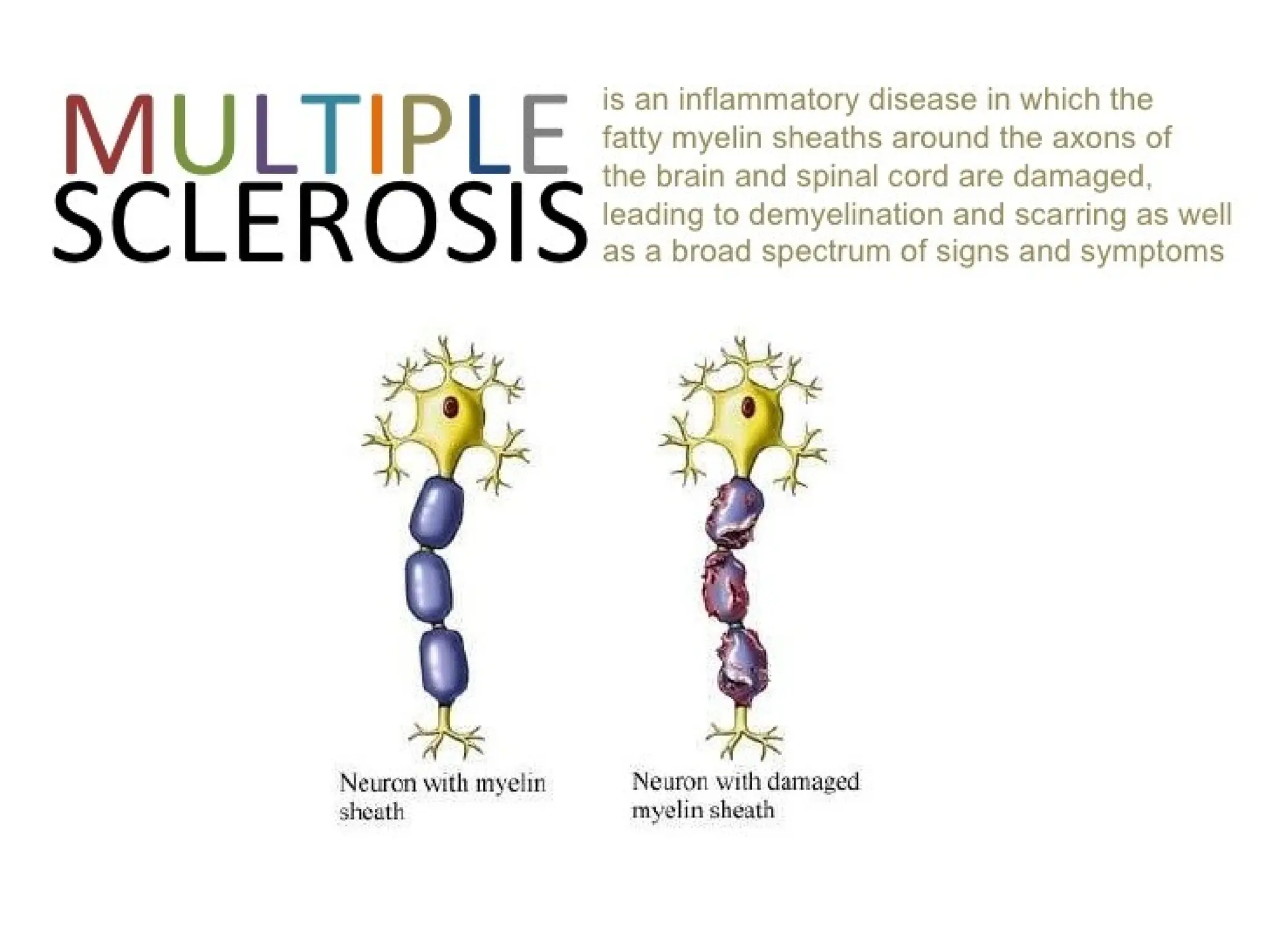
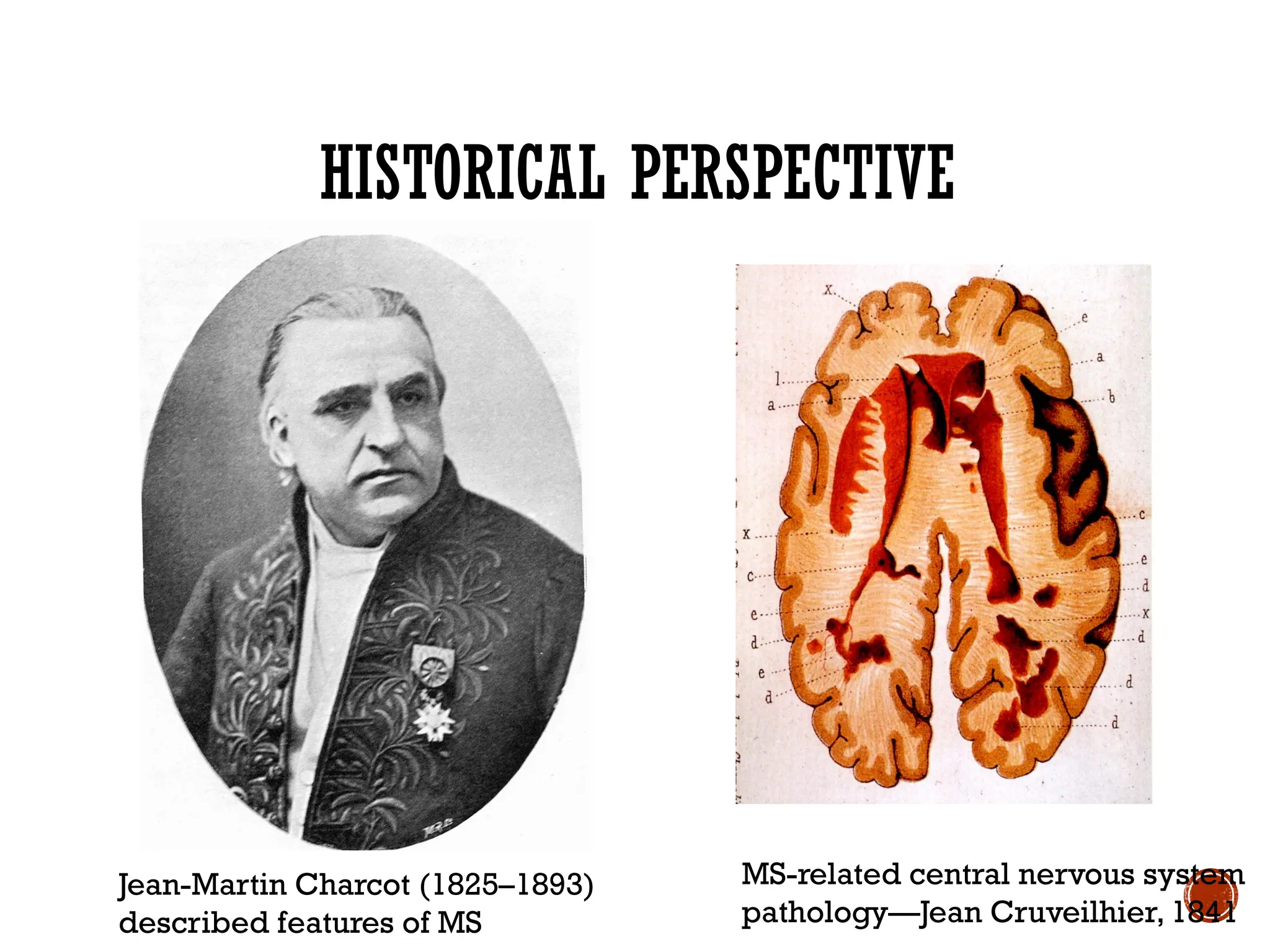
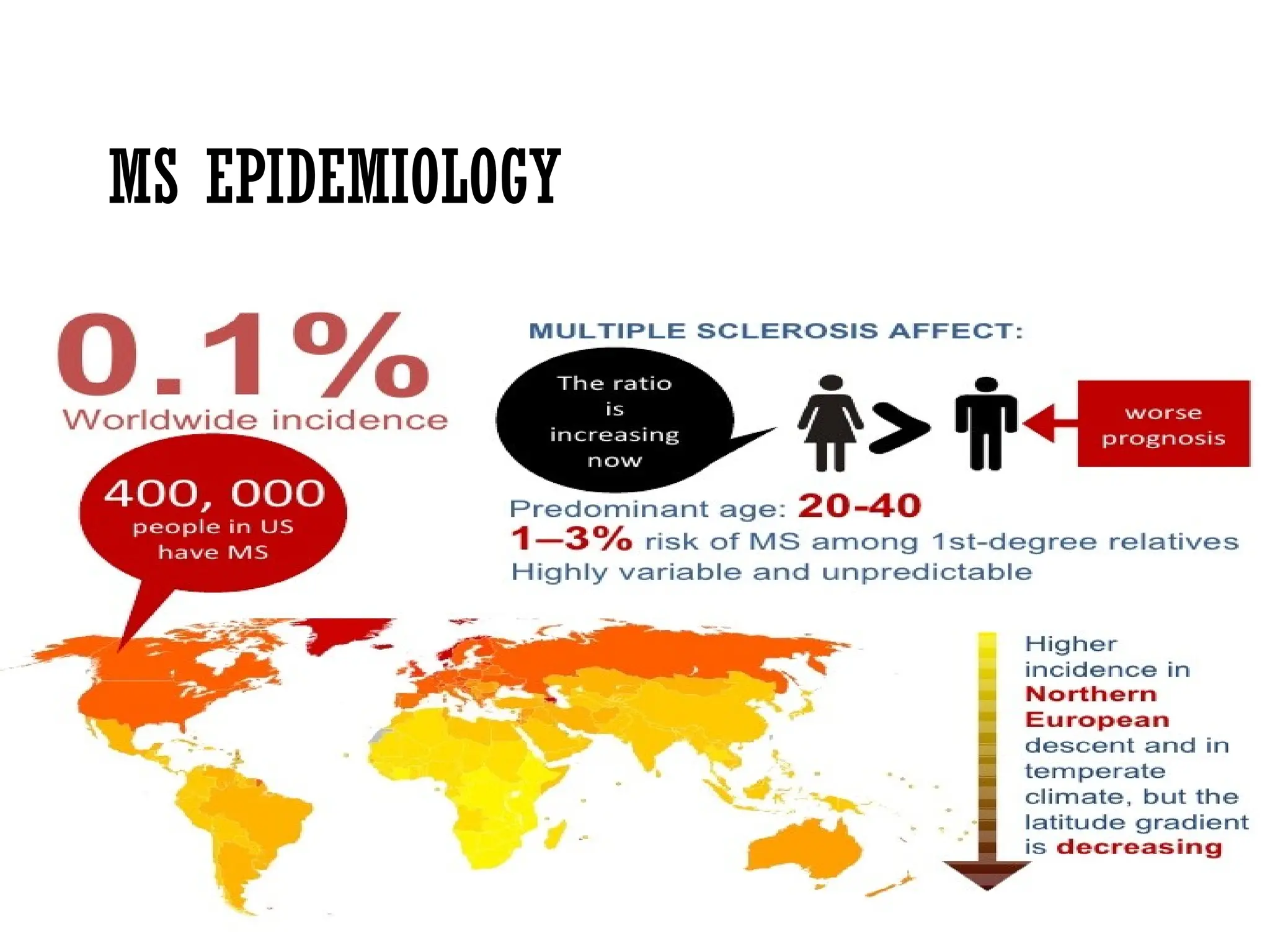
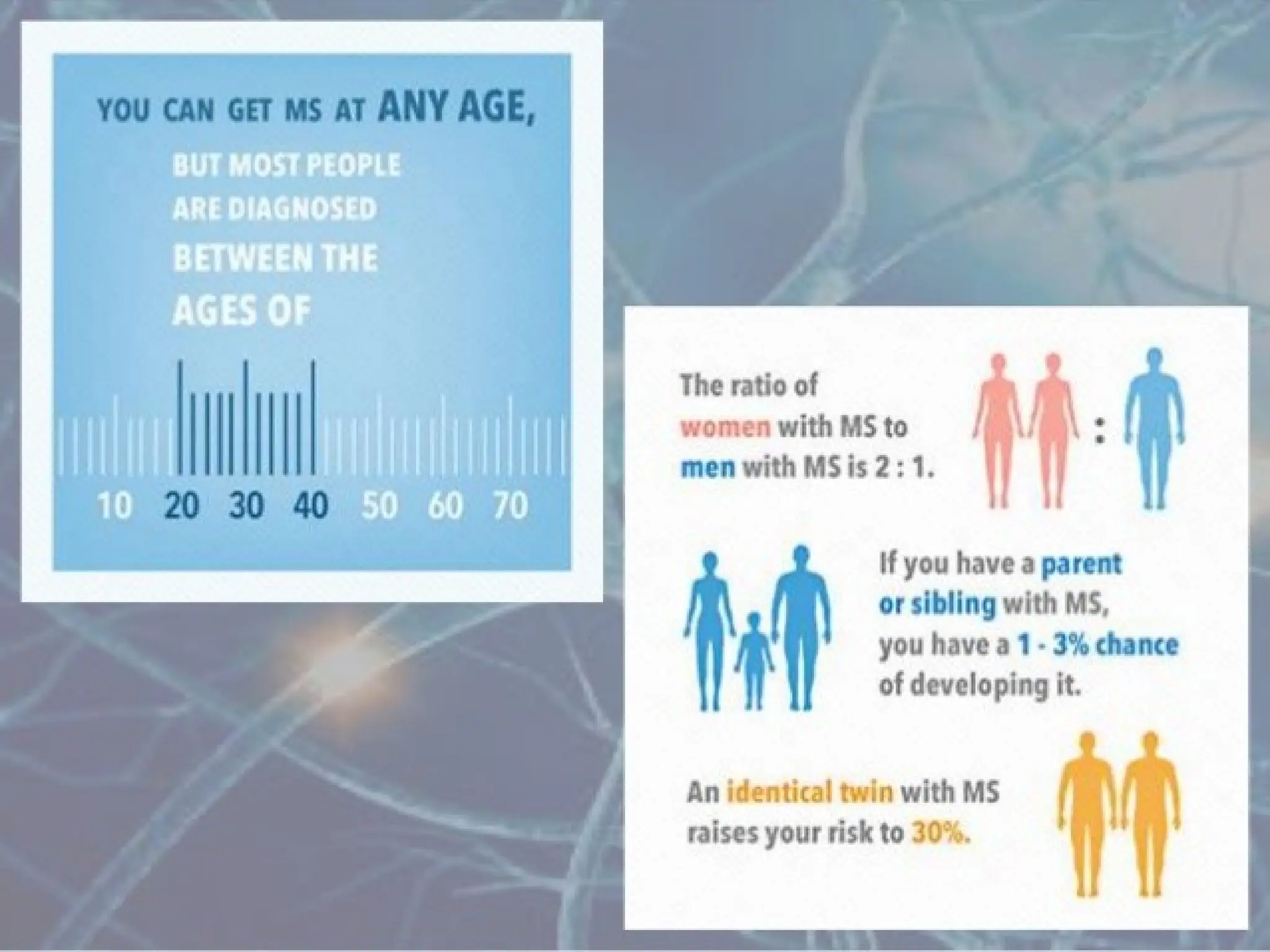
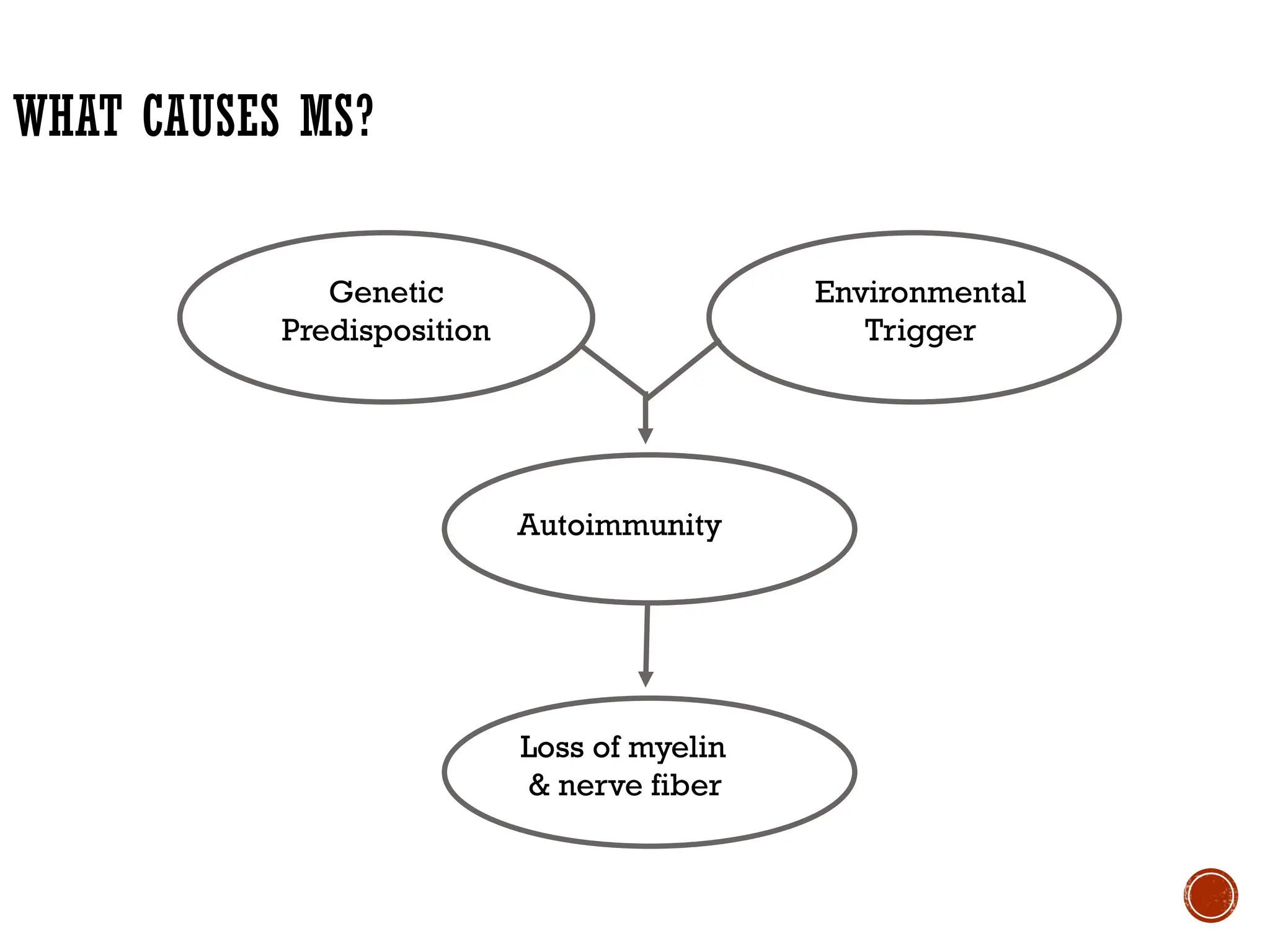
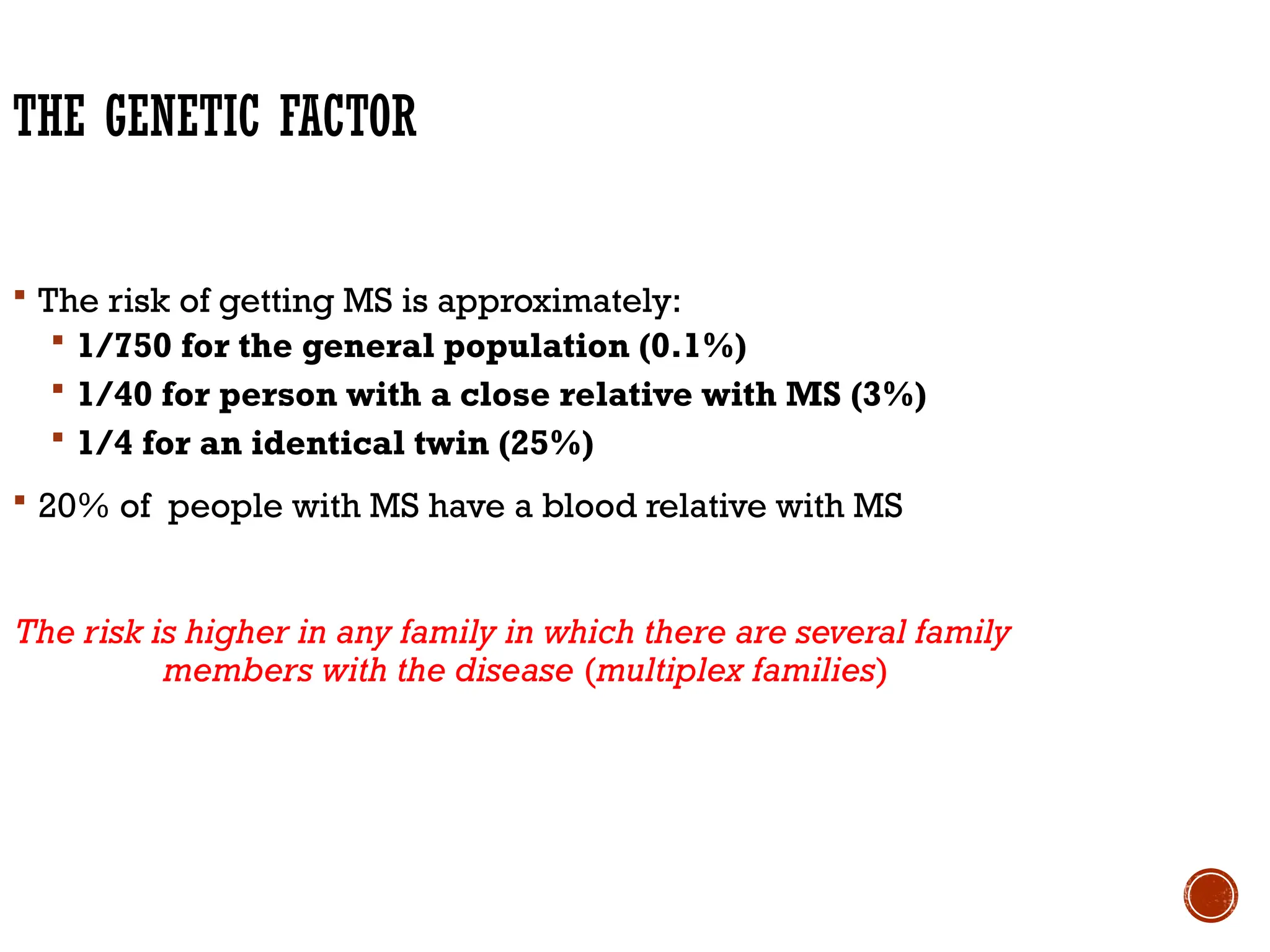
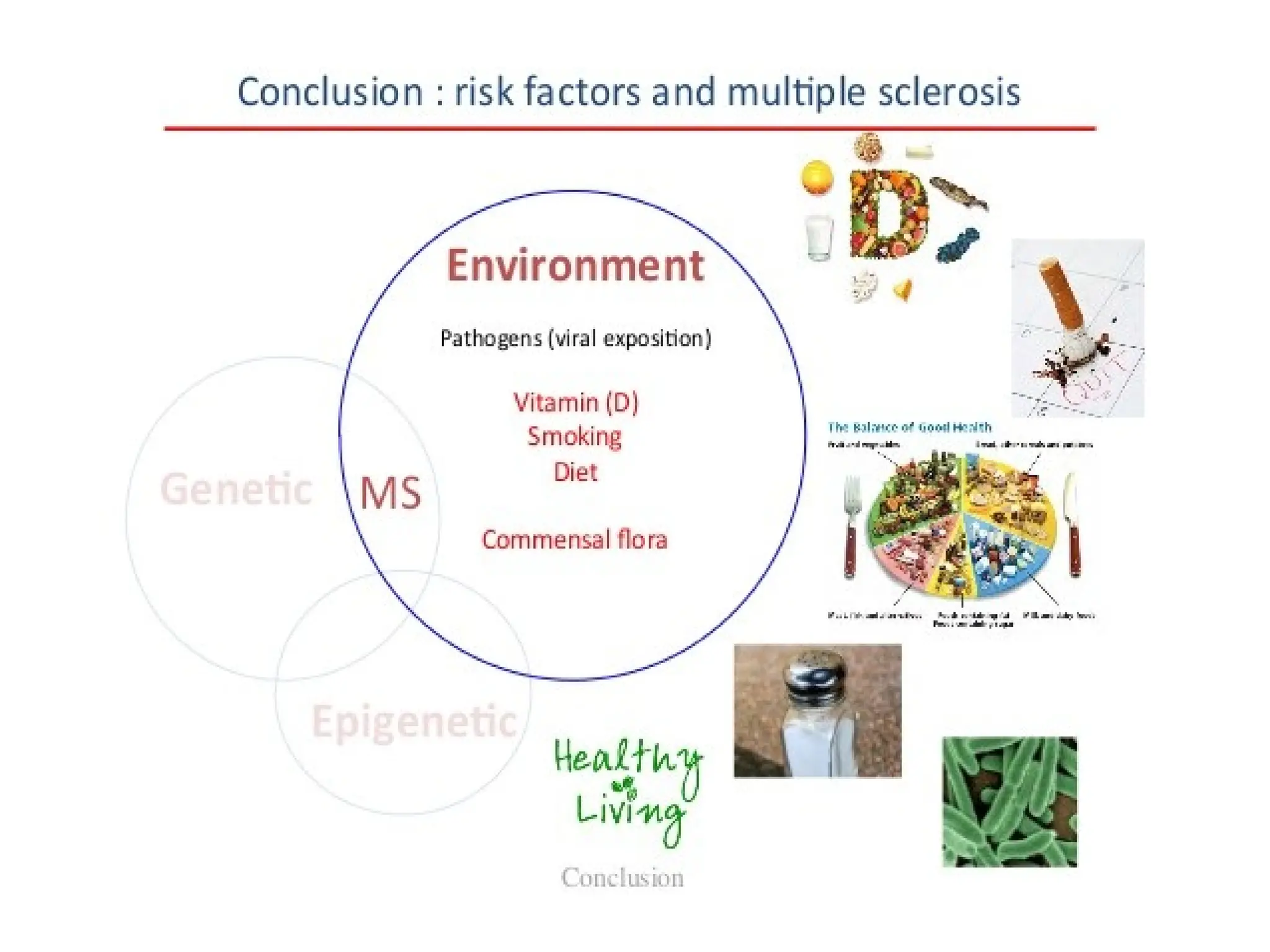
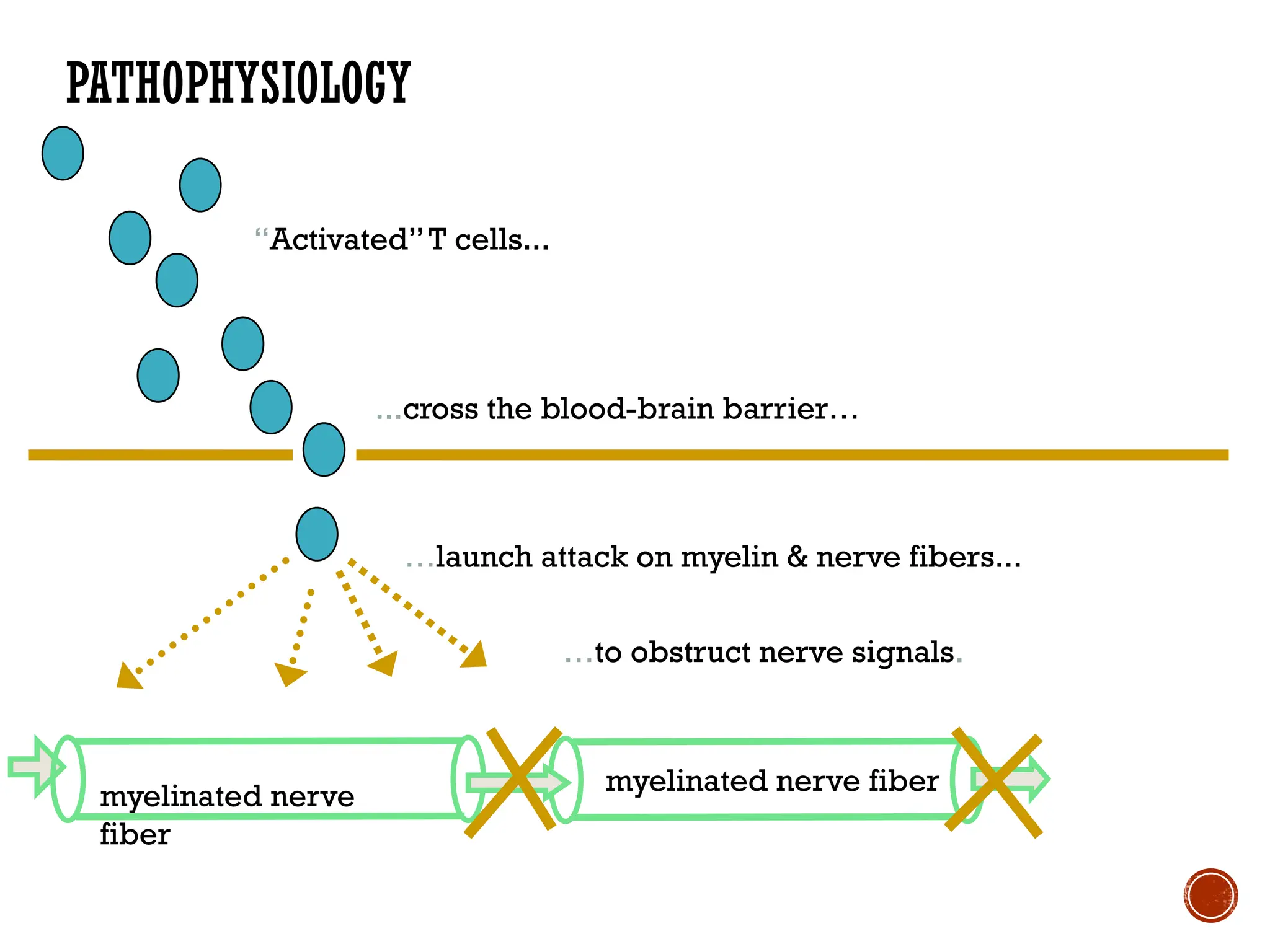
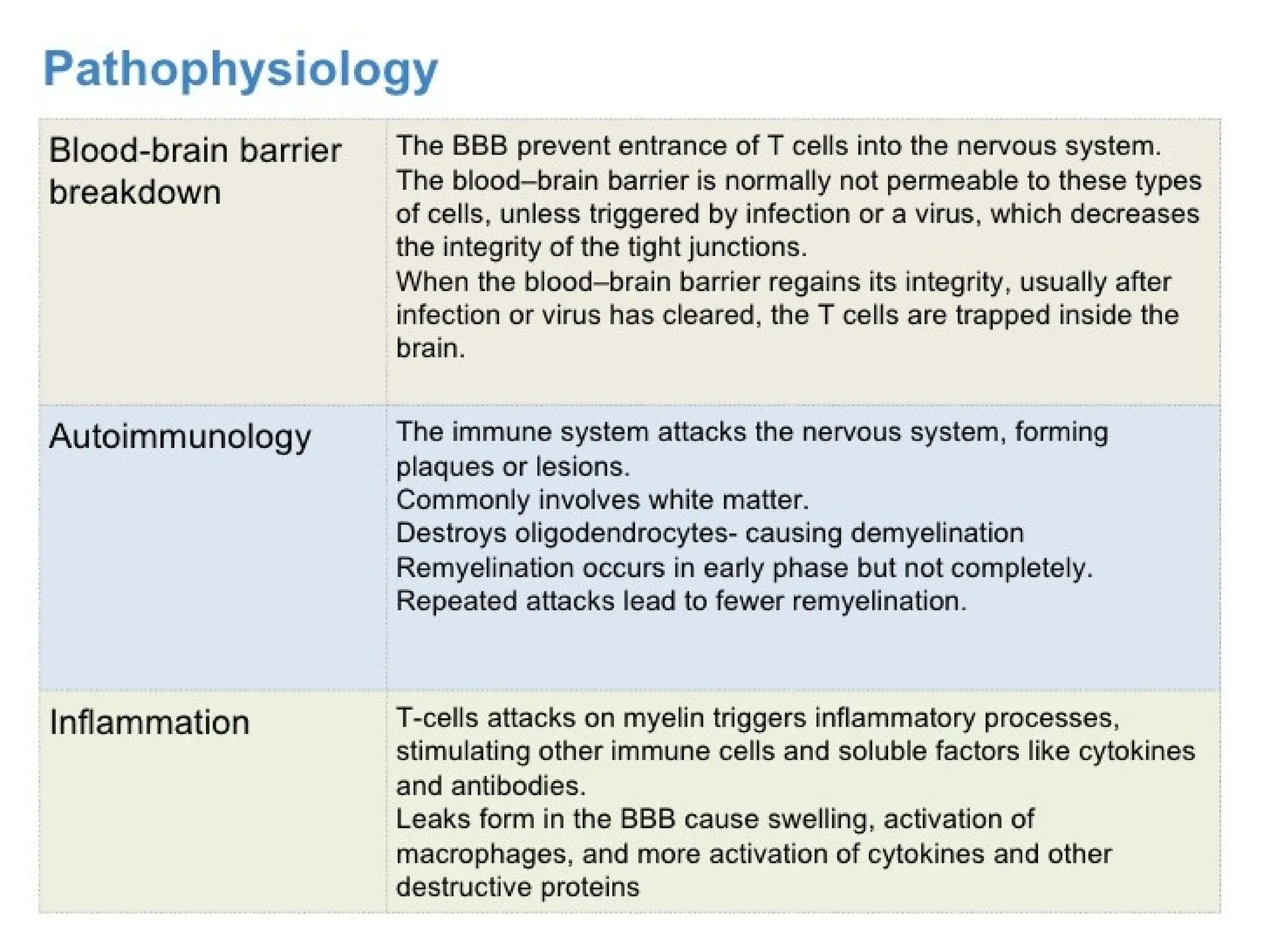
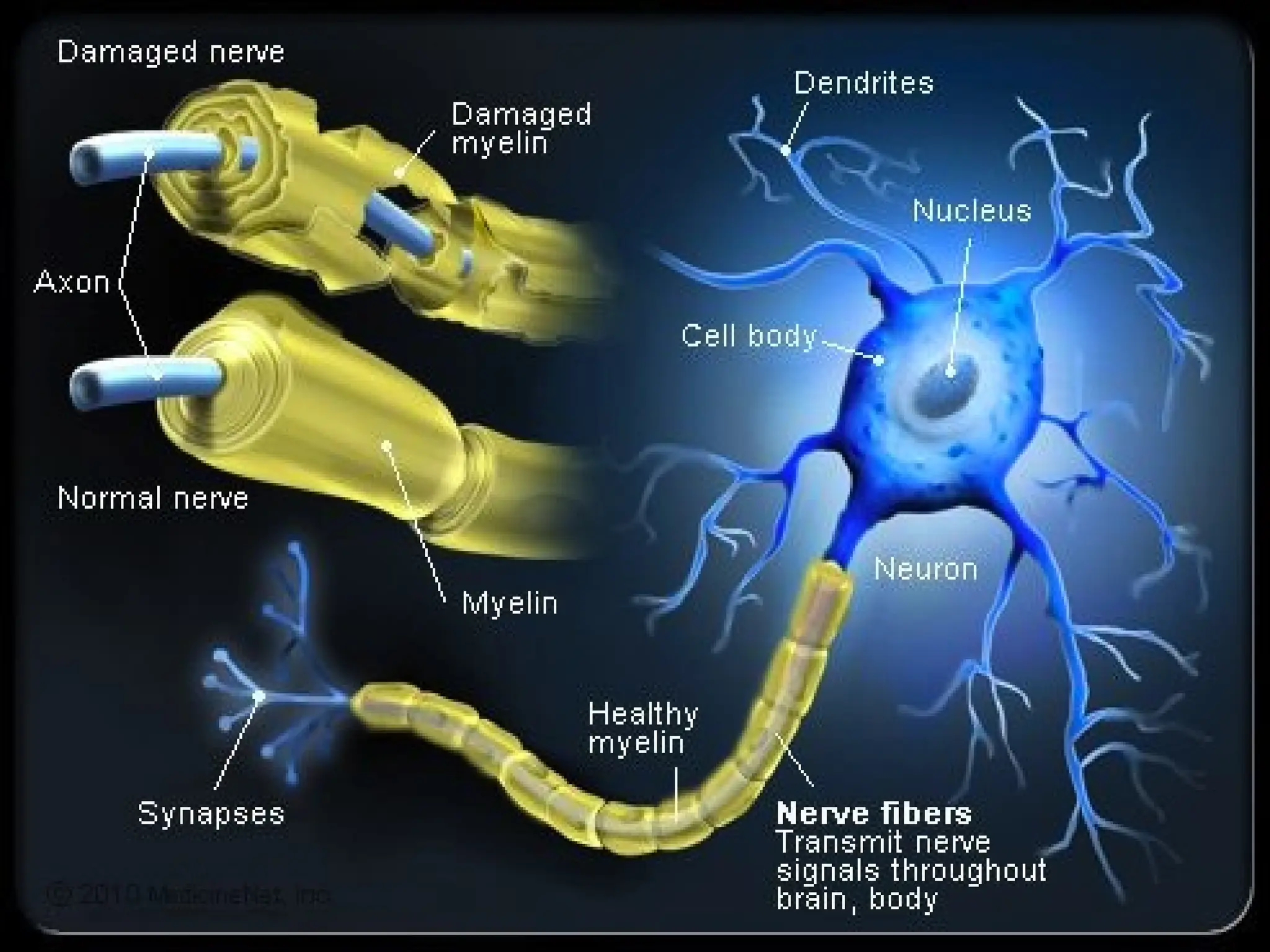
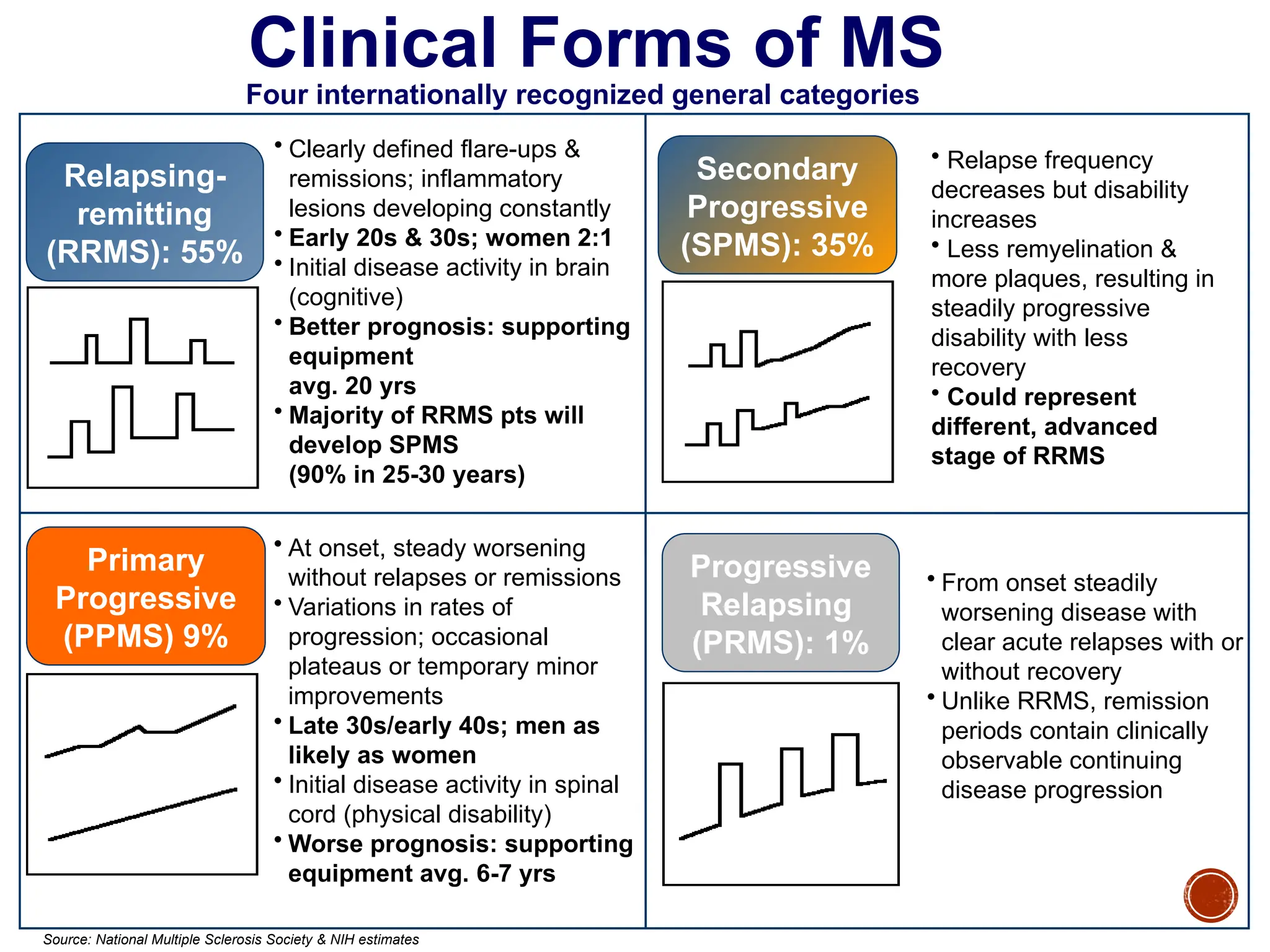
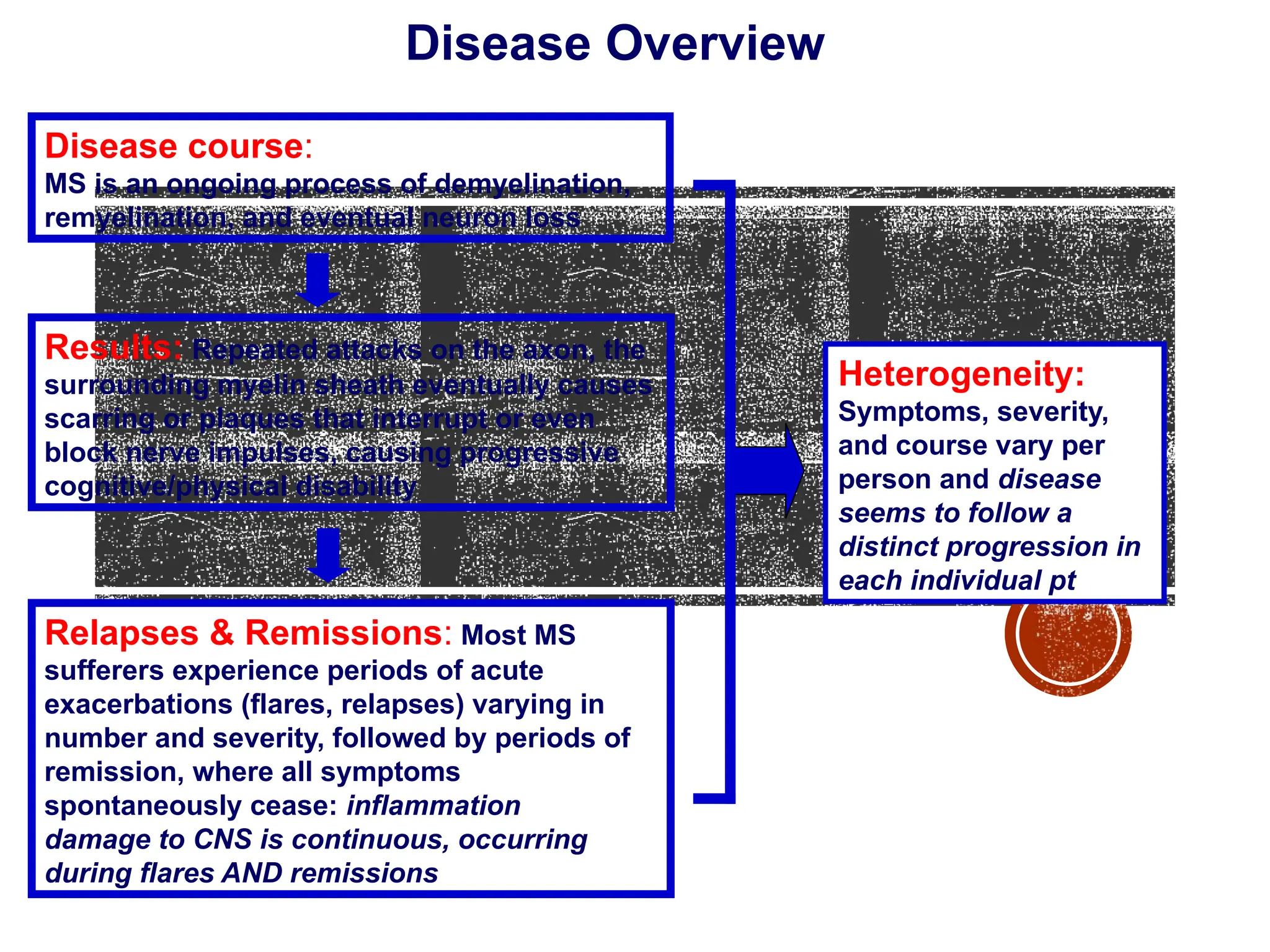
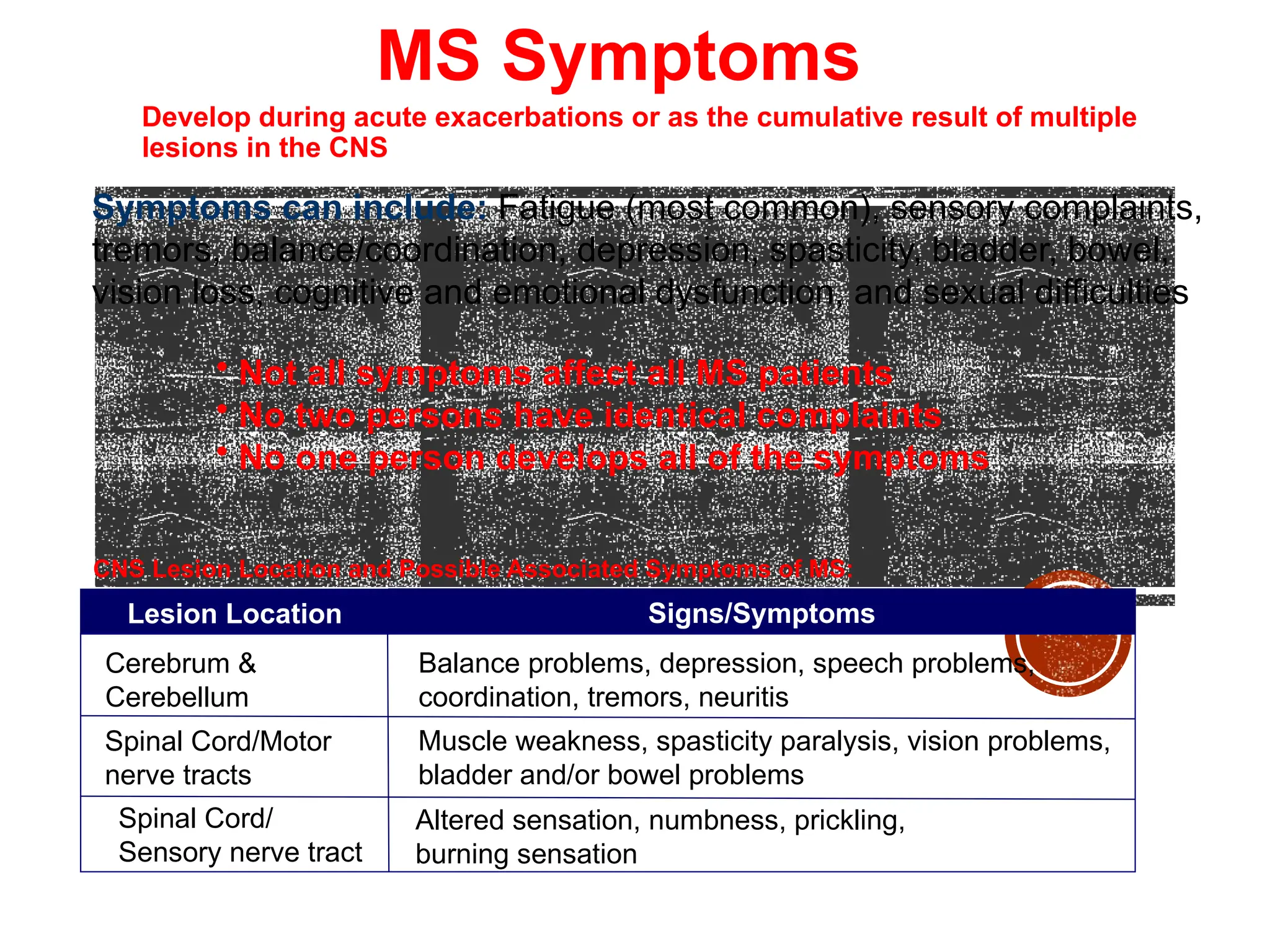
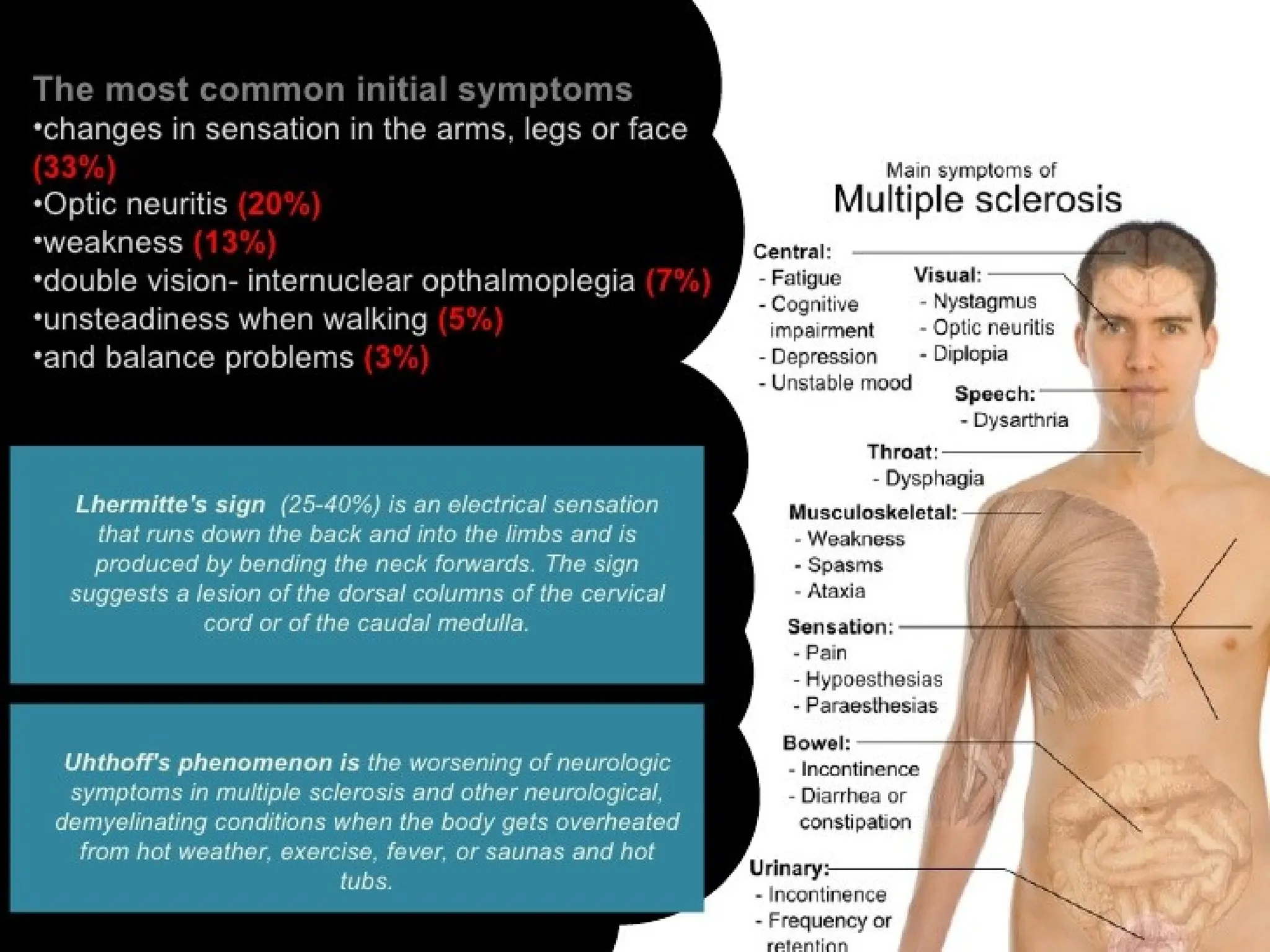
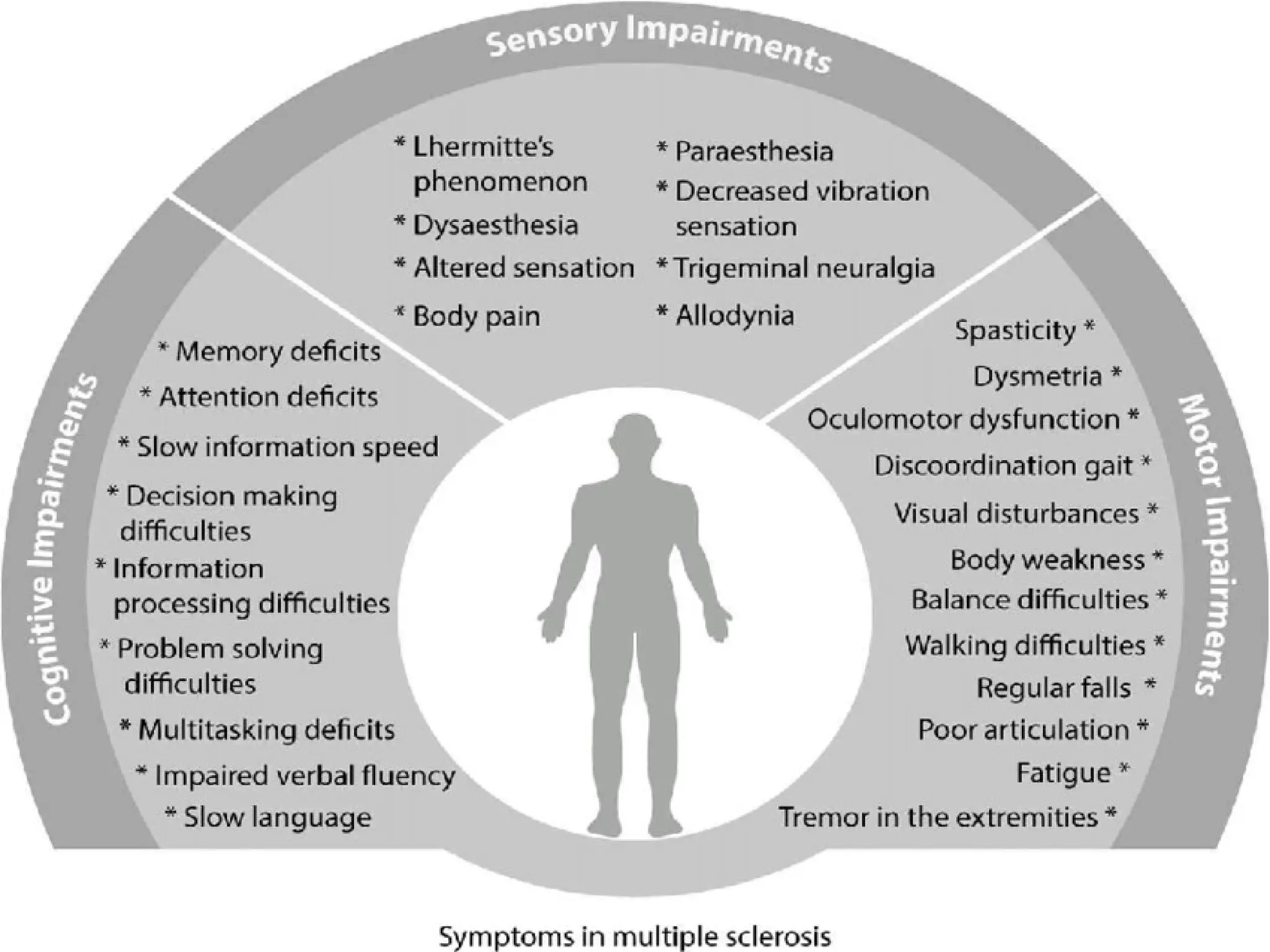
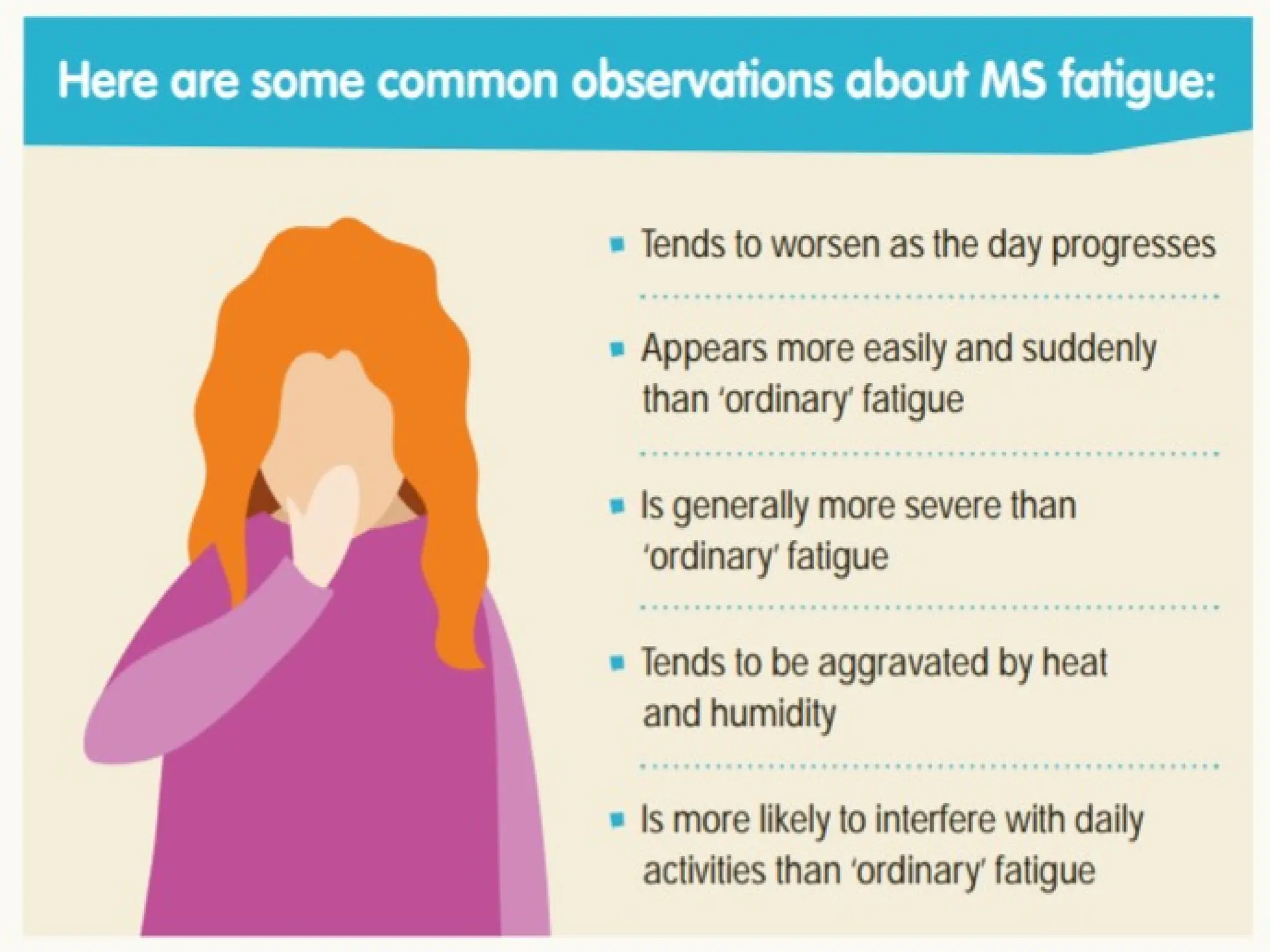
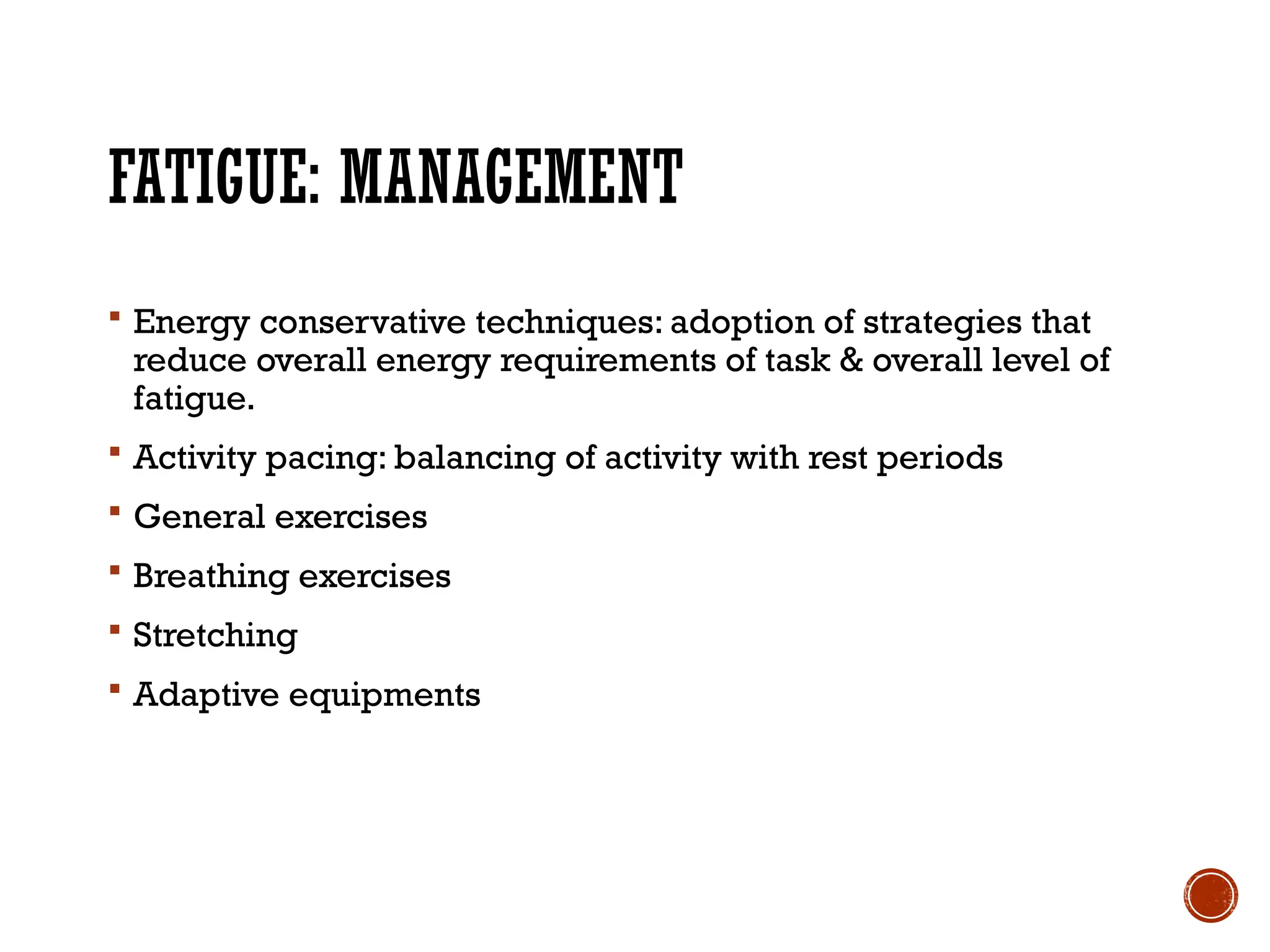
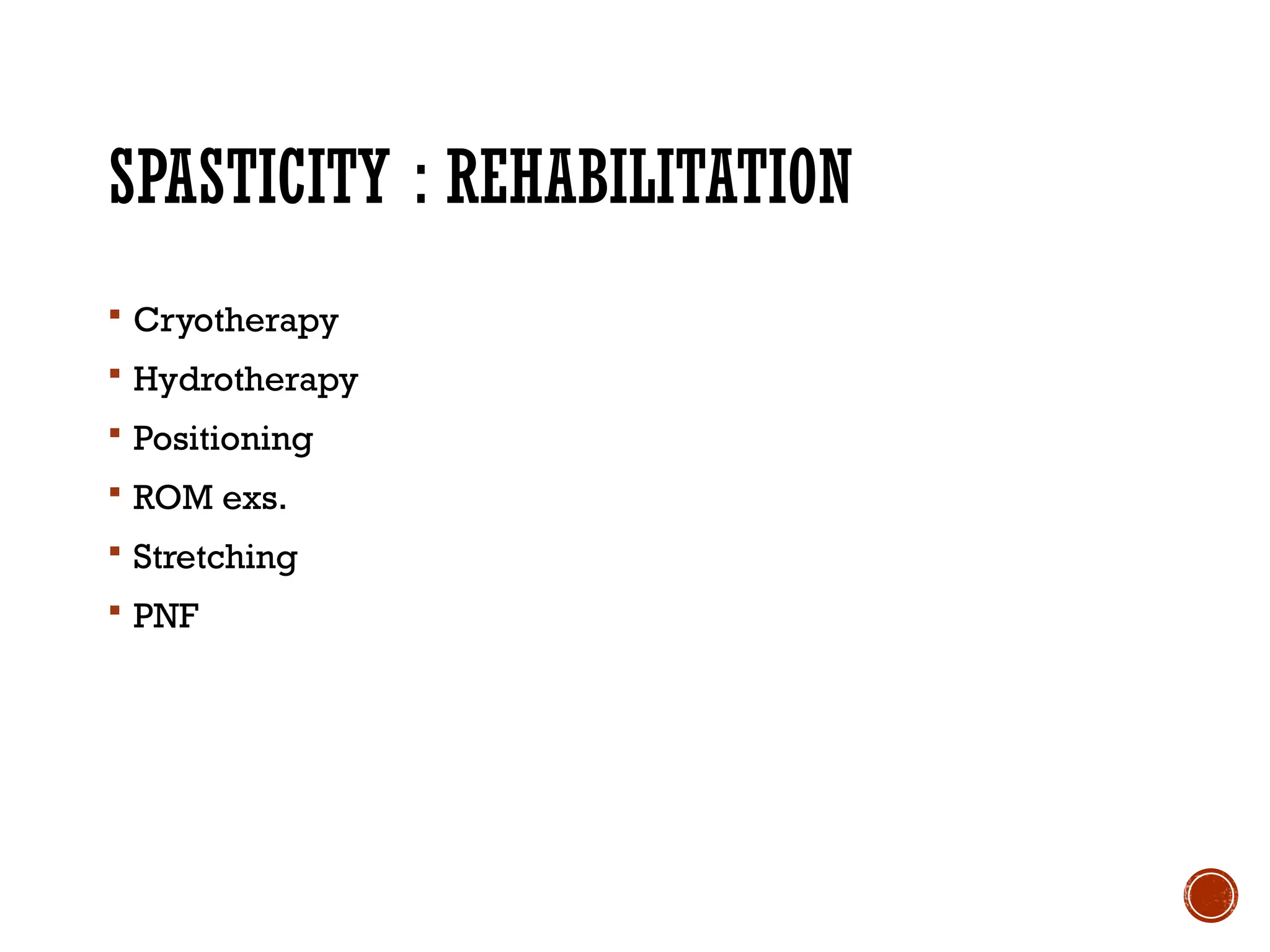
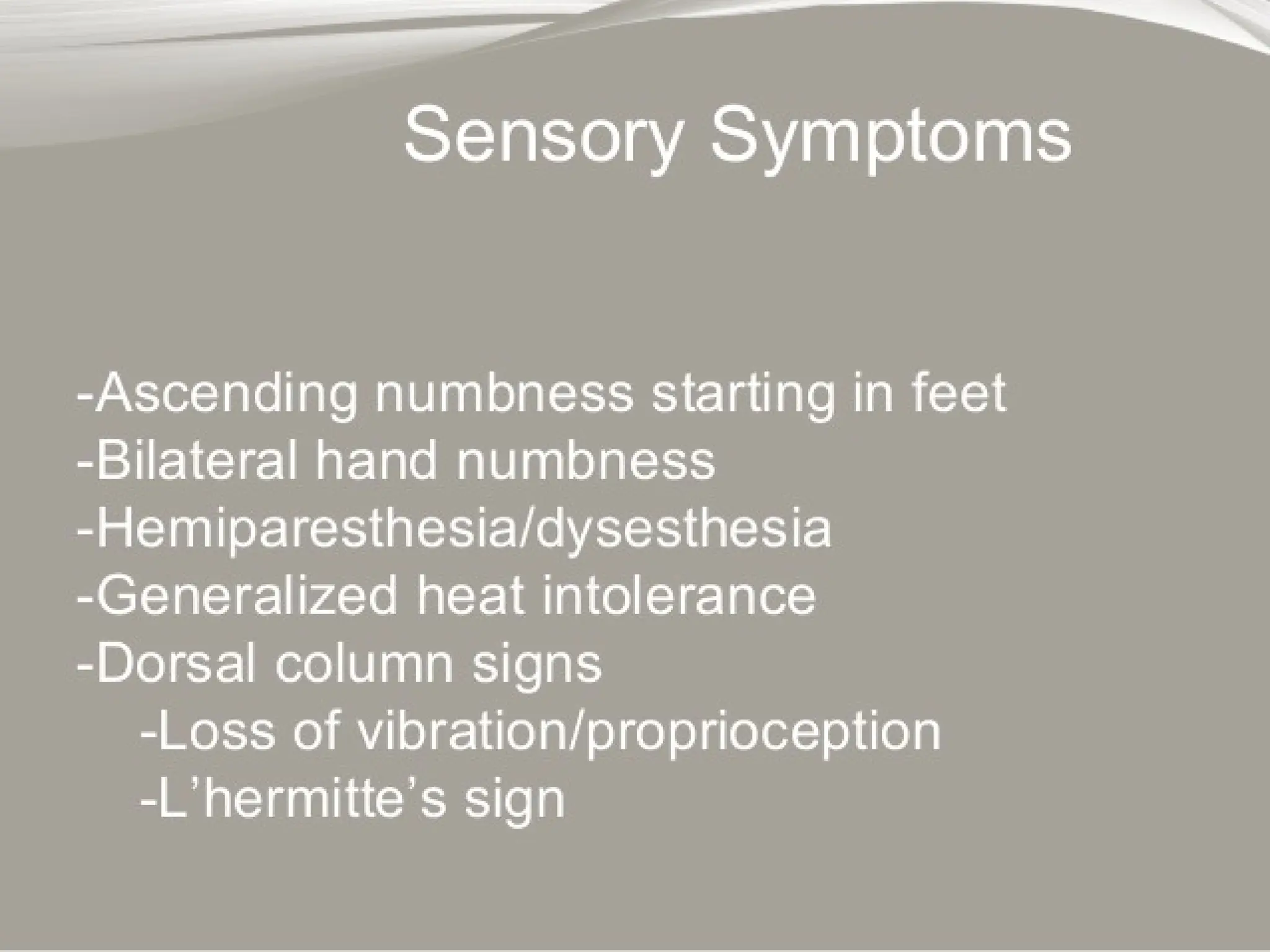
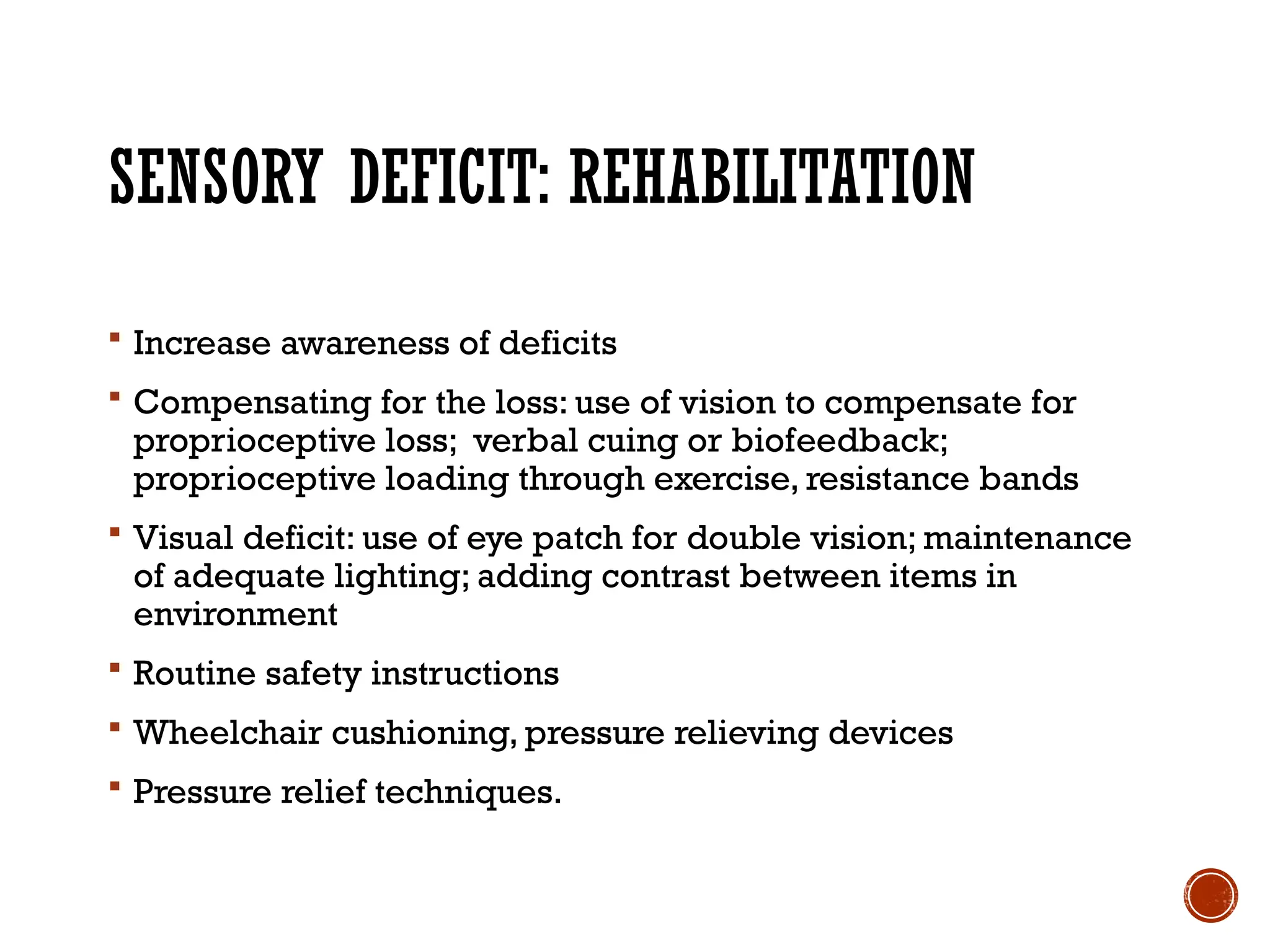
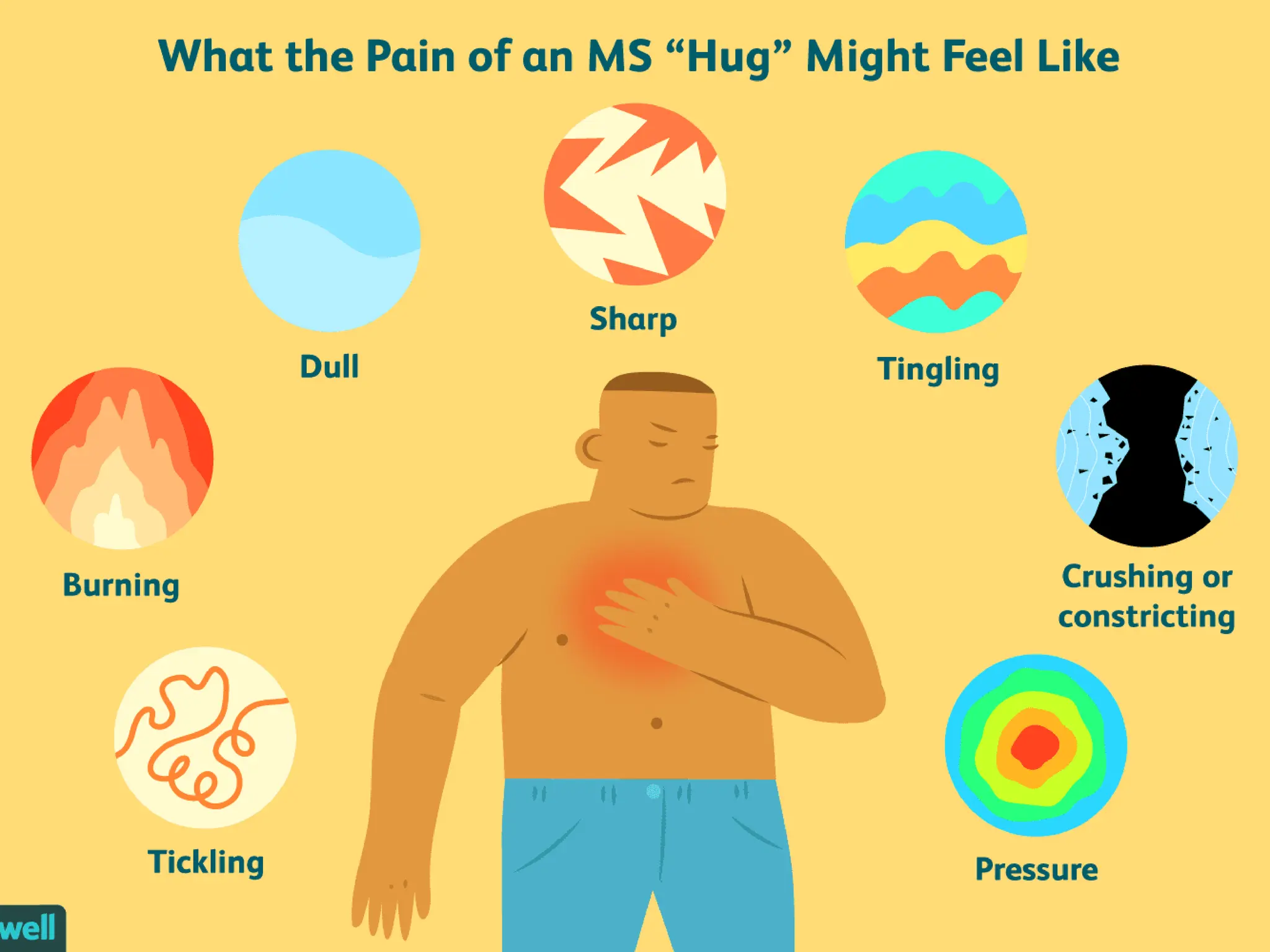
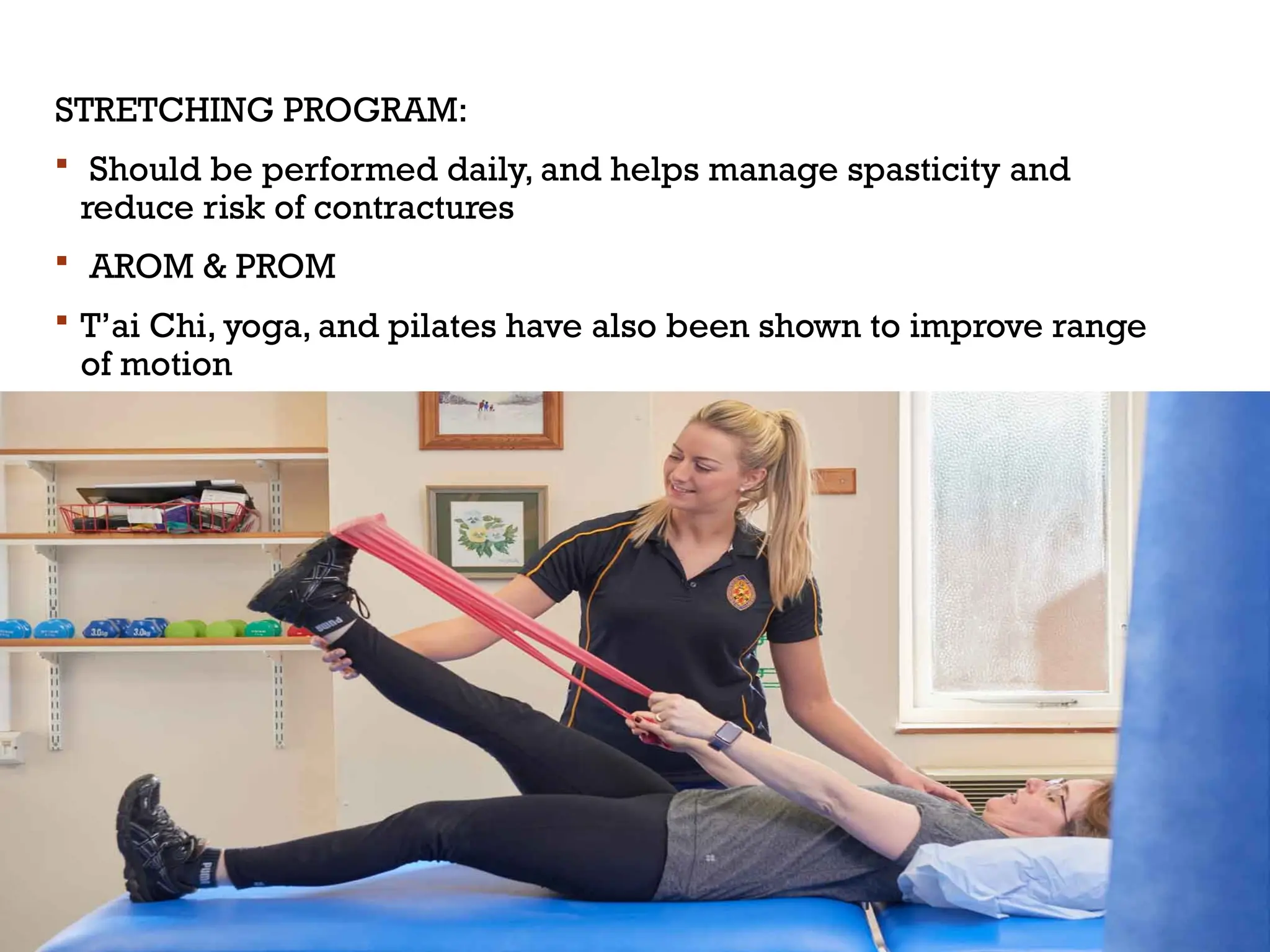
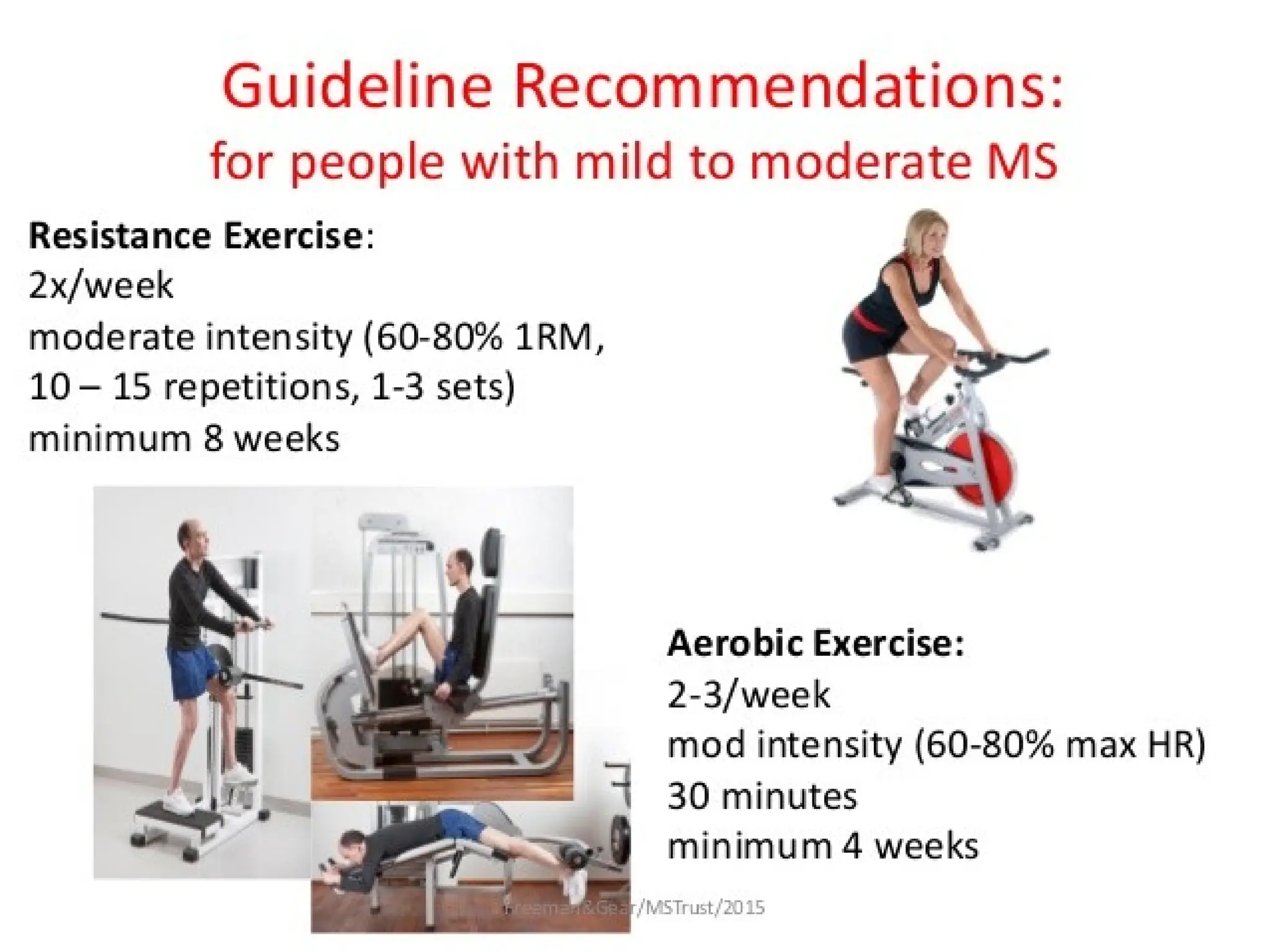
The document discusses the various aspects of physical therapy for patients with multiple sclerosis (MS), including its historical perspective, epidemiology, and pathophysiology. It outlines different clinical forms of MS, typical symptoms, and the impact of rehabilitation methods such as exercise and physiotherapy assessment on managing symptoms and improving quality of life. Key strategies for management include energy conservation techniques, balance training, and tailored exercise programs to enhance mobility, reduce fatigue, and address specific challenges faced by individuals with MS.