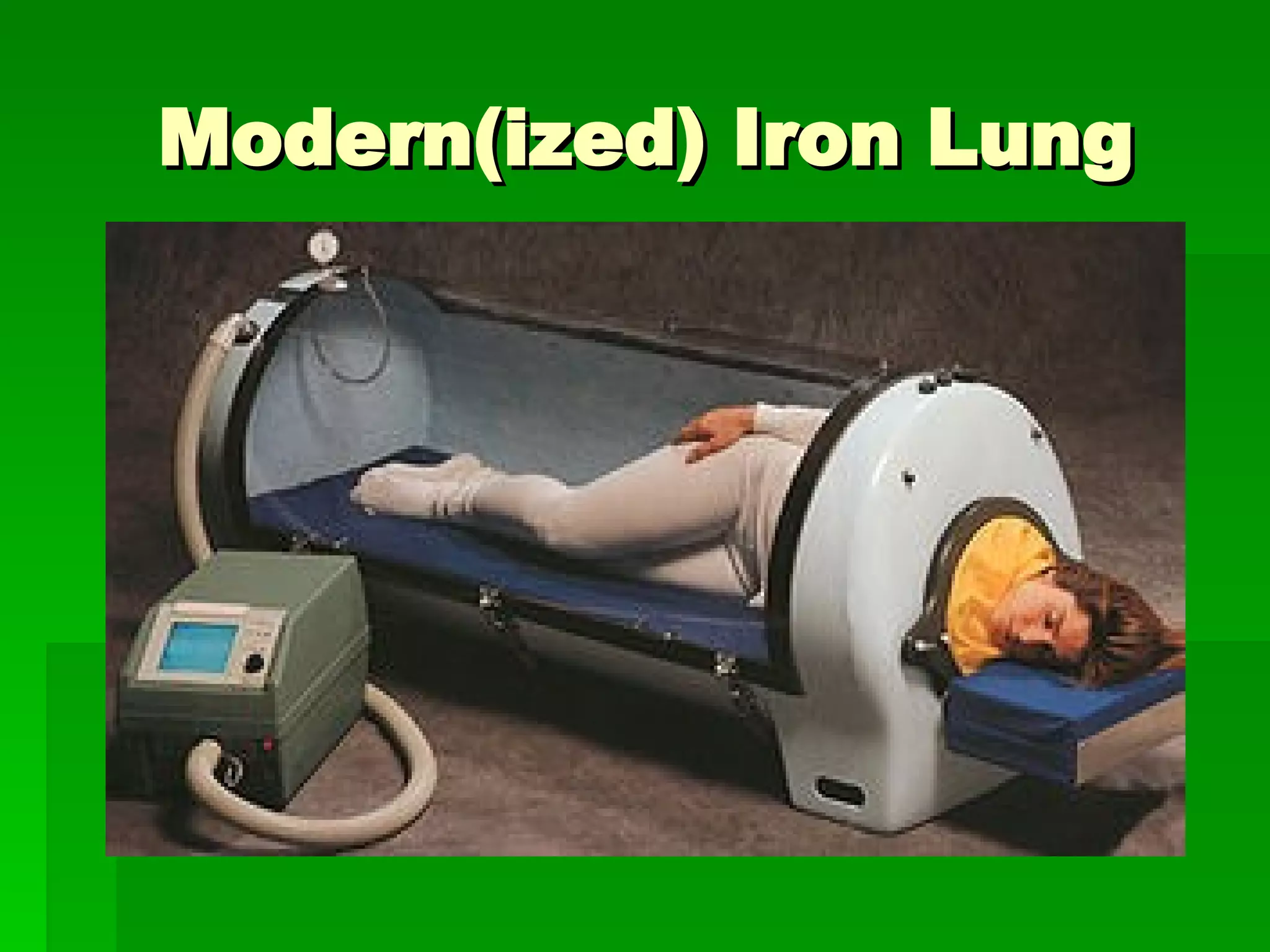
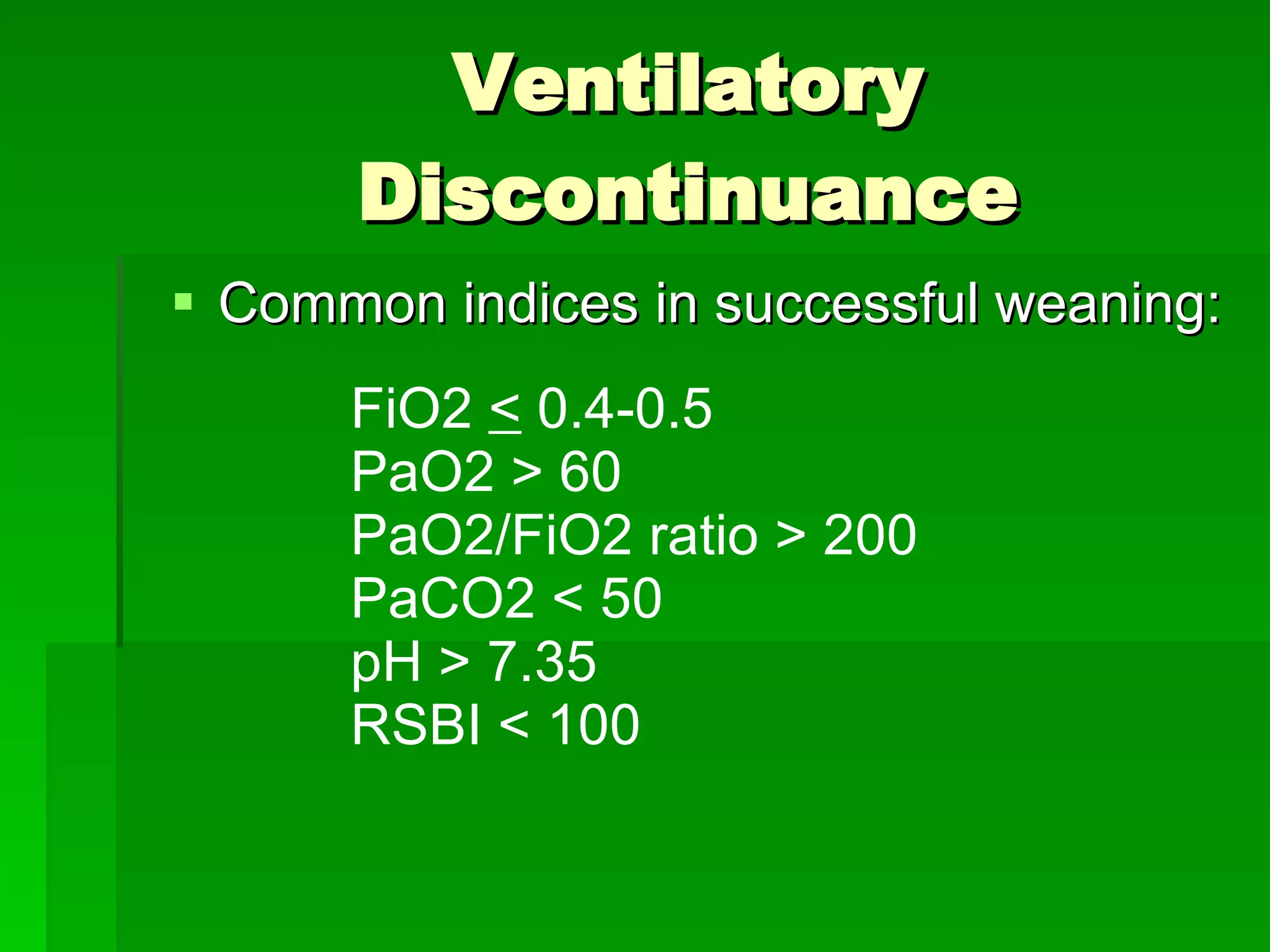
This document provides an overview of mechanical ventilation, including indications for use, key terms, types of ventilation modes, complications, and weaning from ventilation support. It describes positive pressure ventilation as the primary method, using controlled and supportive ventilation modes. Controlled modes deliver set tidal volumes and rates while supportive modes rely on patient triggering. Complications include ventilator-induced lung injury from excessive pressures or volumes and ventilator-associated pneumonia. Successful weaning depends on patient stability in ventilation, oxygenation, cardiovascular function and psychological state.