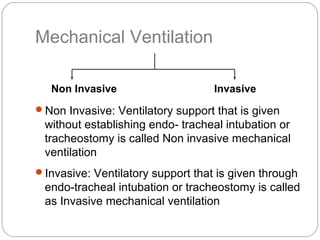
The document outlines the principles, goals, and indications for mechanical ventilation, including methods of invasive and non-invasive ventilation. It details various ventilator settings, modes of operation, and complications associated with mechanical ventilation. Additionally, the document provides information on weaning criteria and procedures for patients requiring respiratory support.