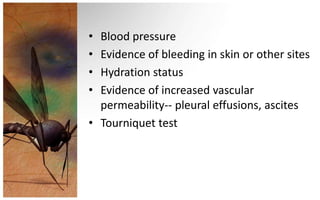
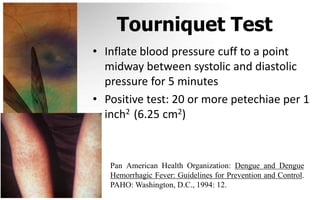
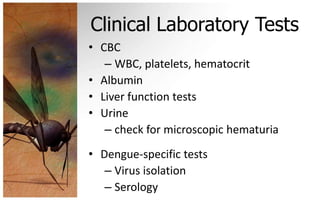
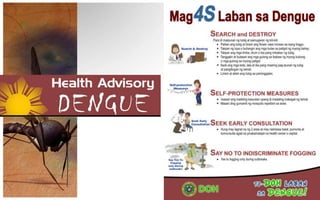
This document provides an overview of dengue fever, including its causes, transmission, global impact, and prevention. Some key points:
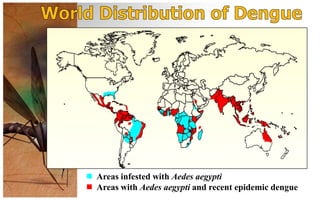
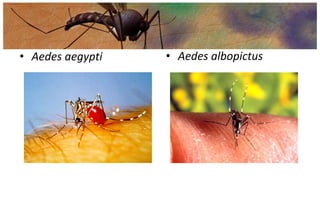
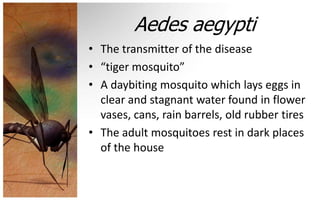
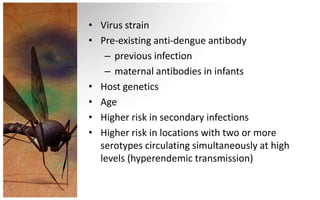
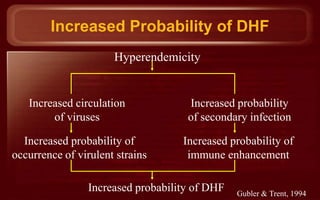
- Dengue fever is a viral disease transmitted by Aedes mosquitoes, primarily Aedes aegypti. There are 4 types of dengue viruses.
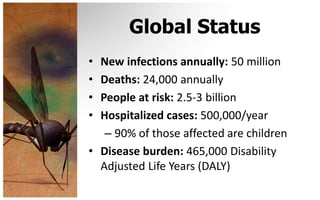
- It affects over 50 million people annually worldwide and is a major public health challenge in many tropical and subtropical countries, including the Philippines.
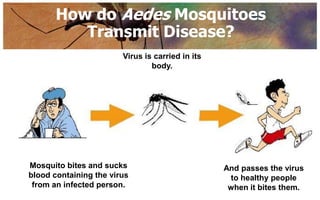
- Transmission occurs when an infected mosquito bites a person and transmits the virus. There is typically an incubation period of 4-7 days before symptoms appear.
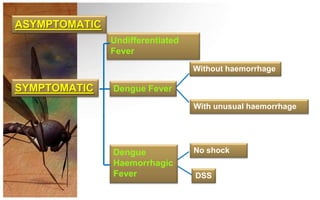
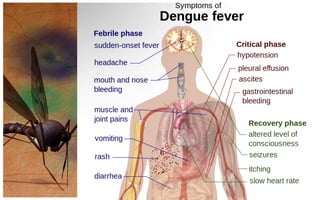
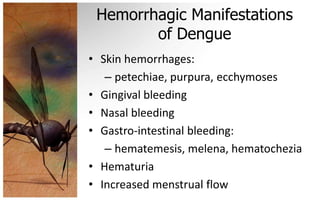
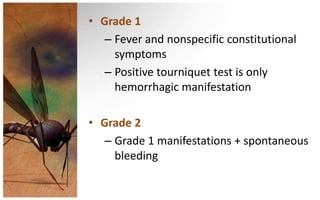
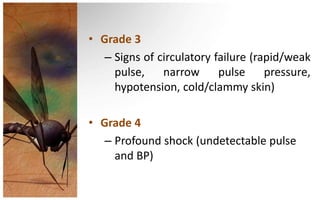
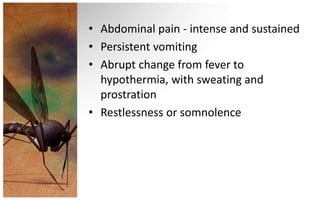
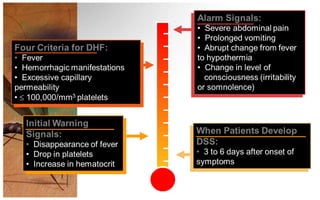
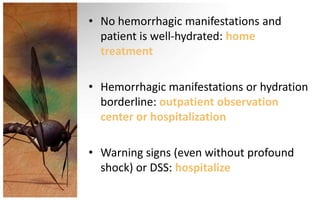
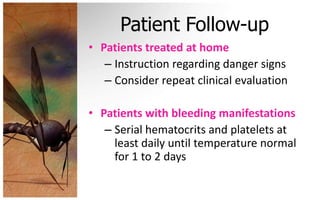
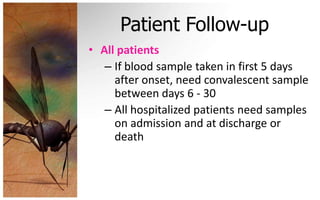
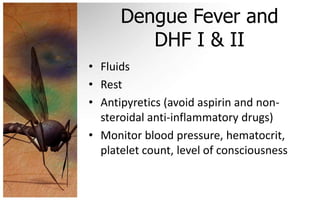
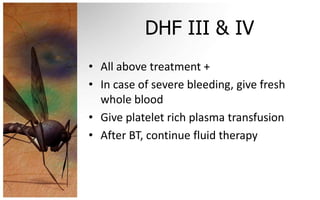
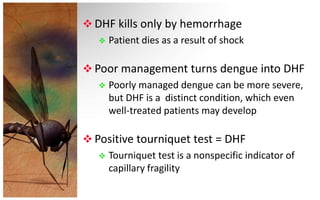
- Symptoms range from mild fever to severe dengue hemorrhagic fever. Treatment depends on