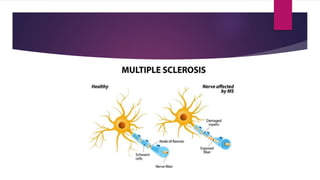
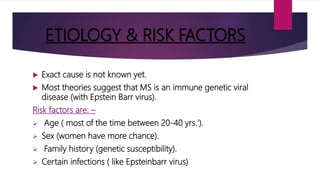
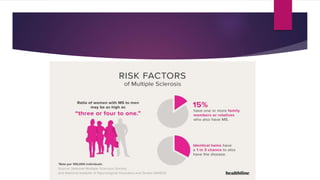
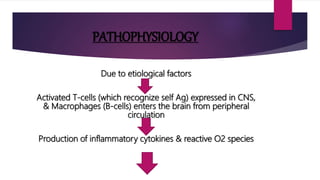
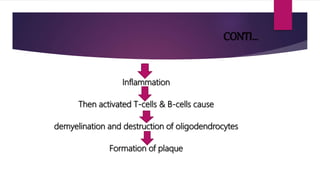
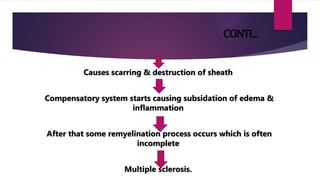
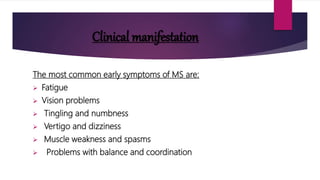
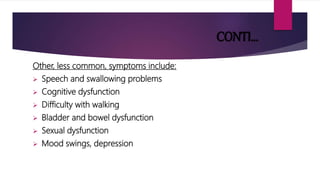
Multiple sclerosis is a chronic demyelinating disease that affects the central nervous system. It occurs most often in people between 20-40 years of age and is more prevalent in women and individuals living in colder climates. The exact cause is unknown but is thought to involve genetic susceptibility and viral triggers. Symptoms vary depending on the affected areas of the nervous system and can include vision problems, numbness, weakness, and cognitive issues. While there is no cure, treatment aims to manage symptoms and slow disease progression.