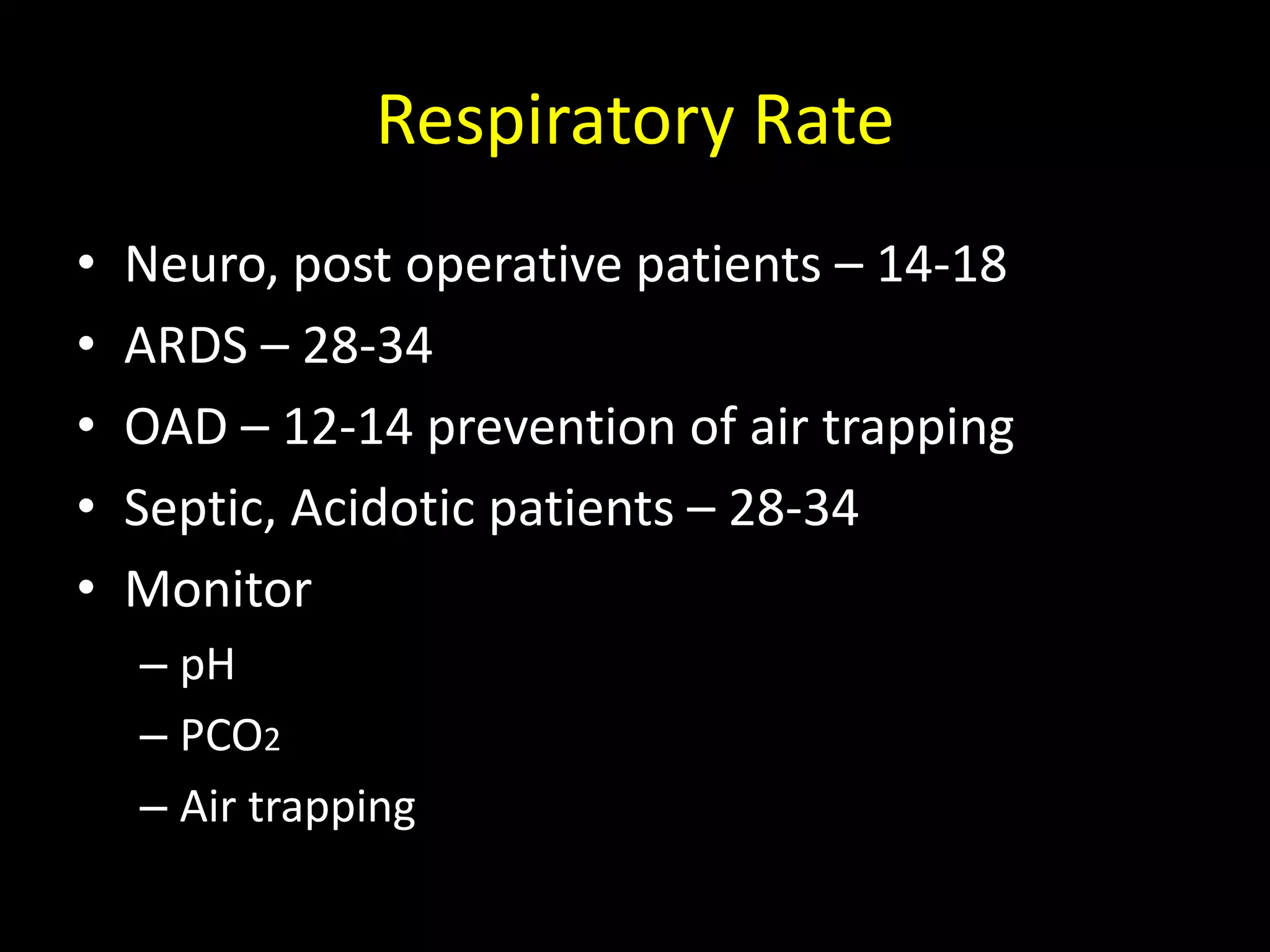
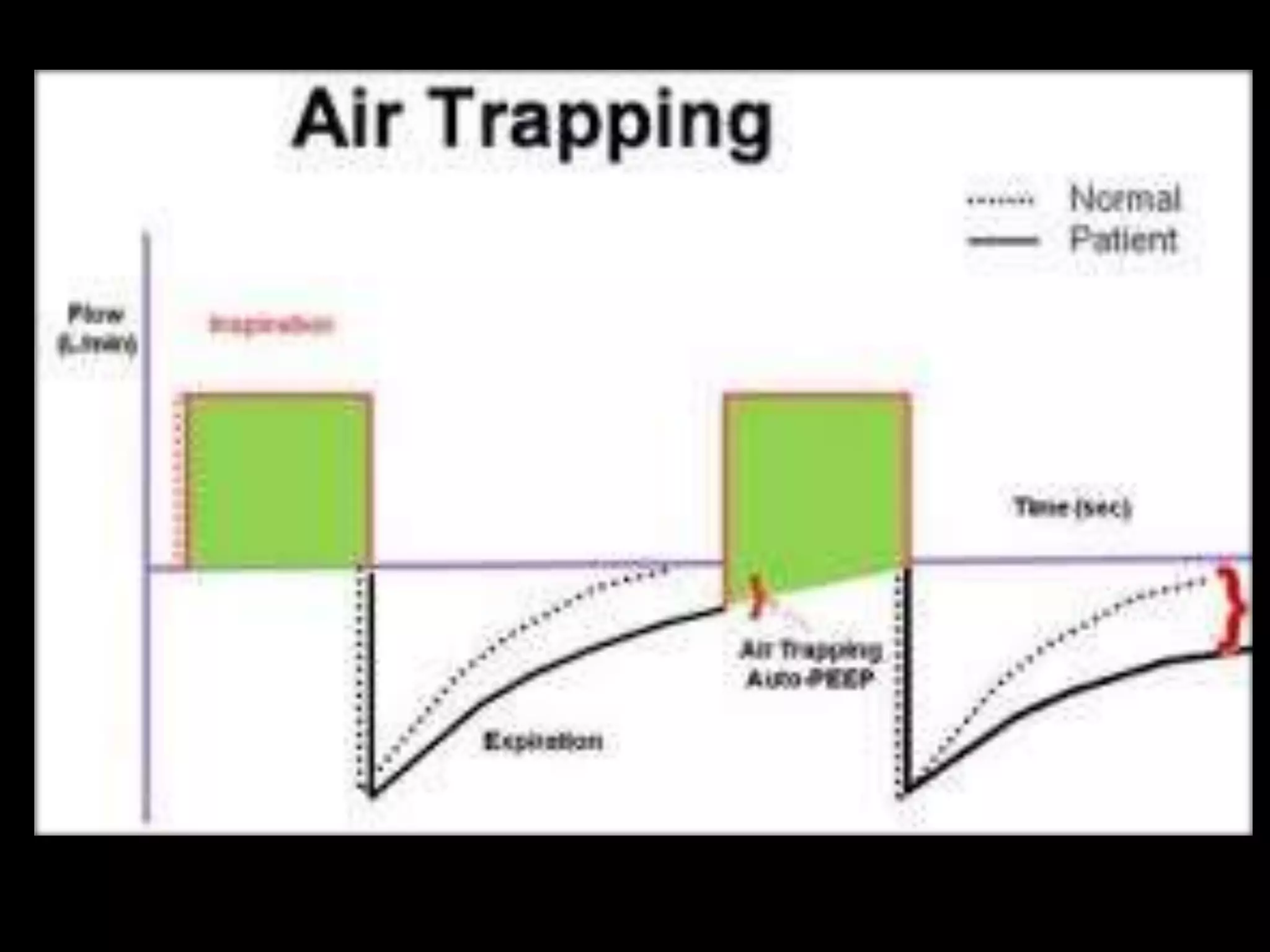
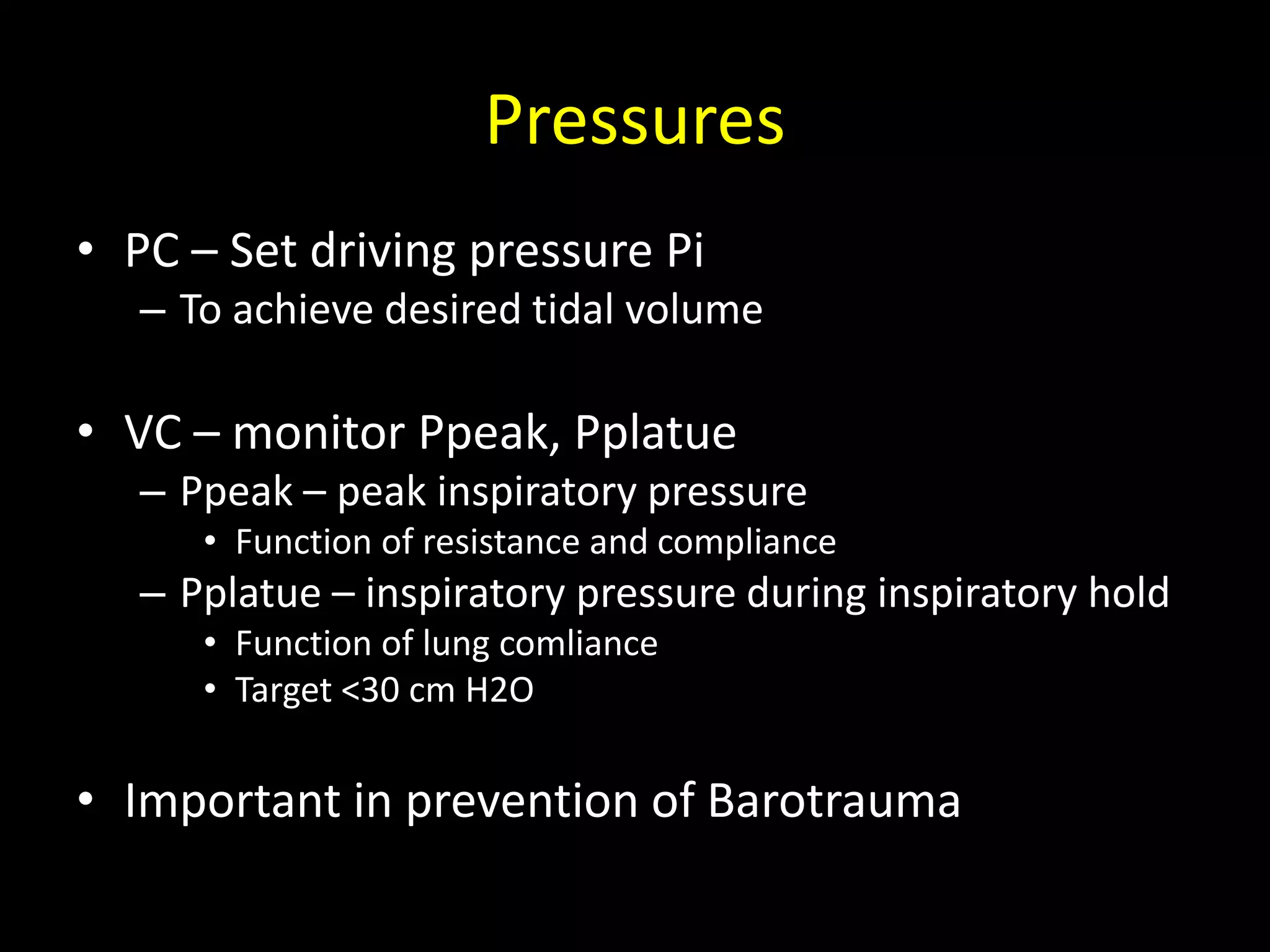
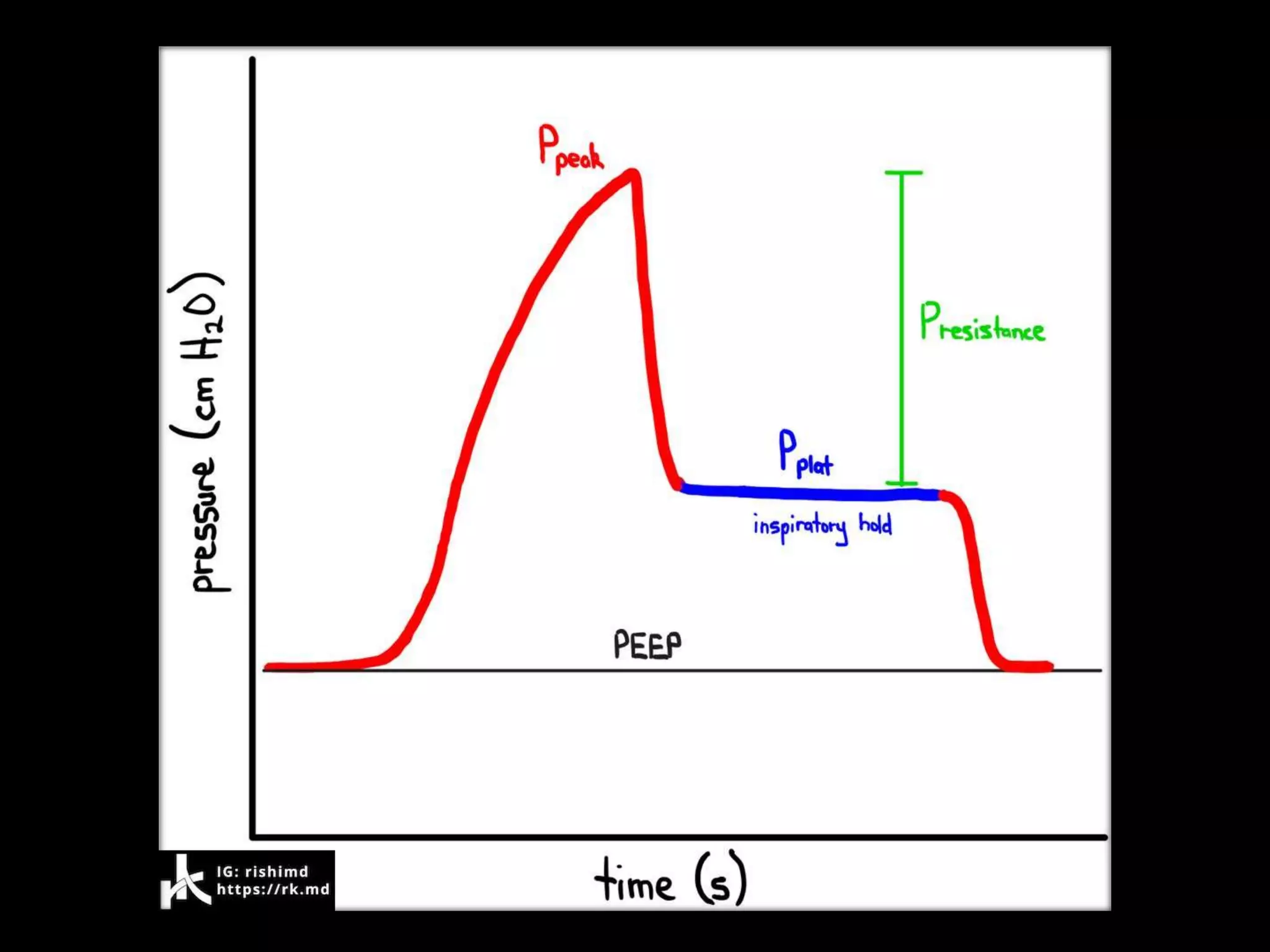
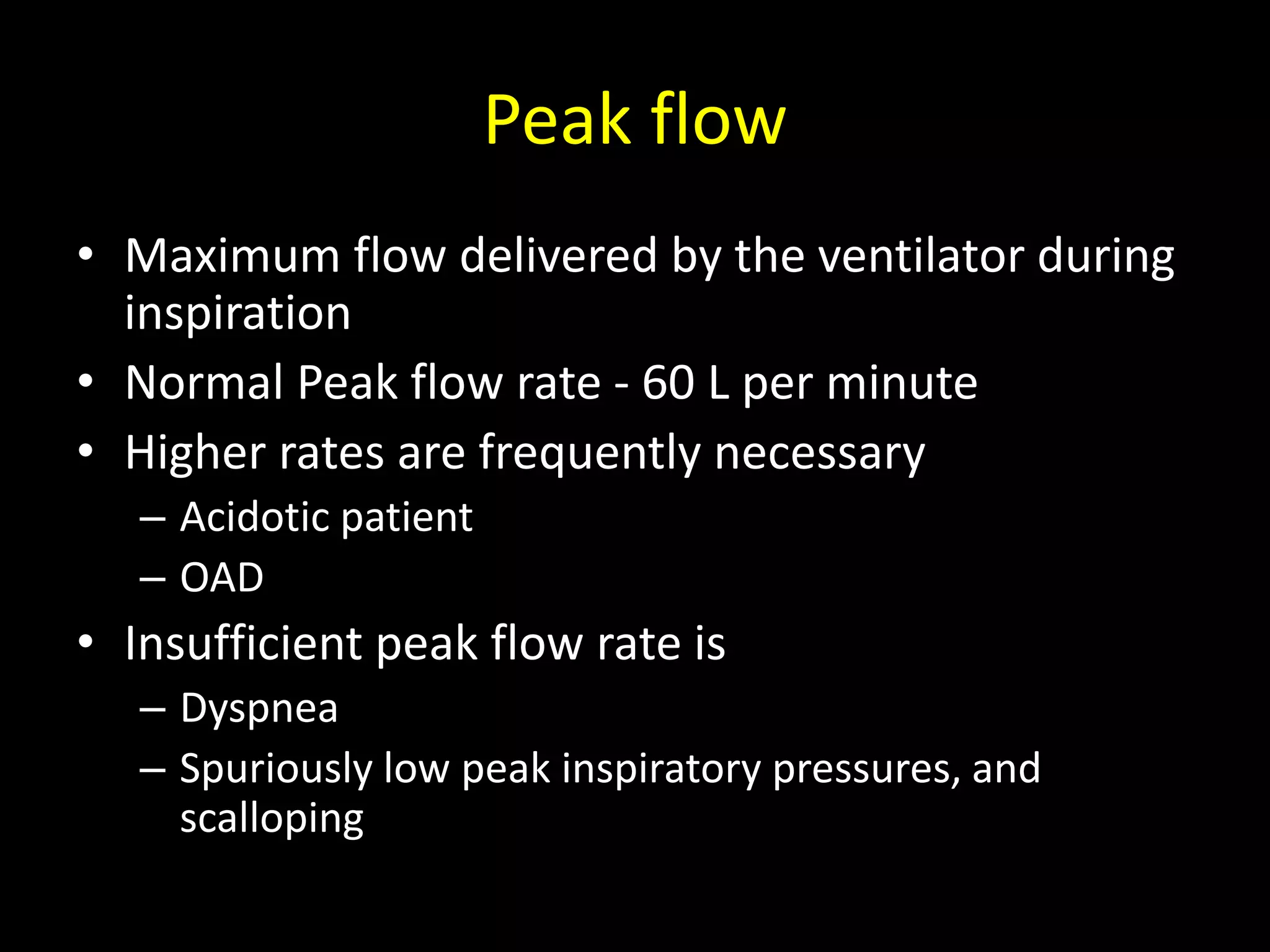
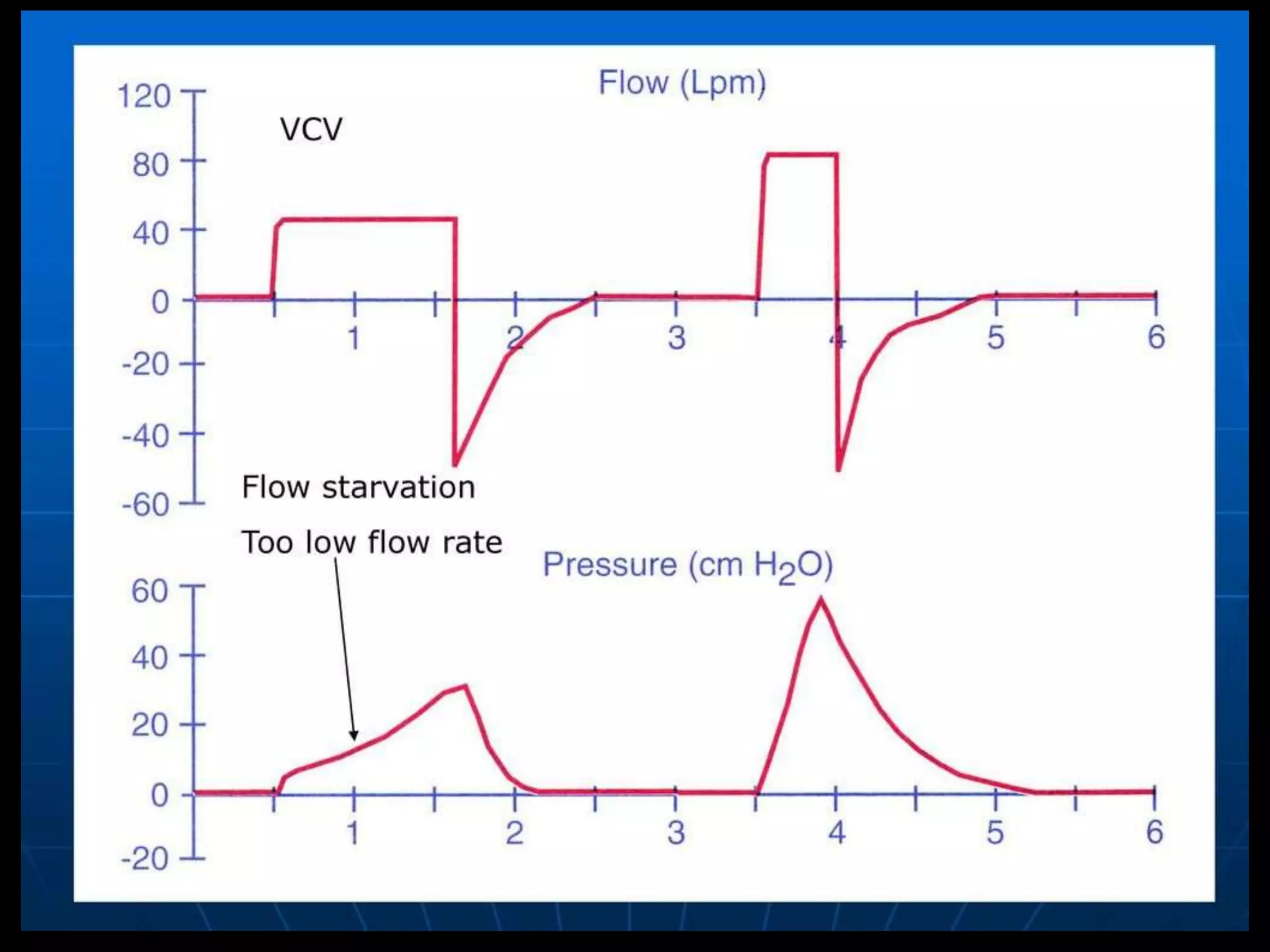
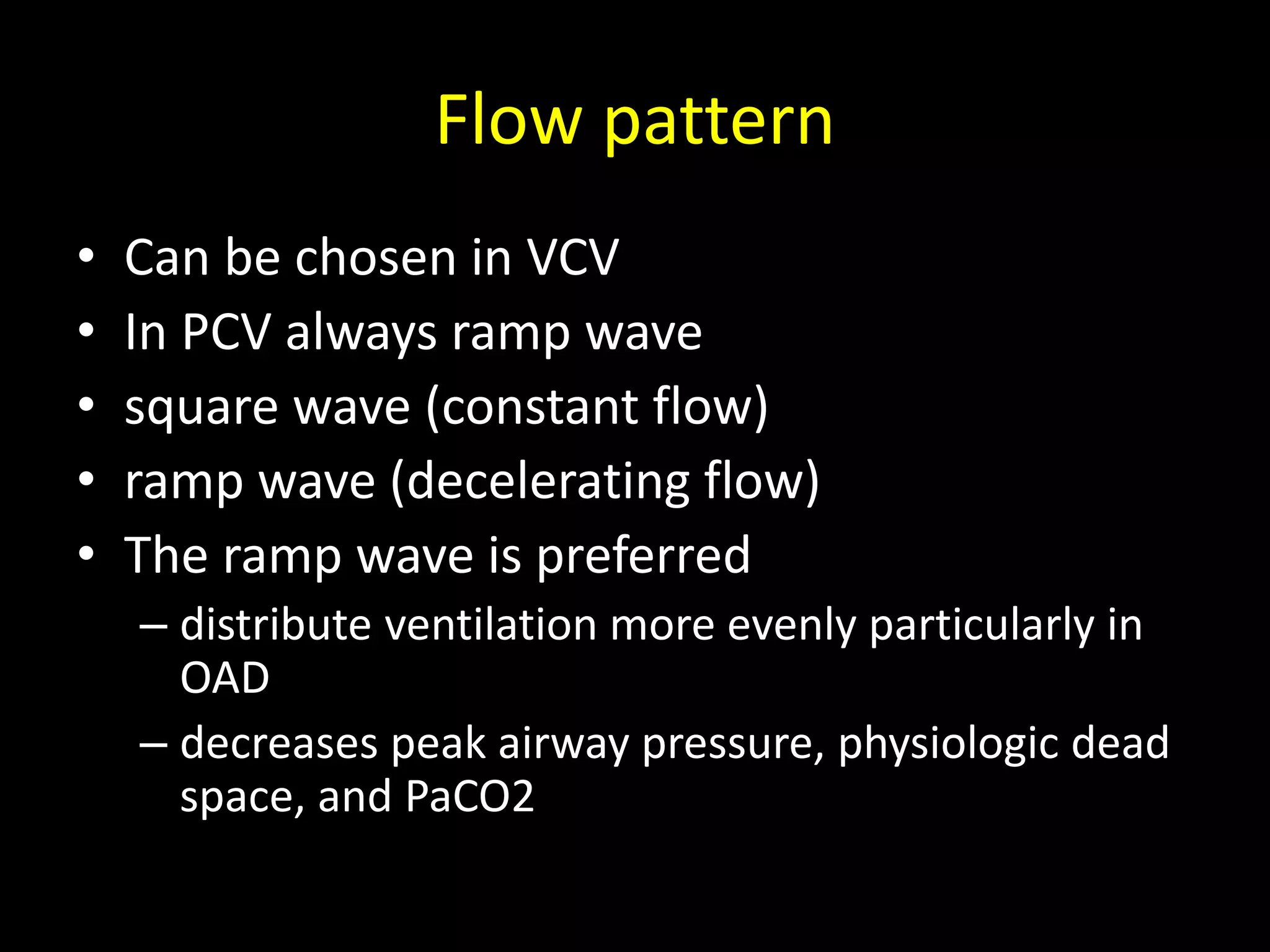
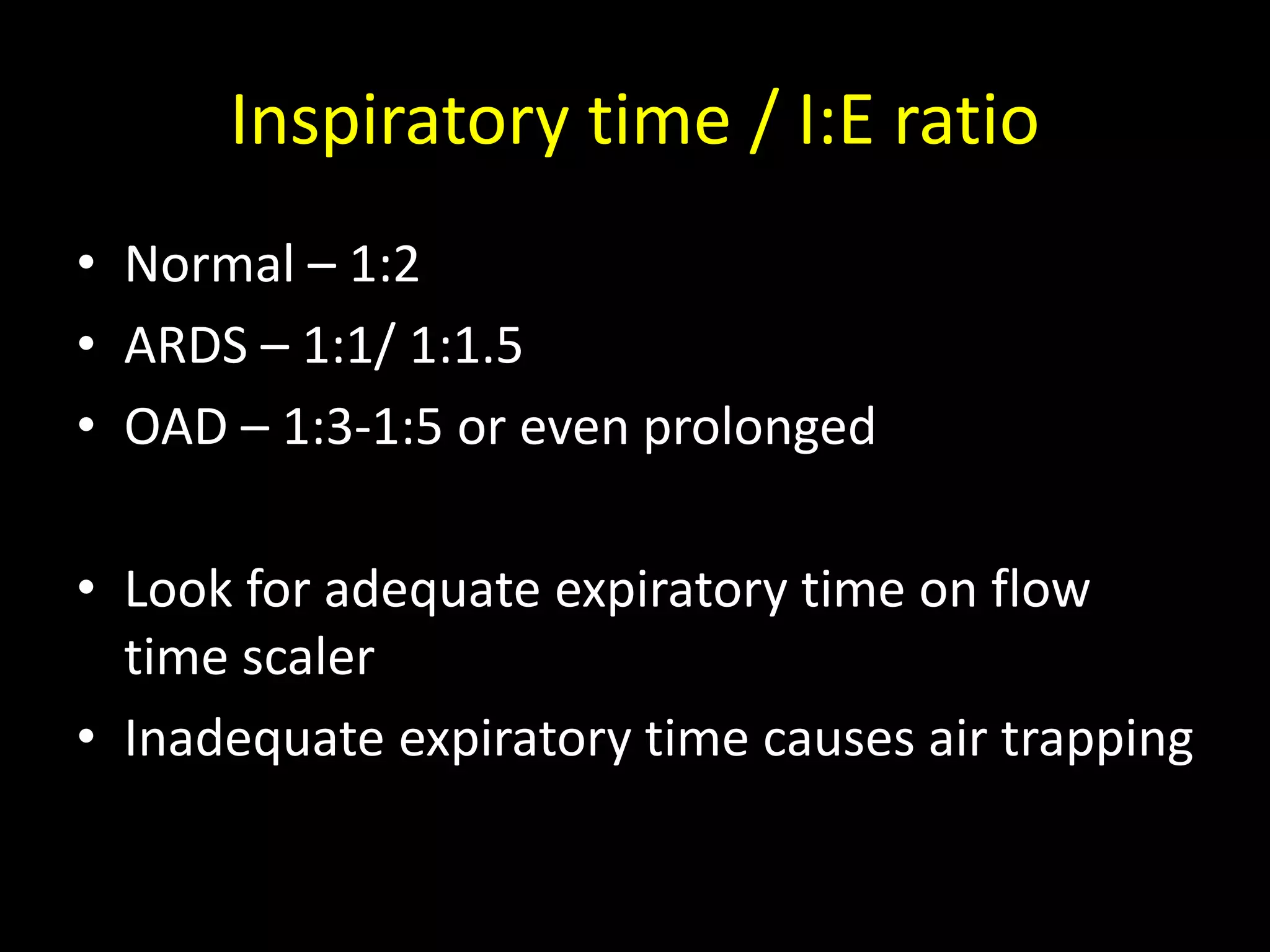
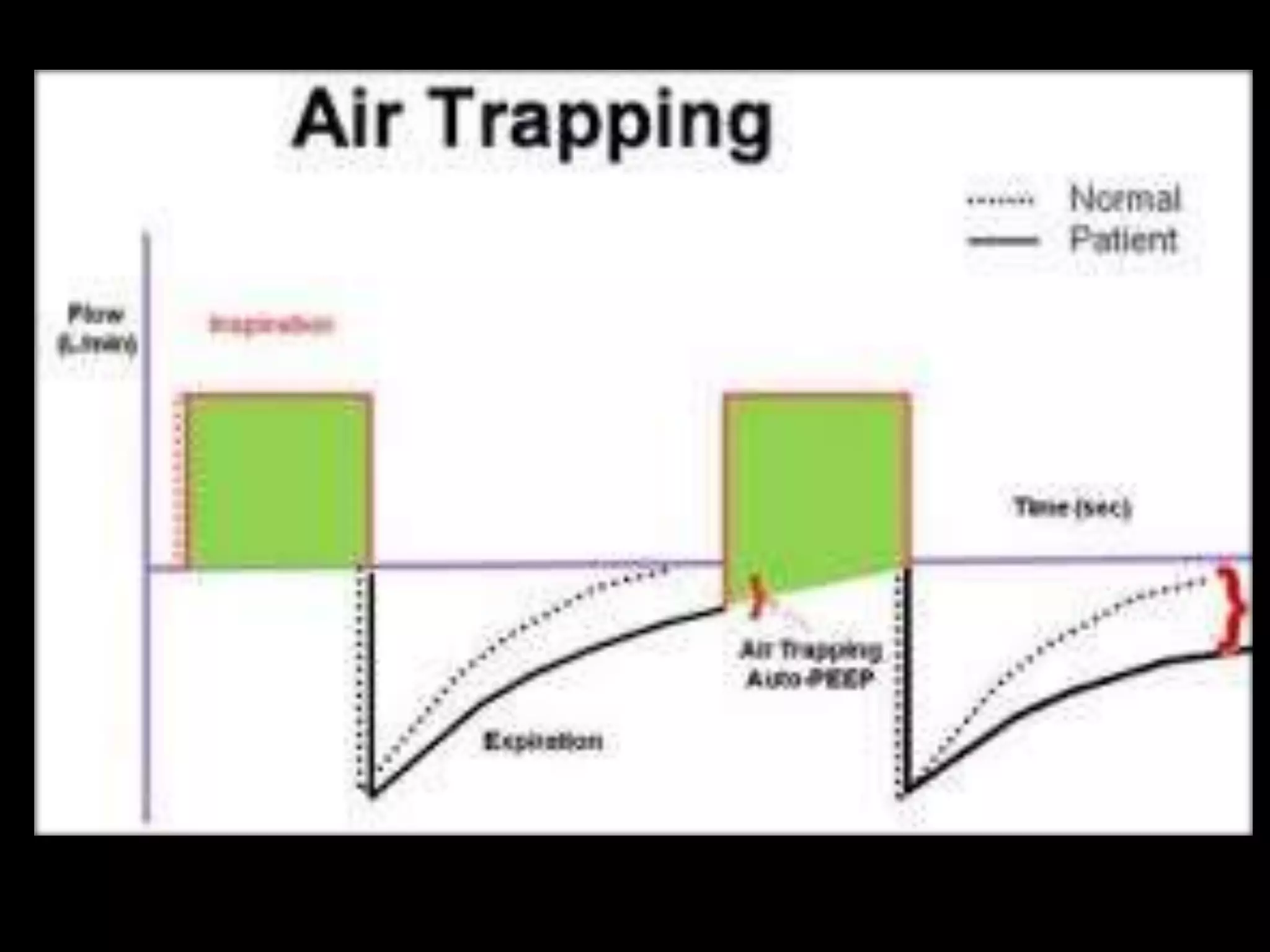
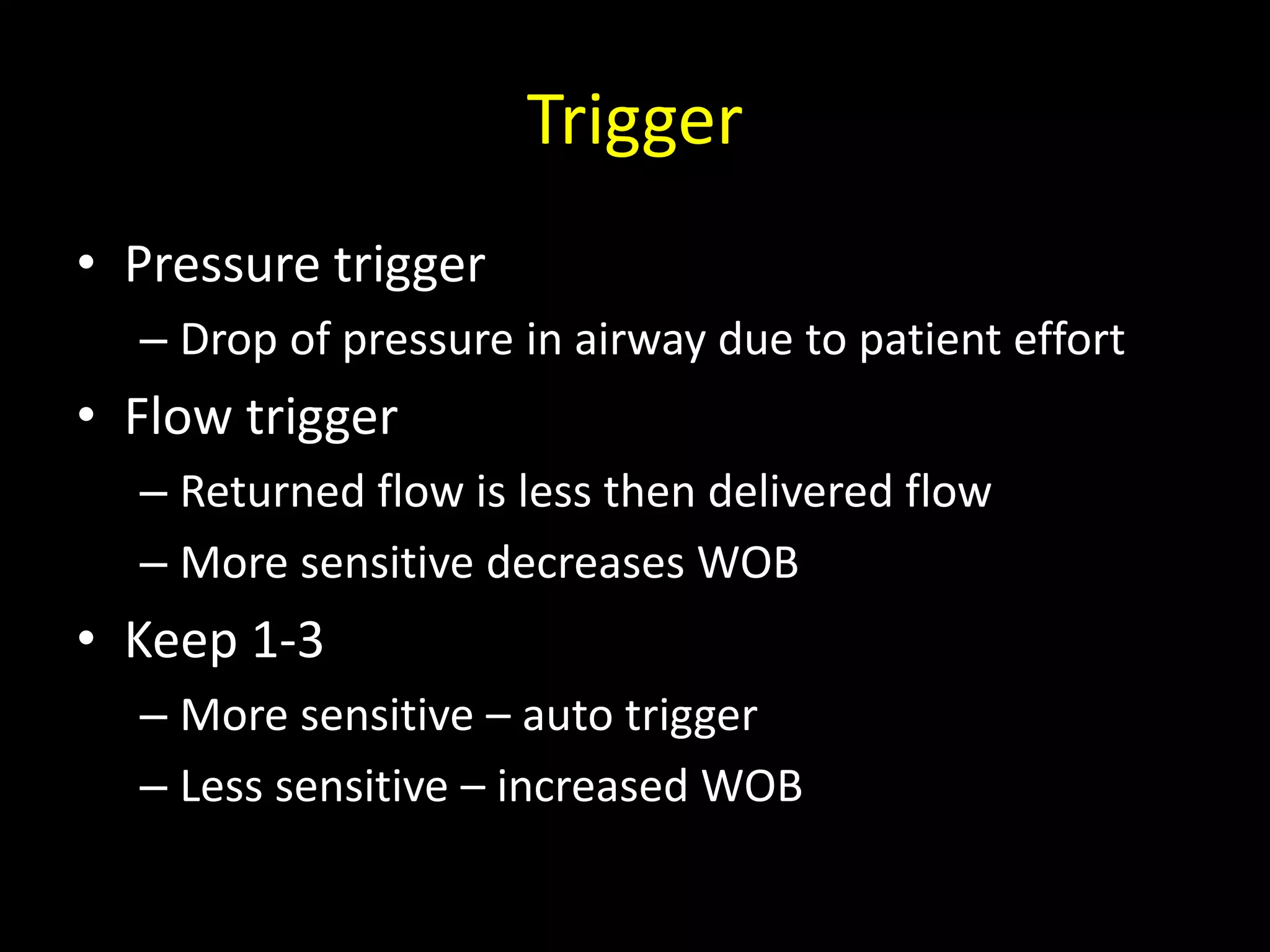
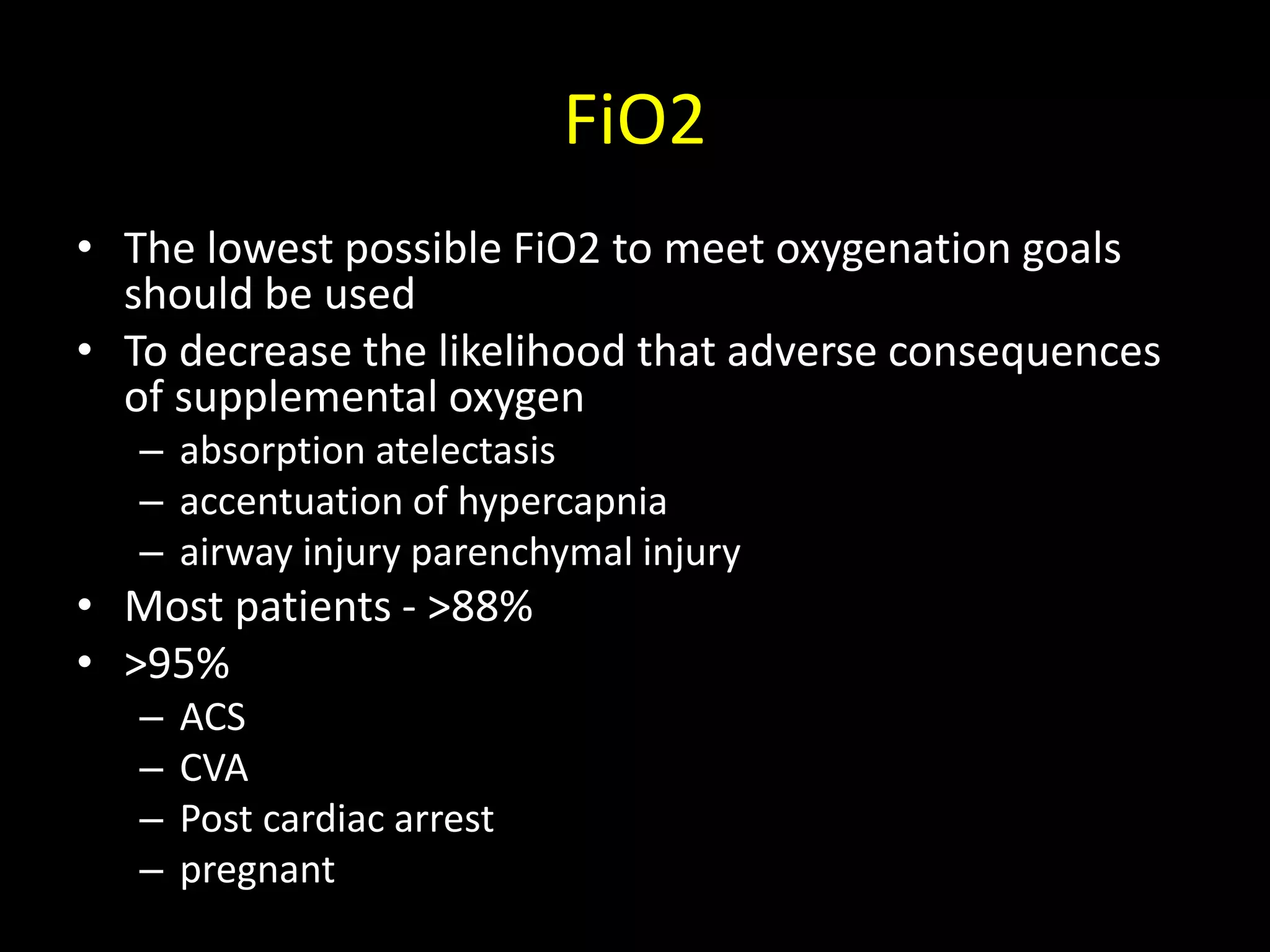
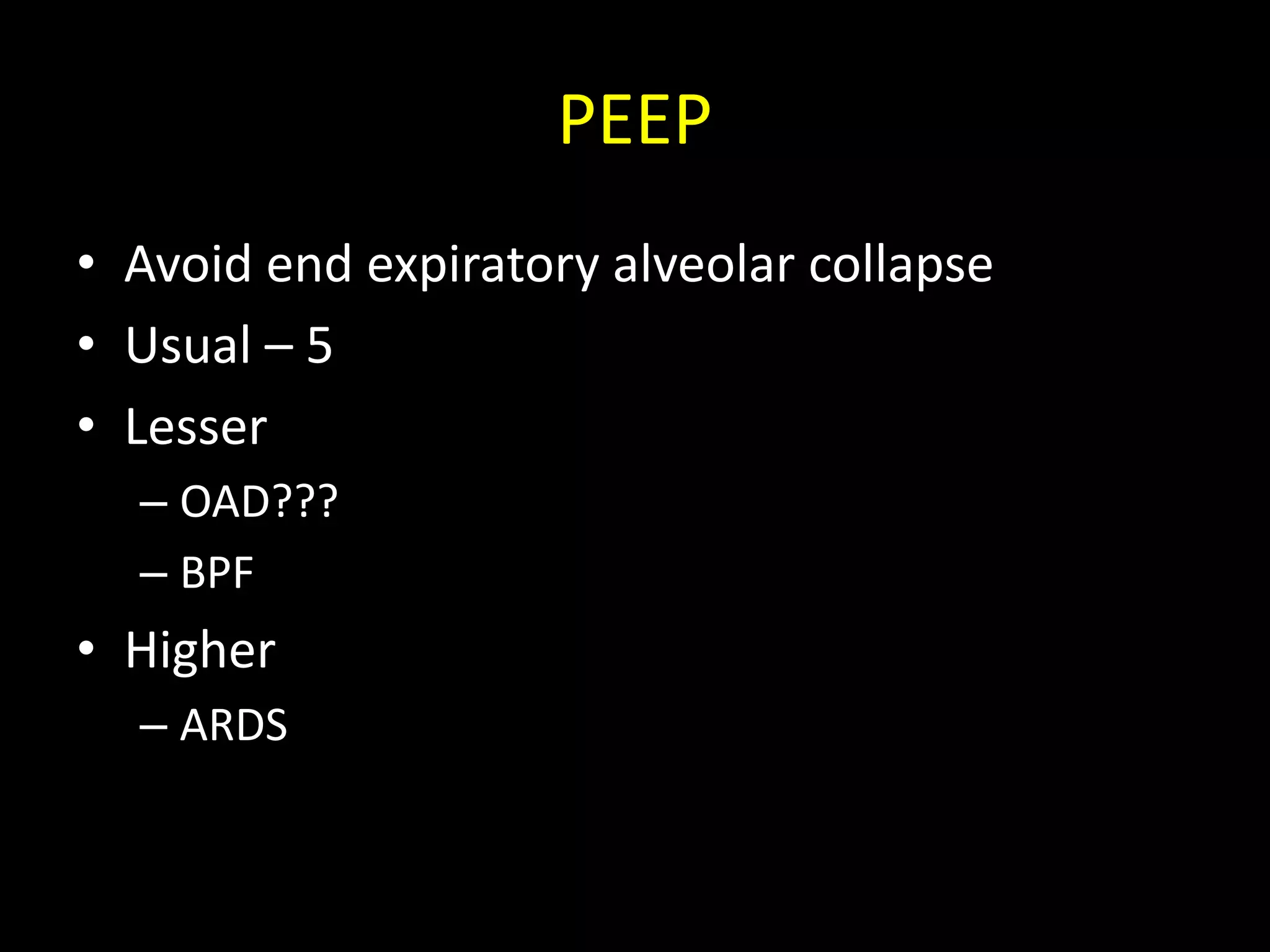
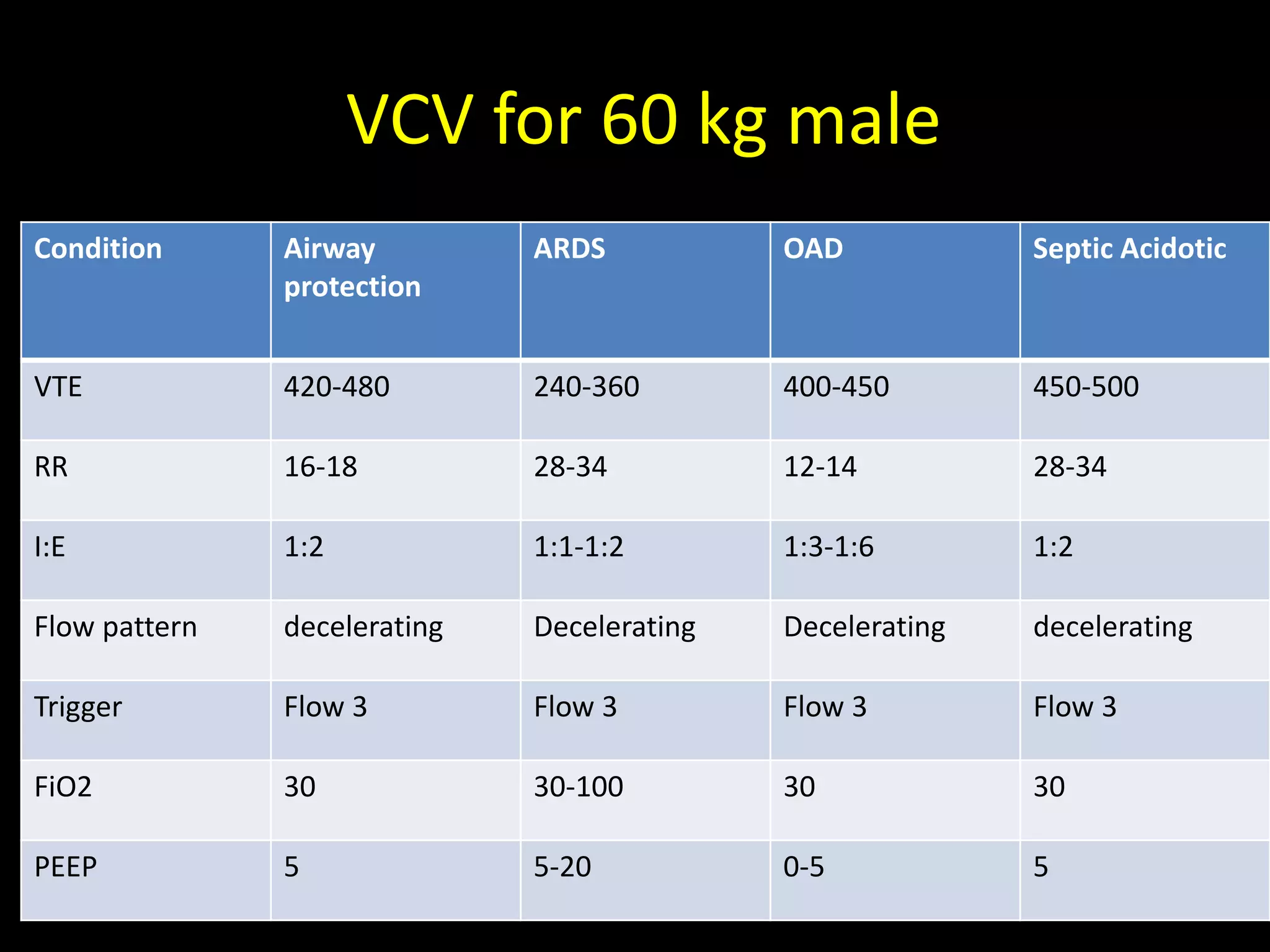
The document outlines key ventilatory parameters essential for achieving desired minute ventilation and adequate gas exchange while minimizing lung injury. It details basic parameters such as tidal volume, respiratory rate, and peak pressures, along with specific guidelines for different patient conditions like ARDS and OAD. Monitoring strategies and adjustments are emphasized to optimize ventilatory support and prevent complications.