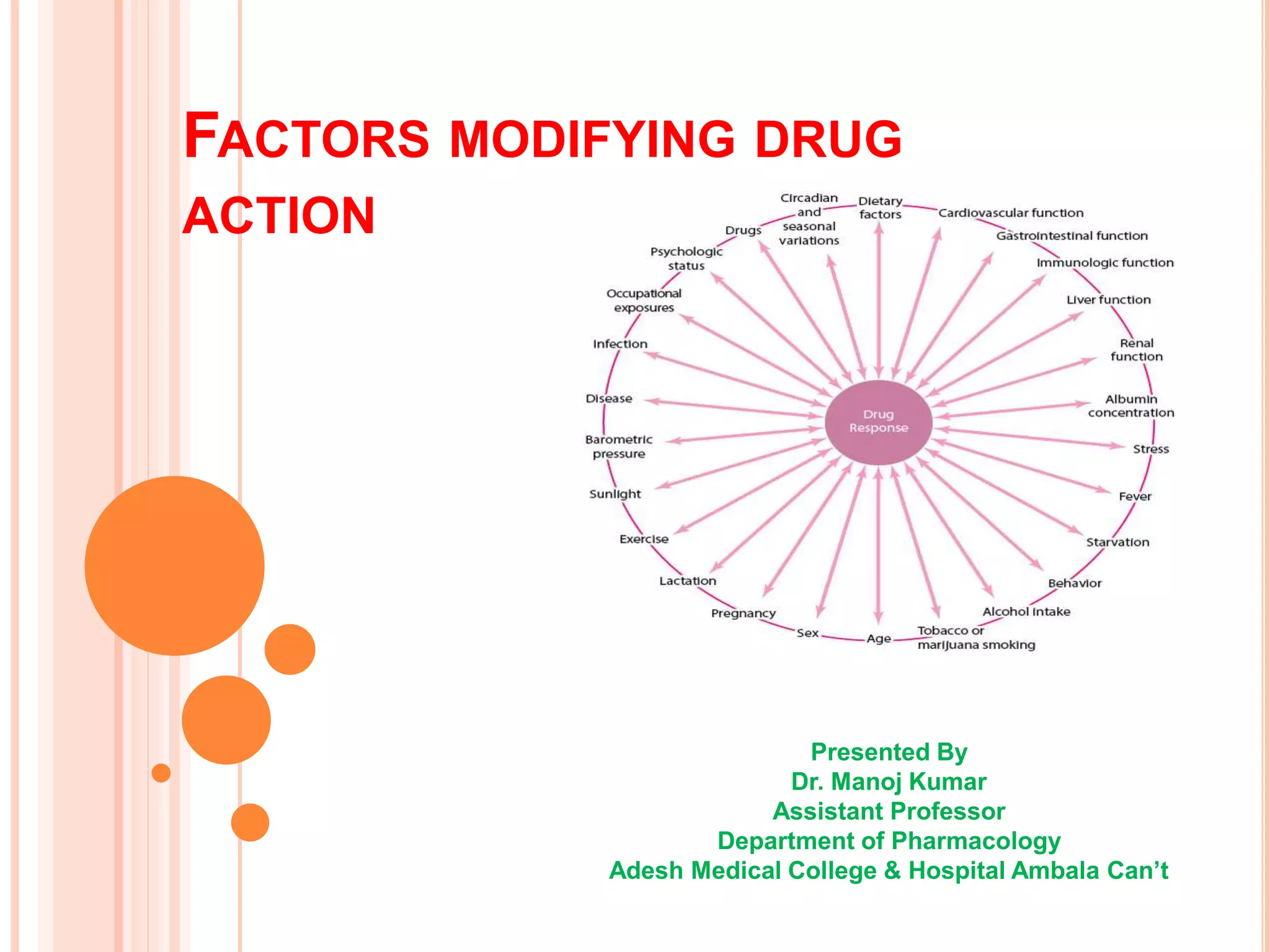
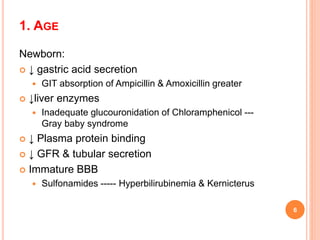
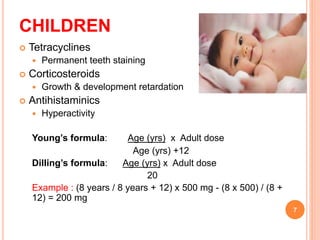
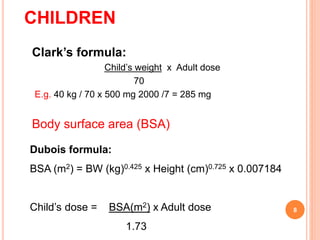
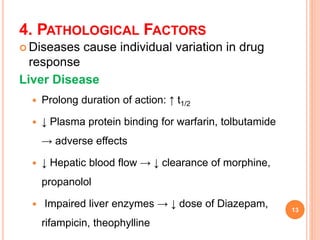
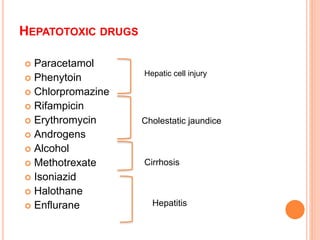
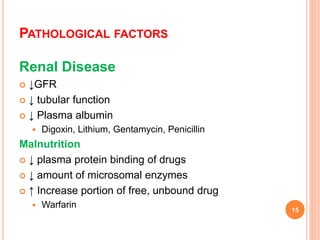
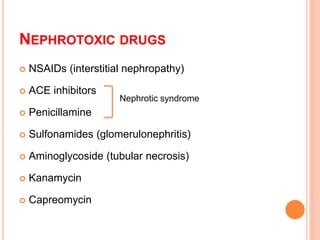
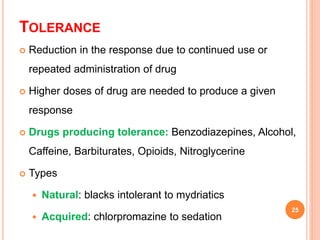
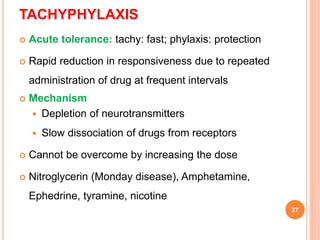
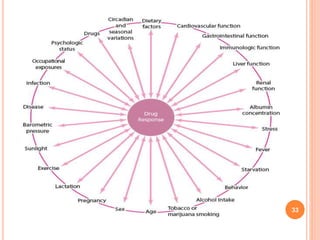
The document discusses various factors that can modify the effects of drugs in the human body. It identifies physiological factors like age, gender, pregnancy, disease states, and food intake that can impact drug pharmacokinetics and response. Genetic differences, environmental exposures, psychological states, drug interactions, and the development of tolerance are also outlined as factors modifying drug action. The document provides examples of how each factor can quantitatively or qualitatively change the expected response to a drug in a patient.