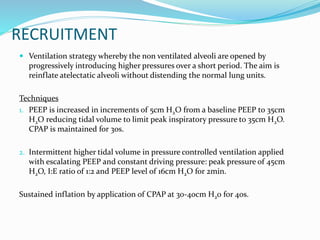
Modern ventilators use electromagnetic valves and microprocessors to control gas flow. They monitor factors like tidal volume, respiratory rate, inspiratory/expiratory ratios, PEEP, peak pressures, and compliance to optimize ventilation for patients. Recruitment techniques apply higher pressures to reopen collapsed alveoli without overdistending healthy ones. Weaning assessments evaluate readiness to transition patients off ventilator support and restore spontaneous breathing.