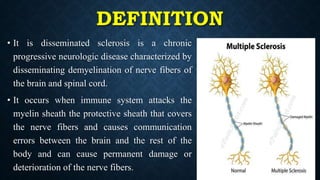
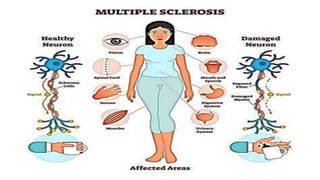
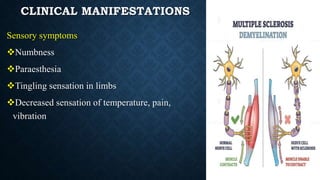
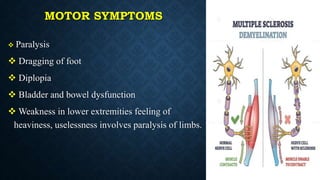
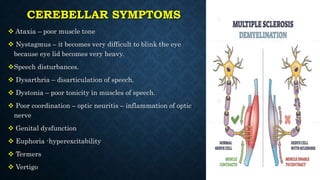
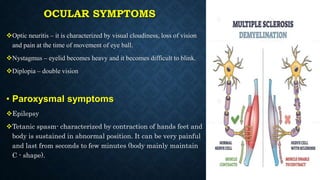
Multiple sclerosis (MS) is a chronic progressive neurological disorder characterized by the demyelination of nerve fibers in the brain and spinal cord, commonly affecting women aged 20-40. Its causes are largely unknown, but factors such as family history, infections, and environmental conditions may play a role. Clinical manifestations include sensory, motor, and ocular symptoms, with various classifications of the disease depending on the progression and severity of symptoms.