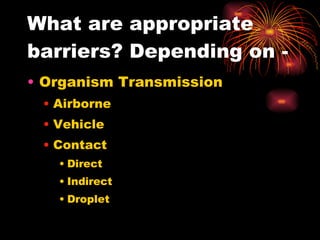
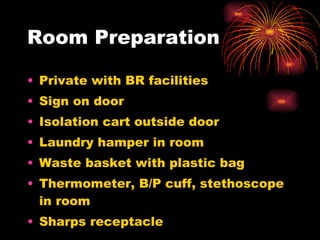
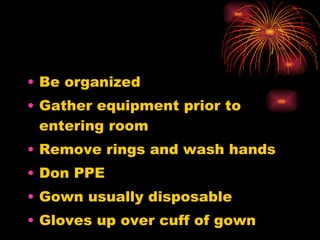
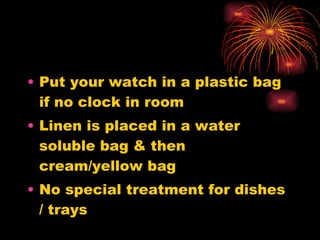
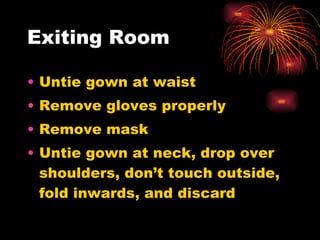
The document discusses various methods for preventing the spread of infection, including isolation procedures and barrier precautions. It outlines different types of isolation like standard precautions, droplet precautions, and airborne precautions. Guidelines are provided for setting up isolation rooms and properly donning and doffing personal protective equipment. Sterile technique and various methods for sterilizing medical equipment are also summarized.