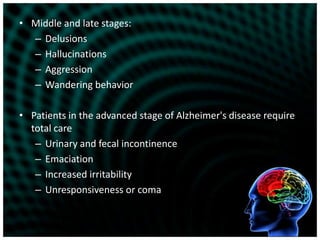
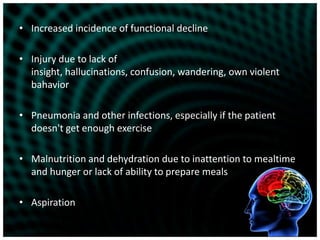
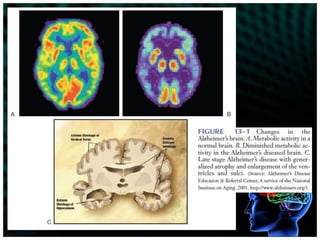
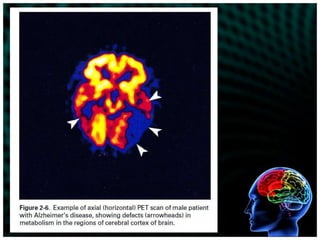
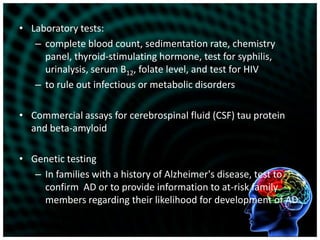
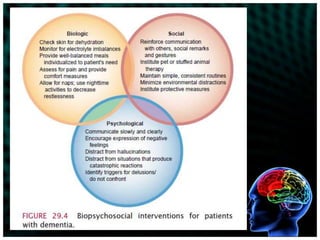
Alzheimer's disease is a progressive degenerative disorder of the brain that initially involves memory loss and cognitive decline, and ultimately results in severe impairment in all areas of functioning. While medications can temporarily improve symptoms, there is no cure. The disease progresses through mild, moderate, and severe stages characterized by worsening memory loss, impaired communication and ability to care for oneself, and may eventually involve inability to walk or speak intelligibly. Patients and families require education and support to understand and cope with the progression of the disease.