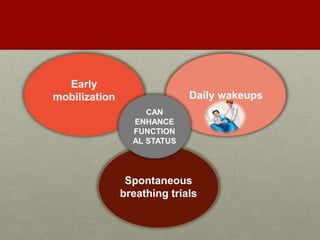
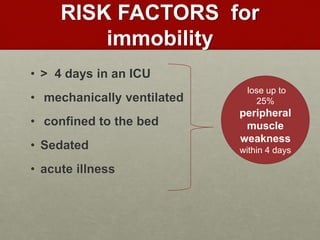
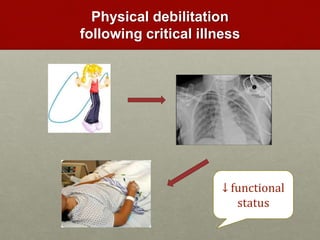
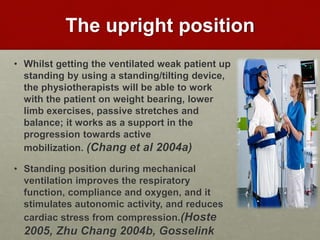
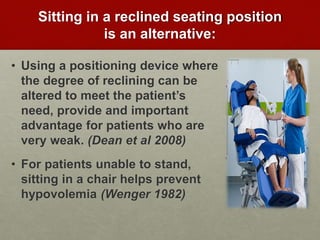
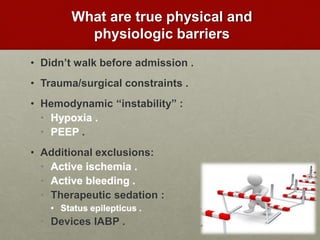
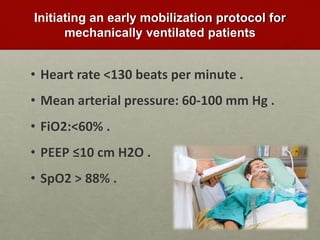
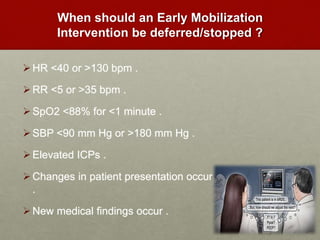
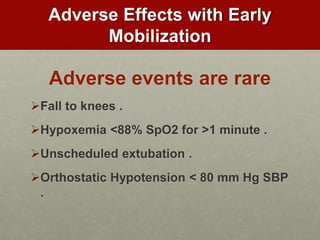
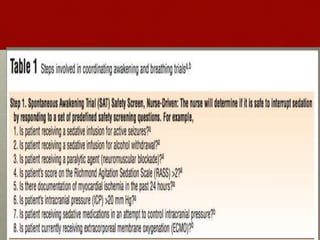
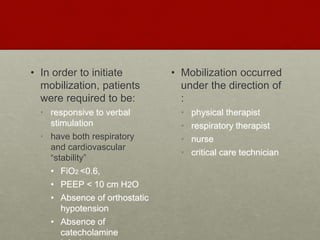
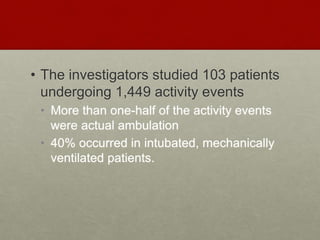
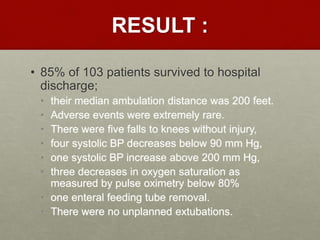
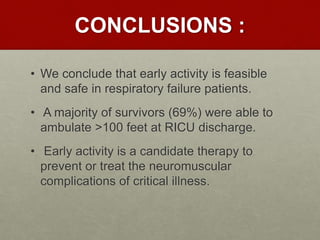
This document discusses the benefits of early mobilization for mechanically ventilated patients in the ICU. Prolonged bed rest can lead to increased morbidity, mortality, costs, and length of stay. Early mobilization, which involves getting patients sitting up and out of bed when minimally able, provides several benefits like improving respiratory function and reducing adverse effects of immobility. Two studies presented found that early mobilization was feasible and safe for respiratory failure patients, with adverse events being rare. Transferring patients to an ICU that prioritizes early activity was also found to substantially improve patient ambulation levels.