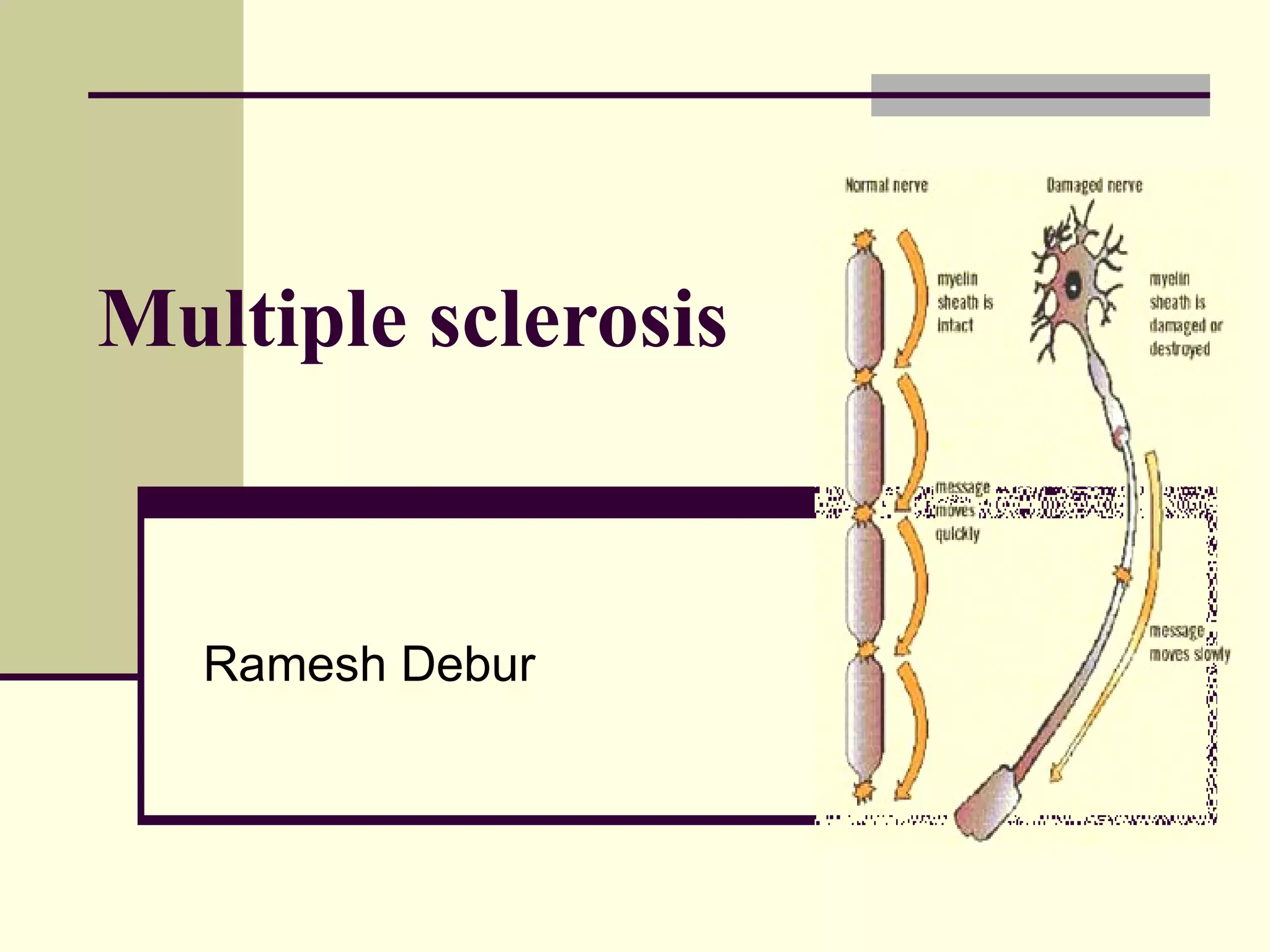
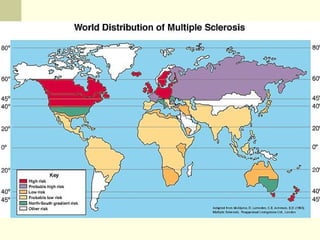
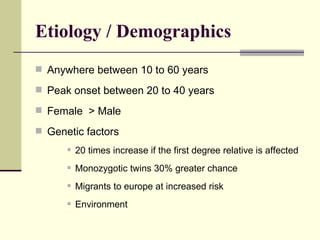
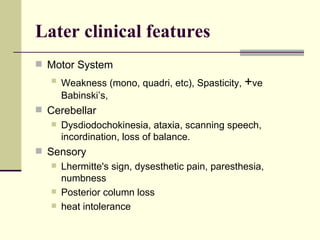
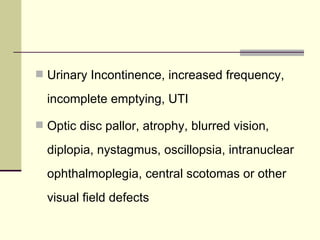
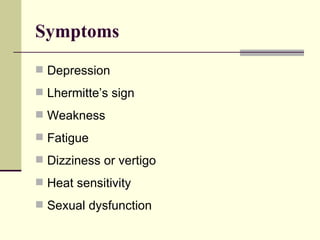
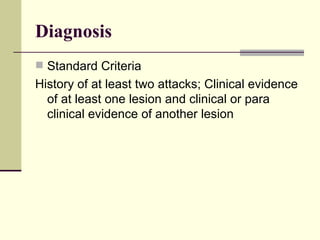
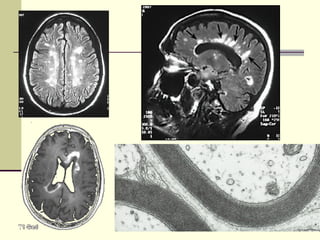
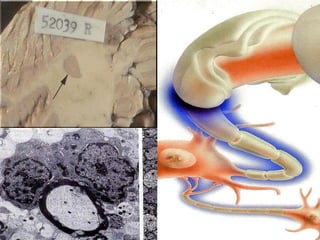
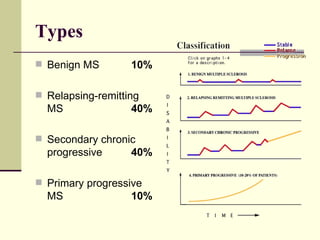
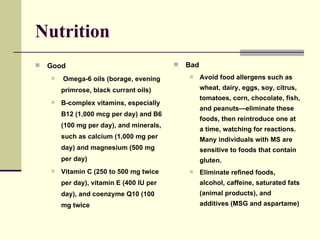
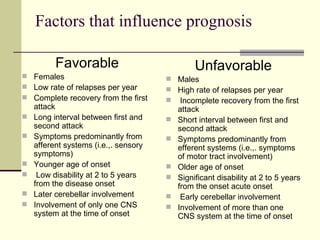
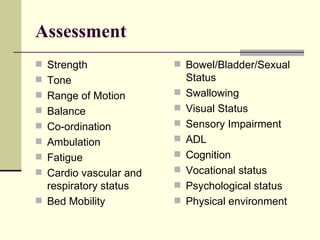
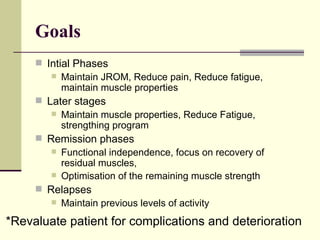
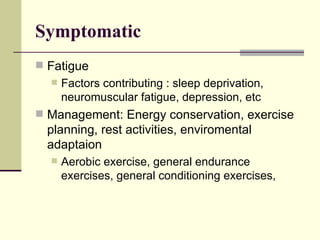
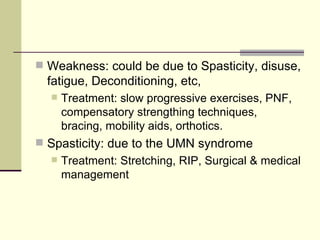
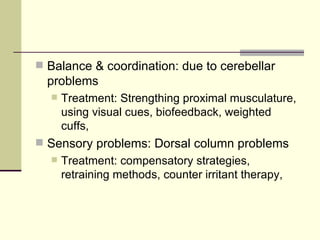
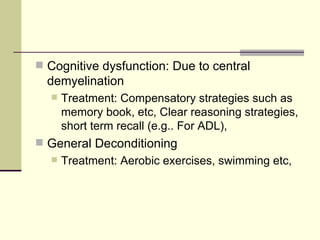
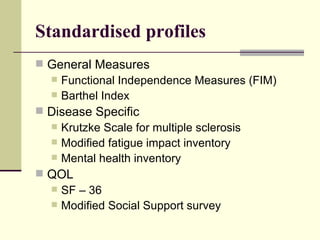
Multiple sclerosis is an inflammatory demyelinating disorder of the central nervous system that is more common in northern latitudes and among Caucasian populations. It typically presents with sensory disturbances, weakness, and visual problems and is diagnosed based on disseminated lesions found on MRI. Management involves immunosuppression and physical/occupational therapy to address symptoms and maintain function. Prognosis depends on factors like age of onset, relapse rate, and the degree of disability.